北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (2): 315-319. doi: 10.19723/j.issn.1671-167X.2022.02.019
经锁孔入路显微外科切除腰椎管肿瘤54例临床研究
- 北京大学第三医院神经外科,北京 100191
Microscopic resection of lumbar intraspinal tumor through keyhole approach: A clinical study of 54 cases
LIN Guo-zhong,MA Chang-cheng( ),WU Chao,SI Yu
),WU Chao,SI Yu
- Department of Neurosurgery, Peking University Third Hospital, Beijing 100191, China
摘要:
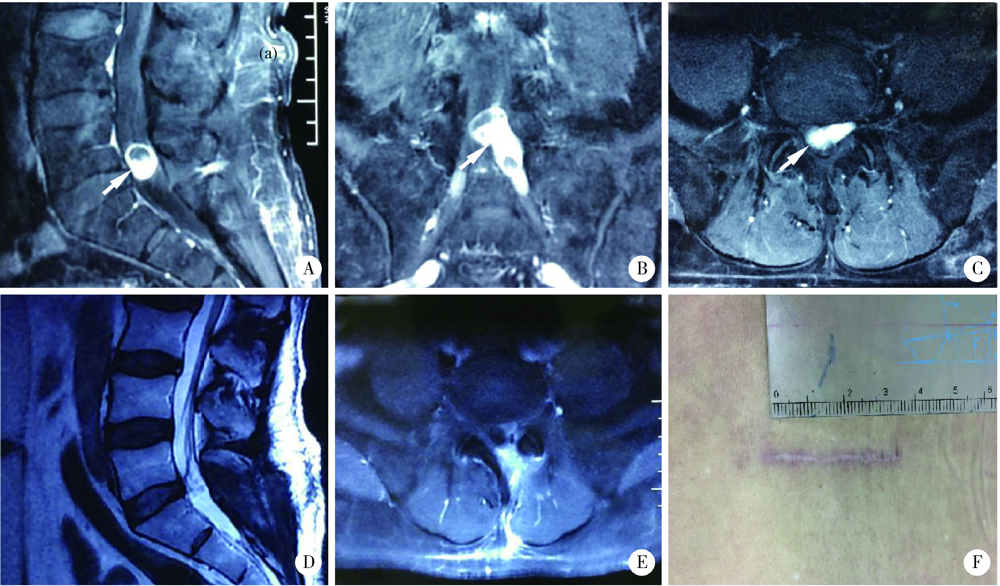
目的: 探讨经微通道锁孔显微手术切除腰椎管肿瘤的可行性和关键技术。方法: 回顾性分析2017年2月至2019年9月纳入研究的54例腰椎管肿瘤患者的临床资料,包括硬膜外肿瘤8例,硬膜内外肿瘤3例,髓外硬膜下肿瘤43例(脊髓圆锥腹侧肿瘤3例),肿瘤长径0.5~3.0 cm。患者的临床症状包括:相应神经支配区疼痛49例,肿瘤所在节段及以下感觉障碍(麻木)5例,肢体无力7例,大小便功能障碍2例。患者均采用显微镜下微通道锁孔技术进行手术。结果: 微通道下半椎板切除37例,半侧椎板间开窗14例,半椎板切除或半侧椎板间开窗+小关节内侧1/4切除3例,所有患者的肿瘤均得以全切除。手术时间75~135 min,平均93.3 min;术后住院时间4~7 d,平均5.7 d。术后组织病理检查结果为神经鞘瘤34例,脊膜瘤4例,室管膜瘤9例,肠源性囊肿1例,畸胎瘤/皮样囊肿/表皮样囊肿5例,副神经节瘤1例。所有患者术后无感染,无脑脊液漏,4例患者出现相应神经支配区的麻木感,1例患者出现排尿困难,其余患者无神经功能障碍加重。术后随访3~33个月,平均14.4个月,5例术后症状加重的患者均恢复正常,49例术前有疼痛症状者均完全缓解,7例术前肌力减退者和2例术前大小便功能障碍者均恢复正常,5例术前感觉减退者中有4例完全恢复,1例仍残余轻度感觉减退。未见脊柱不稳定或畸形,未见肿瘤复发或残留。按McCormick分级,均为Ⅰ级。结论: 经微通道锁孔显微手术切除腰椎管肿瘤应适当选择病例,两个节段以下的腰椎管髓外肿瘤(包括部分脊髓圆锥腹侧肿瘤)通过微通道技术可Ⅰ期全切除。微通道技术有利于保留腰椎的正常结构和肌肉附着,有利于保持腰椎的完整性及稳定性。
中图分类号:
- R739.4
| [1] | 林国中, 马长城, 吴超. 显微镜下微通道锁孔技术在椎管肿物手术中的应用[J]. 中国微创外科杂志, 2019, 19(6):494-497. |
| [2] | 马长城, 王振宇. 半椎板切除入路治疗颈椎管哑铃型肿瘤[J]. 中国微创外科杂志, 2001, 1(6):336-337. |
| [3] | 吴超, 王振宇, 林国中, 等. 颈椎单侧半椎板及不同程度小关节切除术后生物力学变化的有限元分析[J]. 中华神经外科疾病研究杂志, 2018, 17(4):352-356. |
| [4] | 林国中, 王振宇, 谢京城, 等. 半椎板入路显微手术治疗颈椎椎管内肿瘤[J]. 中国临床神经外科杂志, 2010, 15(7):390-392. |
| [5] |
Zairi F, Nzokou A, Sunna T, et al. Minimally invasive costotransversectomy for the resection of large thoracic dumbbell tumors[J]. Br J Neurosurg, 2017, 31(2):179-183.
doi: 10.1080/02688697.2016.1233317 |
| [6] | Mende K, Krätzig T, Mohme M, et al. Keyhole approaches to intradural pathologies[J]. Neurosurg Focus, 2017, 43(2):E5. |
| [7] | Reisch R, Koechlin N, Marcus H. Minimally invasive keyhole approaches in spinal intradural tumor surgery: report of two cases and conceptual considerations[J]. J Neurosurg Sci, 2016, 60(3):392-397. |
| [8] | Turel MK, D’Souza WP, Rajshekhar V. Hemilaminectomy approach for intradural extramedullary spinal tumors: An analysis of 164 patients[J]. Neurosurg Focus, 2015, 39(2):E9. |
| [9] |
Kaya RA. Surgical excition of spinal intradural meningiomas through a single-sided minimally invasive approach: Key-hole laminotomy[J]. Asian Spine J, 2015, 9(2):225-231.
doi: 10.4184/asj.2015.9.2.225 |
| [10] | 林国中, 马长城, 吴超. 显微镜下微通道锁孔技术切除脊髓腹侧肿瘤[J]. 中国微创外科杂志, 2020, 20(1):52-54. |
| [11] |
Xu J, Liu C, Lin Y, et al. Microscopic minimally invasive keyhole technique for surgical resection of spinal dumbbell tumors[J]. World Neurosurg, 2018, 109:e110-e117.
doi: 10.1016/j.wneu.2017.09.114 |
| [12] | 林国中, 王振宇, 刘彬, 等. 硬膜外哑铃形神经鞘瘤的手术治疗[J]. 中国微创外科杂志, 2018, 18(9):783-786. |
| [13] | Zhuang Y, Cai G, Fu C, et al. Novel combination of paraspinal keyhole surgery with a tubular retractor system leads to significant improvements in lumbar intraspinal extramedullary schwannomas[J]. Oncol Lett, 2017, 14(6):7873-7879. |
| [14] |
Ito K, Aoyama T, Horiuchi T, et al. Utility of nonpenetrating titanium clips for dural closure during spinal surgery to prevent postoperative cerebrospinal fluid leakage[J]. J Neurosurg Spine, 2015, 23(6):812-819.
doi: 10.3171/2015.3.SPINE141215 |
| [15] | 林国中, 王振宇, 刘斌. 神经电生理监测技术在椎管内病变术中的应用[J]. 北京大学学报(医学版), 2012, 44(5):776-779. |
| [1] | 林国中,马长城,吴超,司雨,杨军. 微通道技术在颈椎管肿瘤微创切除术中的应用[J]. 北京大学学报(医学版), 2024, 56(2): 318-321. |
|
||