北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (6): 1086-1093. doi: 10.19723/j.issn.1671-167X.2022.06.005
类风湿关节炎患者生活质量与疾病活动度的横断面研究
- 北京大学第三医院风湿免疫科, 北京 100191
Cross-sectional study on quality of life and disease activity of rheumatoid arthritis patients
Jing-feng ZHANG,Yin-ji JIN,Hui WEI,Zhong-qiang YAO,Jin-xia ZHAO*( )
)
- Department of Rheumatology and Immunology, Peking University Third Hospital, Beijing 100191, China
摘要:
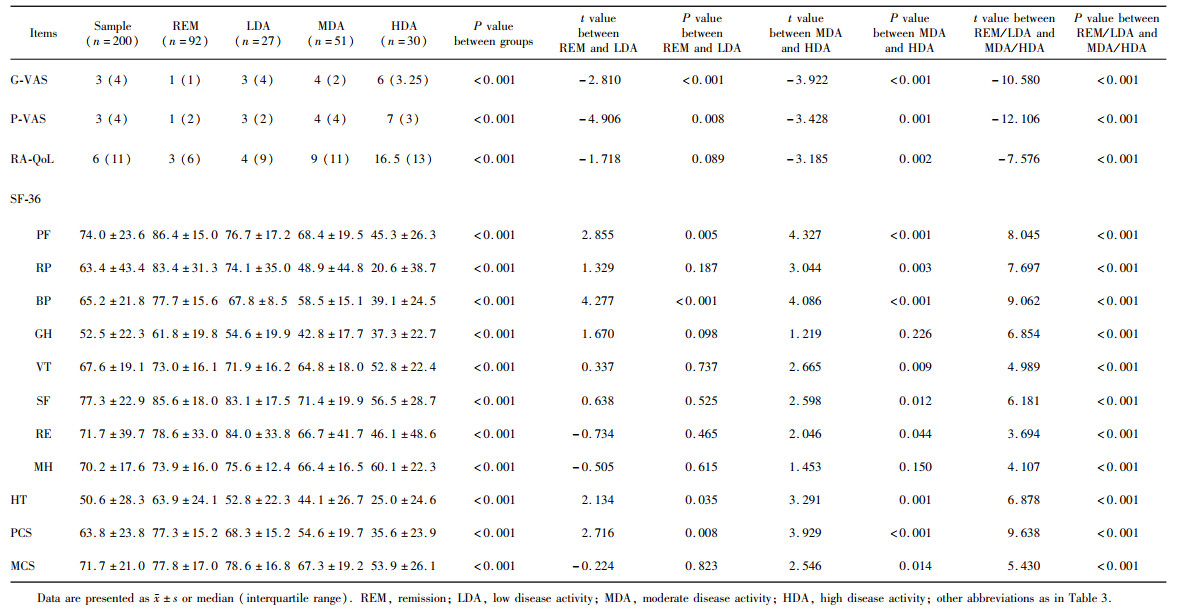
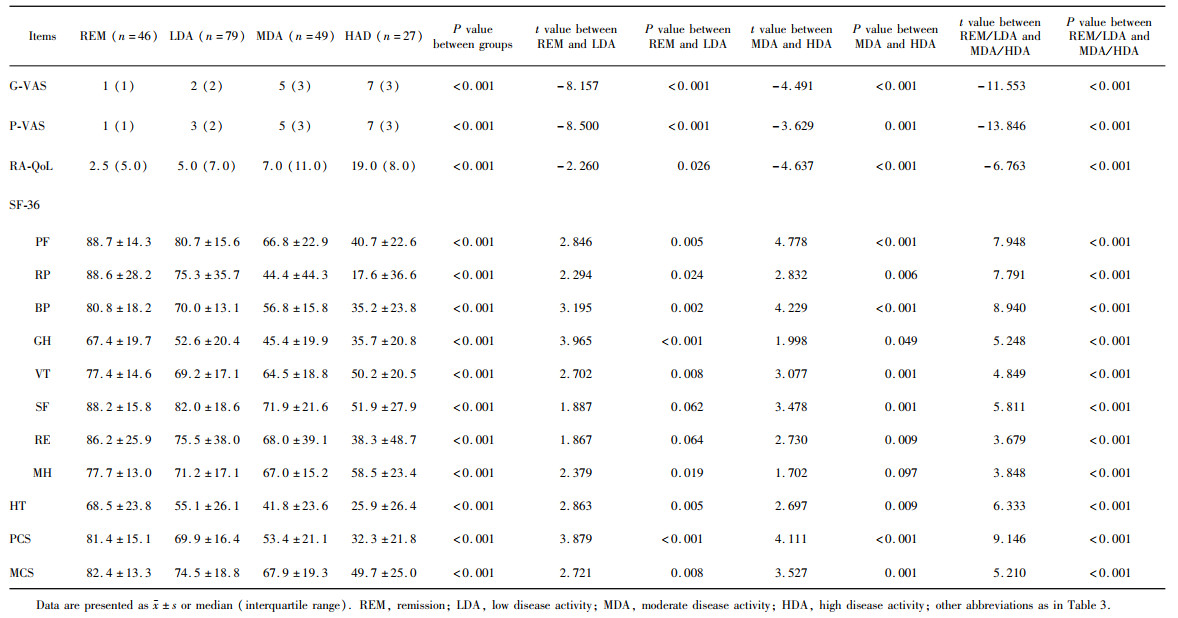
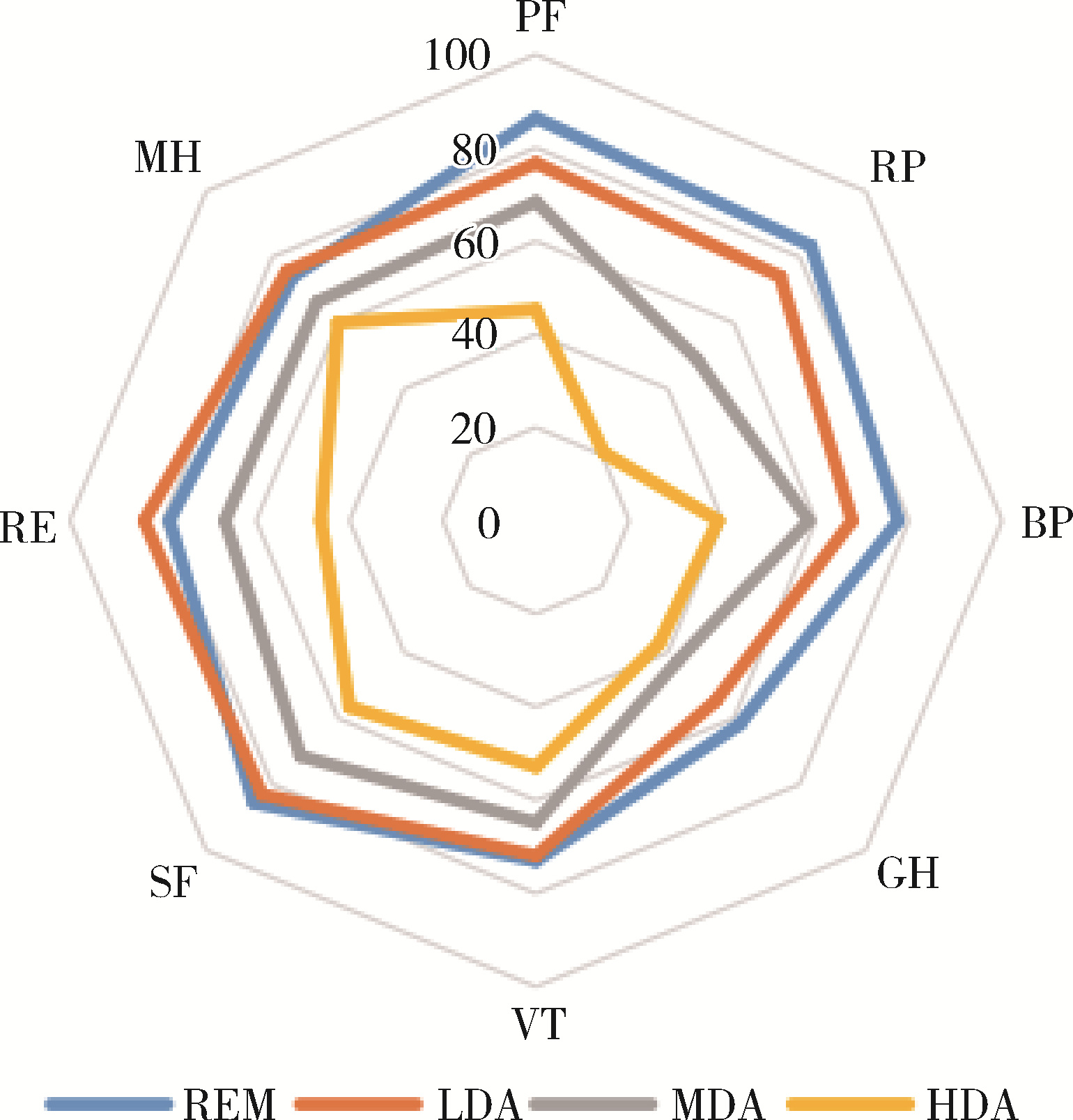
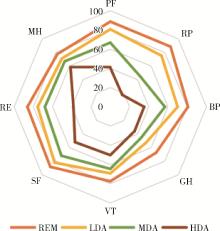
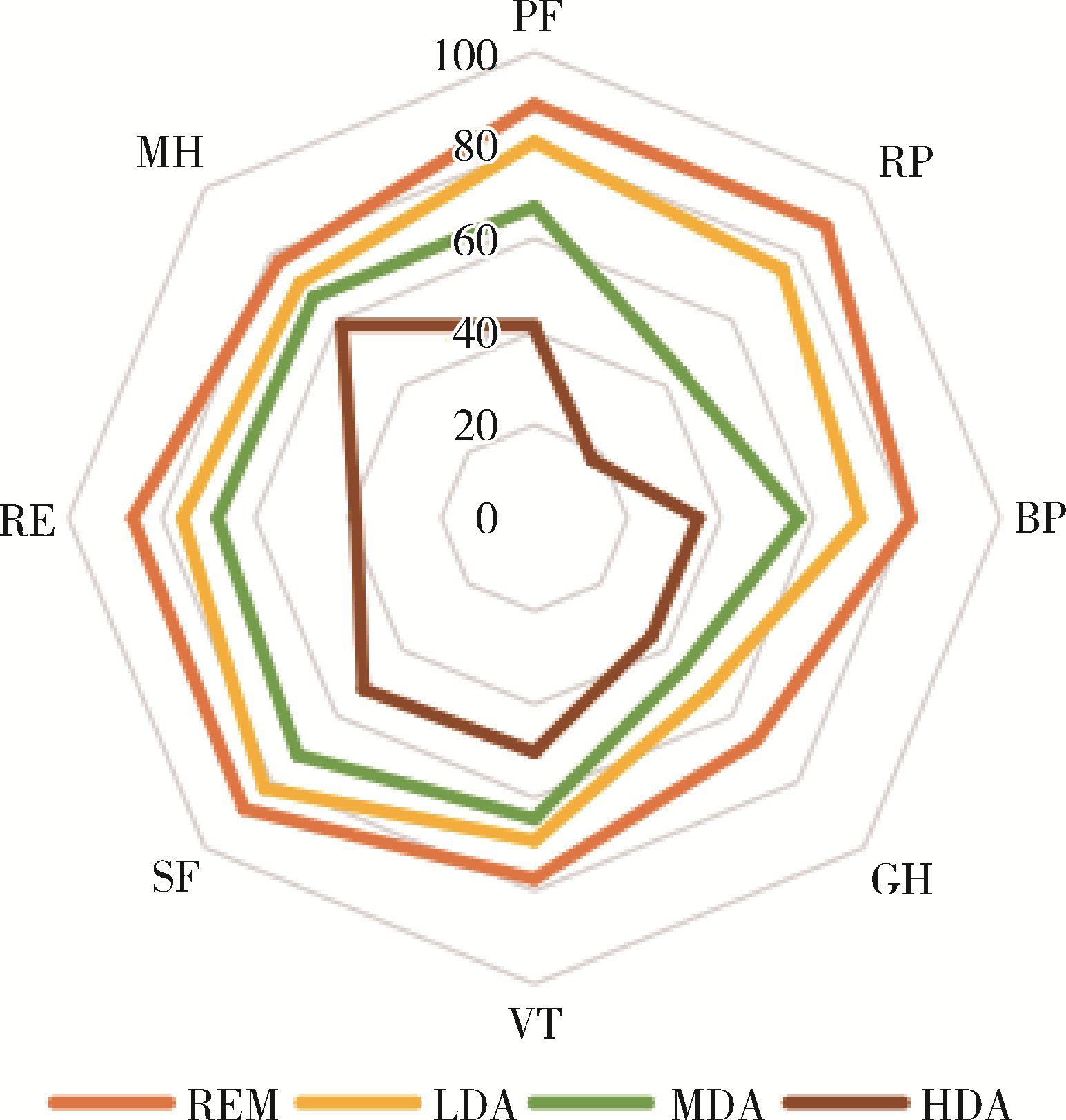
目的: 调查类风湿关节炎(rheumatoid arthritis,RA)患者健康相关生活质量(health related quality of life,HR-QoL)以及身体机能情况,分析疾病活动度对于HR-QoL以及各个维度身体机能的影响,并比较不同疾病活动判断标准下患者生活质量的差异。方法: 选择2021年1—7月于北京大学第三医院风湿免疫科门诊规律随诊的RA患者进行横断面调查,收集患者人口学资料、类风湿关节炎特异性生活质量(RA-specific quality of life,RA-QoL)评分以及36项简明健康调查问卷(the medical outcome 36-item short form health survey,SF-36)评分。符合正态分布的定量资料以${\bar x}$±s表示,两组间差异的比较采用t检验。结果: 共纳入RA患者207例,RA-QoL评分7.8±7.1,躯体功能汇总(physical component summary,PCS)评分63.8±23.8,心理功能汇总(mental component summary,MCS)评分71.7±21.0。以基于红细胞沉降率(erythrocyte sedimentation rate, ESR)的28个关节疾病活动度(disease activity score 28,DAS28)评分(DAS28-ESR)为标准,病情缓解、低疾病活动度的患者共119例(59.5%),以简明类风湿关节炎疾病活动指数(simplified disease activity index, SDAI)为标准,上述患者共125例(62.5%)。病情缓解或低疾病活动度的患者各个维度HR-QoL均显著优于治疗未达标的患者。以DAS28-ESR为评估标准,低疾病活动度组的生理功能评分(76.7±17.2 vs. 86.4±15.0, t=2.855, P < 0.01)、身体疼痛评分(67.8±8.5 vs. 77.7±15.6, t=4.277, P < 0.01)均低于完全缓解组,健康变化得分低于缓解组(52.8±22.3 vs. 63.9±24.1, t=2.134, P < 0.05),其他各个维度生活质量评分两组间差异无统计学意义。低疾病活动组PCS评分低于缓解组(68.3±15.2 vs. 77.3±15.2, t=2.716, P < 0.01),两组间MCS评分、RA-QoL评分差异无统计学意义。以SDAI为评估标准,低疾病活动度组RA-QoL评分显著高于缓解组(9.4±7.1 vs. 6.0±4.8, t=-2.260, P < 0.05),SF-36评分中躯体功能的各个维度以及PCS评分(69.9±16.4 vs. 81.4±15.1, t=3.879, P < 0.05)均低于缓解组,MCS评分低于缓解组(67.9±19.3 vs. 74.5±18.8, t=2.721, P < 0.01)。结论: 门诊就诊RA患者的RA-QoL以及SF-36评分情况较好,心理健康汇总评分高于躯体健康汇总评分,达标治疗对于提高HR-QoL至关重要。SDAI标准在缓解及低疾病活动度的RA患者中可以更好提示各个维度HR-QoL情况。
中图分类号:
- R593.22
| 1 |
Lee DM , Weinblatt ME . Rheumatoid arthritis[J]. Lancet, 2001, 358 (9285): 903- 911.
doi: 10.1016/S0140-6736(01)06075-5 |
| 2 | Lundkvist J , Kastäng F , Kobelt G , et al. The burden of rheumatoid arthritis and access to treatment: Health burden and costs[J]. Eur J Health Econ, 2008, 8 (Suppl 2): S49- S60. |
| 3 |
Li R , Sun J , Ren LM , et al. Epidemiology of eight common rheumatic diseases in China: A large-scale cross-sectional survey in Beijing[J]. Rheumatology (Oxford), 2012, 51 (4): 721- 729.
doi: 10.1093/rheumatology/ker370 |
| 4 | 中华人民共和国国家统计局第二次全国残疾人抽样调查领导小组. 第二次全国残疾人抽样调查主要数据公报[M]. 北京: 中国统计出版社, 2007. |
| 5 | Cunha-Miranda L , Santos H , Ferreira J , et al. Finding rheumatoid arthritis impact on life (FRAIL study): Economic burden[J]. Acta Reumatol Port, 2012, 37 (2): 134- 142. |
| 6 |
de Jong Z , van der Heijde D , McKenna SP , et al. The reliability and construct validity of the RAQoL: A rheumatoid arthritis-specific quality of life instrument[J]. Br J Rheumatol, 1997, 36 (8): 878- 883.
doi: 10.1093/rheumatology/36.8.878 |
| 7 |
Heimans L , Wevers-de Boer KV , Koudijs KK , et al. Health-related quality of life and functional ability in patients with early arthritis during remission steered treatment: Results of the IMPROVED study[J]. Arthritis Res Ther, 2013, 15 (5): R173.
doi: 10.1186/ar4361 |
| 8 |
Marshall S , Haywood K , Fitzpatrick R . Impact of patient-reported outcome measures on routine practice: A structured review[J]. J Eval Clin Pract, 2006, 12 (5): 559- 568.
doi: 10.1111/j.1365-2753.2006.00650.x |
| 9 |
Skevington SM , Day R , Chisholm A , et al. How much do doctors use quality of life information in primary care? Testing the trans-theoretical model of behaviour change[J]. Qual Life Res, 2005, 14 (4): 911- 922.
doi: 10.1007/s11136-004-3710-6 |
| 10 |
Rosa-Goncalves D , Bernardes M , Costa L . Quality of life and functional capacity in patients with rheumatoid arthritis: Cross-sectional study[J]. Reumatol Clin (Engl Ed), 2018, 14 (6): 360- 366.
doi: 10.1016/j.reuma.2017.03.002 |
| 11 |
Gerhold K , Richter A , Schneider M , et al. Health-related quality of life in patients with long-standing rheumatoid arthritis in the era of biologics: Data from the German biologics register RABBIT[J]. Rheumatology, 2015, 54 (10): 1858- 1866.
doi: 10.1093/rheumatology/kev194 |
| 12 |
Zhou YS , Wang XR , An Y , et al. Disability and health-related quality of life in Chinese patients with rheumatoid arthritis: A cross-sectional study[J]. Int J Rheum Dis, 2018, 21 (9): 1709- 1715.
doi: 10.1111/1756-185X.13345 |
| 13 |
Matcham F , Scott IC , Rayner L , et al. The impact of rheumatoid arthritis on quality-of-life assessed using the SF-36: A systematic review and meta-analysis[J]. Semin Arthritis Rheum, 2014, 44 (2): 123- 130.
doi: 10.1016/j.semarthrit.2014.05.001 |
| 14 |
Pencheva DT , Heaney A , McKenna SP , et al. Adaptation and validation of the rheumatoid arthritis quality of life (RAQoL) questionnaire for use in Bulgaria[J]. Rheumatol Int, 2020, 40 (12): 2077- 2083.
doi: 10.1007/s00296-020-04686-2 |
| 15 |
Rupp I , Boshuizen HC , Jacobi CE , et al. Impact of fatigue on health-related quality of life in rheumatoid arthritis[J]. Arthritis Rheum, 2004, 51 (4): 578- 585.
doi: 10.1002/art.20539 |
| 16 |
Bedi GS , Gupta N , Handa R , et al. Quality of life in Indian patients with rheumatoid arthritis[J]. Qual Life Res, 2005, 14 (8): 1953- 1958.
doi: 10.1007/s11136-005-4540-x |
| 17 |
Walker GJ , Littlejohn GO . Measuring quality of life in rheumatic conditions[J]. Clin Rheumatol, 2007, 26 (5): 671- 673.
doi: 10.1007/s10067-006-0450-8 |
| 18 |
Tander B , Cengiz K , Alayli G , et al. A comparative evaluation of health related quality of life and depression in patients with Wbromyalgia syndrome and rheumatoid arthritis[J]. Rheumatol Int, 2008, 28 (9): 859- 865.
doi: 10.1007/s00296-008-0551-6 |
| 19 |
Smolen JS , Aletaha D , Barton A , et al. Rheumatoid arthritis[J]. Nat Rev Dis Primers, 2018, 4, 18001.
doi: 10.1038/nrdp.2018.1 |
| 20 |
Waimann CA , Dal Pra FM , Marengo MF , et al. Quality of life of patients with rheumatoid arthritis in Argentina: Rliability, validity, and sensitivity to change of a Spanish version of the rheumatoid arthritis quality of life questionnaire[J]. Clin Rheumatol, 2012, 31 (7): 1065- 1071.
doi: 10.1007/s10067-012-1976-6 |
| 21 | Chiu YM , Lai MS , Lin HY , et al. Disease activity affects all domains of quality of life in patients with rheumatoid arthritis and is modified by disease duration[J]. Clin Exp Rheumatol, 2014, 32 (6): 898- 903. |
| 22 |
Schmalz G , Noack S , Patschan S , et al. Disease activity, morning stiffness and missing teeth are associated with oral health-related quality of life in individuals with rheumatoid arthritis[J]. Clin Oral Investig, 2020, 24 (10): 3559- 3566.
doi: 10.1007/s00784-020-03226-3 |
| [1] | 刘东武, 陈杰, 高明利, 于静. 类风湿关节炎伴发淋巴结Castleman样病理改变1例[J]. 北京大学学报(医学版), 2024, 56(5): 928-931. |
| [2] | 黄会娜,赵静,赵祥格,白自然,李霞,王冠. 乳酸对类风湿关节炎患者外周血CD4+T细胞亚群的调控作用[J]. 北京大学学报(医学版), 2024, 56(3): 519-525. |
| [3] | 汤晓菲,李永红,丁秋玲,孙卓,张阳,王育梅,田美伊,刘坚. 类风湿关节炎患者下肢深静脉血栓发病率及危险因素[J]. 北京大学学报(医学版), 2024, 56(2): 279-283. |
| [4] | 邹雪,白小娟,张丽卿. 艾拉莫德联合托法替布治疗难治性中重度类风湿关节炎的疗效[J]. 北京大学学报(医学版), 2023, 55(6): 1013-1021. |
| [5] | 吴琦,蔡月明,何娟,黄文蒂,王庆文. 血脂异常与类风湿关节炎肺间质病变的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 982-992. |
| [6] | 张警丰,金银姬,魏慧,姚中强,赵金霞. 体重指数与类风湿关节炎临床特征的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 993-999. |
| [7] | 赖金惠,王起,姬家祥,王明瑞,唐鑫伟,许克新,徐涛,胡浩. 新型冠状病毒肺炎疫情期间延迟拔除输尿管支架对泌尿系结石术后患者生活质量和心理状态的影响[J]. 北京大学学报(医学版), 2023, 55(5): 857-864. |
| [8] | 金银姬,孙琳,赵金霞,刘湘源. 血清IgA型抗鼠科肉瘤病毒癌基因同源物B1抗体在类风湿关节炎中的意义[J]. 北京大学学报(医学版), 2023, 55(4): 631-635. |
| [9] | 李志华,黄燕波,庞秋颖,于书慧,陈宇珂,李德润. 膀胱阴道瘘修补术后患者生存质量和心理状态调查[J]. 北京大学学报(医学版), 2023, 55(1): 190-193. |
| [10] | 蔡文心,李仕成,刘一鸣,梁如玉,李静,郭建萍,胡凡磊,孙晓麟,李春,刘栩,叶华,邓立宗,李茹,栗占国. 类风湿关节炎临床分层及其特征的横断面研究[J]. 北京大学学报(医学版), 2022, 54(6): 1068-1073. |
| [11] | 程昉,杨邵英,房星星,王璇,赵福涛. CCL28-CCR10通路在类风湿关节炎单核细胞迁移中的作用[J]. 北京大学学报(医学版), 2022, 54(6): 1074-1078. |
| [12] | 刘蕊,赵金霞,闫良. 类风湿关节炎合并下肢静脉血栓患者的临床特点[J]. 北京大学学报(医学版), 2022, 54(6): 1079-1085. |
| [13] | 高超,陈立红,王莉,姚鸿,黄晓玮,贾语博,刘田. 类风湿关节炎合并纤维肌痛简易分类标准的临床验证[J]. 北京大学学报(医学版), 2022, 54(2): 278-282. |
| [14] | 娄雪,廖莉,李兴珺,王楠,刘爽,崔若玫,徐健. 类风湿关节炎患者外周血TWEAK基因启动子区甲基化状态及其表达[J]. 北京大学学报(医学版), 2021, 53(6): 1020-1025. |
| [15] | 钟华,徐丽玲,白明欣,苏茵. 类风湿关节炎患者趋化因子CXCL9和CXCL10在骨侵蚀中的作用[J]. 北京大学学报(医学版), 2021, 53(6): 1026-1031. |
|
||