北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (6): 1049-1054. doi: 10.19723/j.issn.1671-167X.2021.06.007
类风湿关节炎初治患者颈椎失稳情况及临床特征
张璐1,胡小红2,陈澄1,蔡月明1,王庆文1,赵金霞3,△( )
)
- 1.北京大学深圳医院风湿免疫科,广东深圳 518036
2.北京大学深圳医院影像科,广东深圳 518036
3.北京大学第三医院风湿免疫科,北京 100191
Analysis of cervical instability and clinical characteristics in treatment-naive rheumatoid arthritis patients
ZHANG Lu1,HU Xiao-hong2,CHEN Cheng1,CAI Yue-ming1,WANG Qing-wen1,ZHAO Jin-xia3,△( )
)
- 1. Department of Rheumatology & Immunology, Shenzhen 518036, Guangdong, China
2. Department of medical imaging, Peking University Shenzhen Hospital, Shenzhen 518036, Guangdong, China
3. Department of Rheumatology & Immunology, Peking University Third Hospital, Beijing 100191, China
摘要:
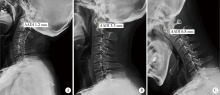
目的:研究初治类风湿关节炎(rheumatoid arthritis, RA)患者合并颈椎失稳者占比情况以及临床特征,并与经治RA患者颈椎失稳的发生情况及临床特点进行比较。方法:纳入2015年8月至2019年10月北京大学深圳医院和北京大学第三医院风湿免疫科住院期间行颈椎X线检查且有临床用药记录的RA患者,收集包括颈部症状等临床表现和实验室资料以及颈椎影像学资料进行分析。统计初治RA患者颈椎失稳人群的构成比,比较有无颈椎失稳两组初治RA患者的临床资料,比较初治及经治RA患者的颈椎失稳情况和临床特点。结果:408例RA患者中初治患者105例,女性87例,占82.9%,患者平均年龄(52±14)岁,病程中位数24个月,最短2周,最长30年。28.6%(30/105)合并颈椎失稳,其中病程≤24个月的初治RA颈椎失稳的发生率达13.6%。颈椎失稳组和无颈椎失稳组患者的颈部相关症状差异无统计学意义,与未合并颈椎失稳患者相比,颈椎失稳患者病程更长[60(18,180)个月vs. 16(8,51)个月],更多合并外周关节畸形(63.3%vs. 21.3%),血红蛋白水平较低 [(106.90±21.61) g/L vs. (115.77±14.69) g/L],经治及初治RA患者颈椎失稳构成比差异无统计学意义。合并颈椎失稳RA患者中,初治RA患者除病程更短[120.0 (72.0, 240.0)个月vs. 60.0 (27.0, 167.5)个月]外,各类型构成情况与经治RA患者差异无统计学意义。结论:初治RA患者颈椎失稳发生率较高,与经治RA患者颈椎失稳发生率相似,病程小于24个月的早期初治RA患者中已有相当比例合并颈椎失稳;颈部相关症状在初治RA患者合并颈椎失稳人群中并无明显特异性;对具有病程长、外周关节畸形比例高及血红蛋白水平低临床特点的初治RA患者应注意排查颈椎失稳。
中图分类号:
- R593.22
| [1] | Yang SY, Boniello AJ, Poorman CE, et al. A review of the diagnosis and treatment of atlantoaxial dislocations[J]. Global Spine, 2014, 4(3):197-210. |
| [2] |
Olinger CR, Bransford R. Upper cervical trauma[J]. Orthop Clin North Am, 2021, 52(4):451-479.
doi: 10.1016/j.ocl.2021.05.013 |
| [3] |
Hedequist D, Bekelis K, Emans J, et al. Single stage reduction and stabilization of basilar invagination after failed prior fusion surgery in children with Down’s syndrome[J]. Spine (Phila Pa 1976), 2010, 35(4):E128-133.
doi: 10.1097/BRS.0b013e3181bad0c2 |
| [4] | 张璐, 刘湘源. 不可忽视类风湿关节炎的颈椎受累[J]. 中华风湿病学杂志, 2015, 19(4):217-218. |
| [5] | 张璐, 胡小红, 王庆文, 等. 类风湿关节炎合并颈椎失稳的人群分布及临床特征[J]. 北京大学学报(医学版), 2020, 52(6):50-55. |
| [6] |
Bodakçi E, Üsküdar CD, Ertürk A, et al. Can neck pain be an initial symptom of rheumatoid arthritis? A case report and literature review[J]. Rheumatol Int, 2018, 38(5):925-931.
doi: 10.1007/s00296-018-4019-z pmid: 29589114 |
| [7] |
Baek IW, Joo YB, Park KS, et al. Risk factors for cervical spine instability in patients with rheumatoid arthritis[J]. Clin Rheumatol, 2021, 40(2):547-555.
doi: 10.1007/s10067-020-05243-9 |
| [8] |
Mori Y, Izumiyama T, Baba K, et al. Evaluation of risk factors of vertebral fracture in Japanese female patients with glucocorticoid-induced osteoporosis[J]. J Orthop Surg Res, 2020, 15(1):290.
doi: 10.1186/s13018-020-01813-4 pmid: 32727595 |
| [9] |
Sandström T, Rantalaiho V, Yli-Kerttula T, et al. Cervical spine involvement among patients with rheumatoid arthritis treated actively with treat-to-target strategy: 10-year results of the NEO-RACo study[J]. J Rheumatol, 2020. 47(8):1160-1164.
doi: 10.3899/jrheum.190139 pmid: 31732558 |
| [10] |
Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative[J]. Ann Rheum Dis, 2010, 69(9):1580-1588.
doi: 10.1136/ard.2010.138461 pmid: 20699241 |
| [11] | Joaquim AF, Ghizoni E, Tedeschi H, et al. Radiological evaluation of cervical spine involvement in rheumatoid arthritis[J]. Neurosurg Focus, 2015, 38(4):E4. |
| [12] |
Shlobin NA, Dahdaleh NS. Cervical spine manifestations of rheumatoid arthritis: A review[J]. Neurosurg Rev, 2021, 44(4):1957-1965.
doi: 10.1007/s10143-020-01412-1 |
| [13] |
Drosos AA, Pelechas E, Voulgari PV. Radiological findings of the cervical spine in rheumatoid arthritis: What a rheumatologist should know[J]. Curr Rheumatol Rep, 2020, 22(6):19.
doi: 10.1007/s11926-020-00894-8 |
| [14] |
Zhang T, Pope J. Cervical spine involvement in rheumatoid arthritis over time: Results from a meta-analysis[J]. Arthritis Res Ther, 2015, 17(1):148.
doi: 10.1186/s13075-015-0643-0 |
| [15] | Mańczak M, Gasik R. Cervical spine instability in the course of rheumatoid arthritis-imaging methods[J]. Reumatologia, 2017, 55(4):201-207. |
| [16] |
Zhu S, Xu W, Luo Y, et al. Cervical spine involvement risk factors in rheumatoid arthritis: A meta-analysis[J]. Int J Rheum Dis, 2017, 20(5):541-549.
doi: 10.1111/apl.2017.20.issue-5 |
| [17] |
Na MK, Chun HJ, Bak KH, et al. Risk factors for the development and progression of atlantoaxial subluxation in surgically treated rheumatoid arthritis patients, considering the time interval between rheumatoid arthritis diagnosis and surgery[J]. J Korean Neurosurg Soc, 2016, 59(6):590-596.
doi: 10.3340/jkns.2016.59.6.590 |
| [18] |
Möller B, Everts-graber J, Florentinus S, et al. Low hemoglobin and radiographic damage progression in early rheumatoid arthritis: secondary analysis from a phase Ⅲ trial[J]. Arthritis Care Res (Hoboken), 2018, 70(6):861-868.
doi: 10.1002/acr.v70.6 |
| [1] | 刘东武, 陈杰, 高明利, 于静. 类风湿关节炎伴发淋巴结Castleman样病理改变1例[J]. 北京大学学报(医学版), 2024, 56(5): 928-931. |
| [2] | 黄会娜,赵静,赵祥格,白自然,李霞,王冠. 乳酸对类风湿关节炎患者外周血CD4+T细胞亚群的调控作用[J]. 北京大学学报(医学版), 2024, 56(3): 519-525. |
| [3] | 汤晓菲,李永红,丁秋玲,孙卓,张阳,王育梅,田美伊,刘坚. 类风湿关节炎患者下肢深静脉血栓发病率及危险因素[J]. 北京大学学报(医学版), 2024, 56(2): 279-283. |
| [4] | 邹雪,白小娟,张丽卿. 艾拉莫德联合托法替布治疗难治性中重度类风湿关节炎的疗效[J]. 北京大学学报(医学版), 2023, 55(6): 1013-1021. |
| [5] | 吴琦,蔡月明,何娟,黄文蒂,王庆文. 血脂异常与类风湿关节炎肺间质病变的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 982-992. |
| [6] | 张警丰,金银姬,魏慧,姚中强,赵金霞. 体重指数与类风湿关节炎临床特征的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 993-999. |
| [7] | 金银姬,孙琳,赵金霞,刘湘源. 血清IgA型抗鼠科肉瘤病毒癌基因同源物B1抗体在类风湿关节炎中的意义[J]. 北京大学学报(医学版), 2023, 55(4): 631-635. |
| [8] | 蔡文心,李仕成,刘一鸣,梁如玉,李静,郭建萍,胡凡磊,孙晓麟,李春,刘栩,叶华,邓立宗,李茹,栗占国. 类风湿关节炎临床分层及其特征的横断面研究[J]. 北京大学学报(医学版), 2022, 54(6): 1068-1073. |
| [9] | 程昉,杨邵英,房星星,王璇,赵福涛. CCL28-CCR10通路在类风湿关节炎单核细胞迁移中的作用[J]. 北京大学学报(医学版), 2022, 54(6): 1074-1078. |
| [10] | 刘蕊,赵金霞,闫良. 类风湿关节炎合并下肢静脉血栓患者的临床特点[J]. 北京大学学报(医学版), 2022, 54(6): 1079-1085. |
| [11] | 张警丰,金银姬,魏慧,姚中强,赵金霞. 类风湿关节炎患者生活质量与疾病活动度的横断面研究[J]. 北京大学学报(医学版), 2022, 54(6): 1086-1093. |
| [12] | 高超,陈立红,王莉,姚鸿,黄晓玮,贾语博,刘田. 类风湿关节炎合并纤维肌痛简易分类标准的临床验证[J]. 北京大学学报(医学版), 2022, 54(2): 278-282. |
| [13] | 娄雪,廖莉,李兴珺,王楠,刘爽,崔若玫,徐健. 类风湿关节炎患者外周血TWEAK基因启动子区甲基化状态及其表达[J]. 北京大学学报(医学版), 2021, 53(6): 1020-1025. |
| [14] | 钟华,徐丽玲,白明欣,苏茵. 类风湿关节炎患者趋化因子CXCL9和CXCL10在骨侵蚀中的作用[J]. 北京大学学报(医学版), 2021, 53(6): 1026-1031. |
| [15] | 罗靓,霍文岗,张钦,李春. 类风湿关节炎合并角膜溃疡的临床特点和相关因素分析[J]. 北京大学学报(医学版), 2021, 53(6): 1032-1036. |
|
||