北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (5): 857-864. doi: 10.19723/j.issn.1671-167X.2023.05.013
新型冠状病毒肺炎疫情期间延迟拔除输尿管支架对泌尿系结石术后患者生活质量和心理状态的影响
赖金惠,王起,姬家祥,王明瑞,唐鑫伟,许克新,徐涛,胡浩*( )
)
- 北京大学人民医院泌尿外科, 北京 100044
Effects of delayed ureteral stents removal during the COVID-19 pandemic on the quality of life and psychological status of postoperative patients with urinary calculi
Jin-hui LAI,Qi WANG,Jia-xiang JI,Ming-rui WANG,Xin-wei TANG,Ke-xin XU,Tao XU,Hao HU*( )
)
- Department of Urology, Peking University People's Hospital, Beijing 100044, China
摘要:
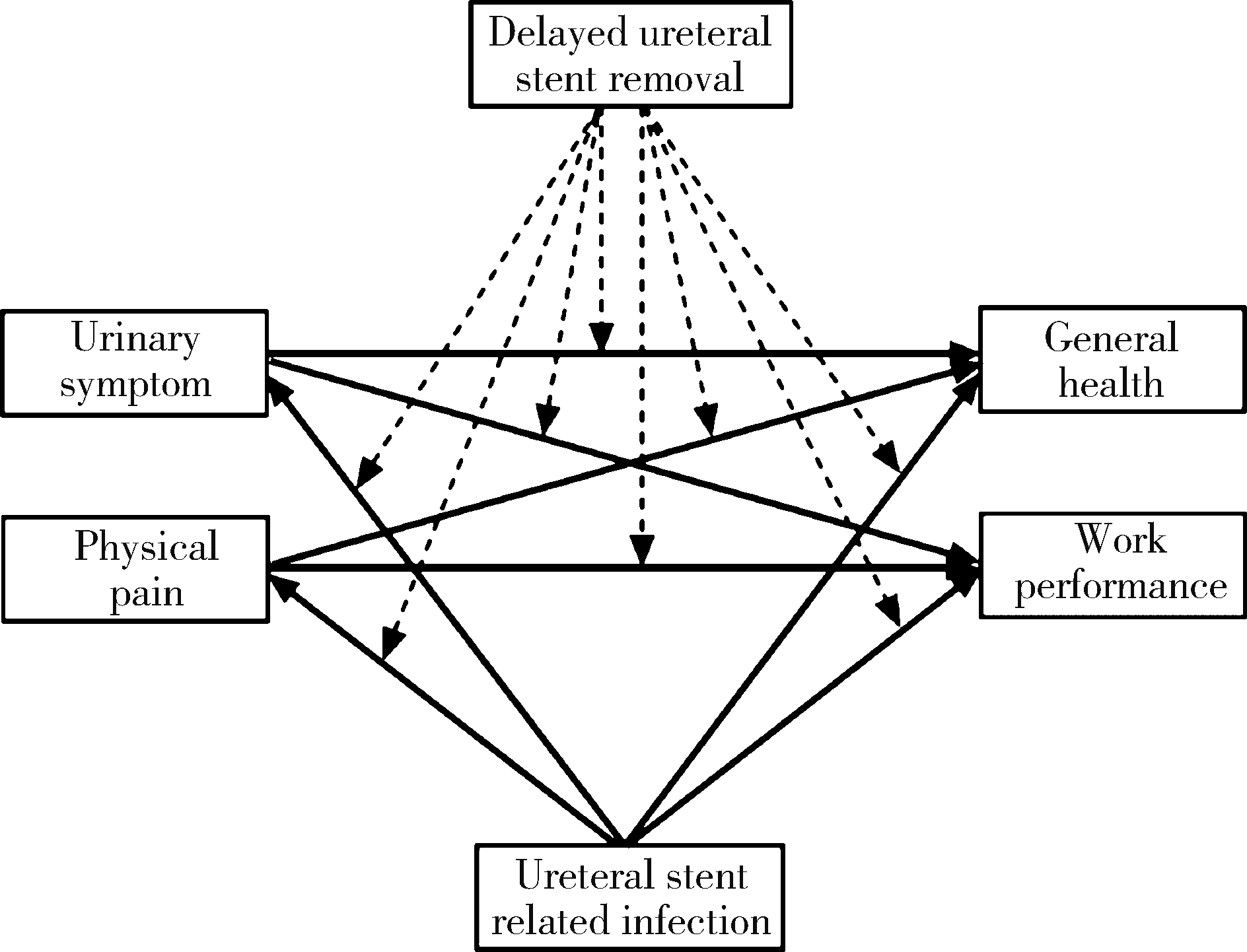
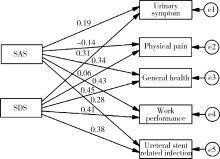
目的: 探讨因新型冠状病毒肺炎(corona virus disease 2019, COVID-19)疫情而延迟拔除输尿管支架对泌尿系结石术后患者生活质量(quality of life, QoL) 和心理状态的影响。方法: 选择2019年12月至2020年6月在北京大学人民医院接受上尿路内镜碎石术后留置输尿管支架并返回医院取出支架患者的病例资料进行回顾性分析,收集患者人口学资料、输尿管支架症状问卷(ureteral stent symptoms questionnaire, USSQ)评分、焦虑自评量表(self-rating anxiety scale, SAS)评分和抑郁自评量表(self-rating depression scale, SDS)评分等。USSQ由6个维度(包括排尿症状、躯体疼痛、一般健康状态、工作表现、性功能和支架相关感染)共44个问题组成,量表大部分问题采用李克特(Likert)五级量表,小部分问题采用四级或七级量表量化。SAS和SDS均由20个问题组成, 用于评估患者的焦虑抑郁状态,两个量表采用李克特四级量表,主要统计指标总分(20~80分)。使用标准分(总分乘以1.25取其整数)量化临床焦虑和抑郁程度,并运用矩阵结构分析构建多群组结构方程模型。结果: 共纳入患者71例,输尿管支架中位留置时间对照组32(30, 33) d与延迟组94.5(88, 103) d相比,差异有统计学意义。延迟组患者在USSQ多维度中(包括排尿症状、一般健康状态、工作表现和支架相关感染)得分较高,焦虑和抑郁程度也明显比对照组严重。延长输尿管支架留置时间会加重患者排尿症状、躯体疼痛共同对工作表现的负面影响(P=0.029 < 0.05),其中,患者较严重的排尿症状导致工作表现欠佳受延长置管时间的影响最显著(CR=2.619>1.96)。新型冠状病毒肺炎疫情期间患者焦虑抑郁程度与支架相关症状严重度呈正相关。结论: 因新型冠状病毒肺炎疫情延迟拔管患者的QoL较差,焦虑和抑郁程度较重;新型冠状病毒肺炎疫情期间患者焦虑抑郁程度越重,支架相关症状会加重。为了提高泌尿系结石术后患者在新型冠状病毒肺炎疫情期间的QoL和心理健康水平,应避免延长支架留置时间或采取相应的干预措施。
中图分类号:
- R699
| 1 |
Alnadhari I , Alwan MA , Salah MA , et al. Treatment of retained encrusted ureteral double-J stent[J]. Arch Ital Urol Androl, 2019, 90 (4): 265- 269.
doi: 10.4081/aiua.2018.4.265 |
| 2 |
Tae BS , Cho S , Jeon BJ , et al. Does mirabegron relieve ureteric stent-related discomfort? A prospective, randomized, multicentre study[J]. BJU Int, 2018, 122 (5): 866- 872.
doi: 10.1111/bju.14416 |
| 3 |
Bosio A , Alessandria E , Dalmasso E , et al. How bothersome double-J ureteral stents are after semirigid and flexible ureteroscopy: A prospective single-institution observational study[J]. World J Urol, 2019, 37 (1): 201- 207.
doi: 10.1007/s00345-018-2376-6 |
| 4 |
Lin TF , Lin WR , Chen M , et al. The risk factors and complications of forgotten double-J stents: A single-center experience[J]. J Chin Med Assoc, 2019, 82 (10): 767- 771.
doi: 10.1097/JCMA.0000000000000161 |
| 5 |
Rabani SM . Combined percutaneous and transurethral lithotripsy for forgotten ureteral stents with giant encrustation[J]. Nephrourol Mon, 2012, 4 (4): 633- 635.
doi: 10.5812/numonthly.4087 |
| 6 |
Nerli RB , Magdum PV , Sharma V , et al. Forgotten/retained double J ureteric stents: A source of severe morbidity in children[J]. Afr J Paediatr Surg, 2016, 13 (1): 32- 35.
doi: 10.4103/0189-6725.181704 |
| 7 |
Westhofen T , Magistro G , Lennartz S , et al. Confronting hidden COVID-19 burden: A telemedical solution for elective urological outpatient clinics[J]. Infection, 2020, 48 (6): 935- 939.
doi: 10.1007/s15010-020-01511-7 |
| 8 |
Zhu C , Qu J , Yang L , et al. The chinese linguistic validation of the ureteral stent symptom questionnaire[J]. Urol Int, 2019, 102 (2): 194- 198.
doi: 10.1159/000493764 |
| 9 |
Wang C , Zhao H . The Impact of COVID-19 on anxiety in Chinese university students[J]. Front Psychol, 2020, 11, 1168.
doi: 10.3389/fpsyg.2020.01168 |
| 10 | Lei L , Huang X , Zhang S , et al. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China[J]. Med Sci Monit, 2020, 26, e924609-1- e924609-12. |
| 11 |
Wu G , Sun F , Sun K , et al. Impact of differential ureteral stent diameters on clinical outcomes after ureteroscopy intracorporeal lithotripsy: A systematic review and meta-analysis[J]. Int J Urol, 2021, 28 (10): 992- 999.
doi: 10.1111/iju.14631 |
| 12 |
Pecoraro A , Peretti D , Tian Z , et al. Treatment of ureteral stent-related symptoms[J]. Urol Int, 2023, 107 (3): 288- 303.
doi: 10.1159/000518387 |
| 13 |
Bao X , Sun F , Yao H , et al. Distal end of double-J ureteral stent position on ureteral stent-related symptoms: A systematic review and meta-analysis[J]. Front Surg, 2022, 9, 990049.
doi: 10.3389/fsurg.2022.990049 |
| 14 |
Kuehhas FE , Miernik A , Sharma V , et al. A prospective evaluation of pain associated with stone passage, stents, and stent removal using a visual analog scale[J]. Urology, 2013, 82 (3): 521- 525.
doi: 10.1016/j.urology.2013.04.031 |
| 15 | Polat H , Yucel MO , Utangac MM , et al. Management of forgotten ureteral stents: Relationship between indwelling time and required treatment approaches[J]. Balkan Med J, 2017, 34 (4): 301- 307. |
| 16 |
Bidnur S , Huynh M , Hoag N , et al. An indwelling ureteral stent forgotten for over 12 years[J]. J Endourol Case Rep, 2016, 2 (1): 135- 137.
doi: 10.1089/cren.2016.0073 |
| 17 |
Nevo A , Mano R , Baniel J , et al. Ureteric stent dwelling time: A risk factor for post-ureteroscopy sepsis[J]. BJU Int, 2017, 120 (1): 117- 122.
doi: 10.1111/bju.13796 |
| 18 | Ramachandra M , Mosayyebi A , Carugo D , et al. Strategies to improve patient outcomes and QoL: Current complications of the design and placements of ureteric stents[J]. Res Rep Urol, 2020, 12, 303- 314. |
| 19 | Kartal IG , Baylan B , Gok A , et al. The association of encrustation and ureteral stent indwelling time in urolithiasis and KUB grading system[J]. Urol J, 2018, 15 (6): 323- 328. |
| 20 |
Frank A , Hormann S , Krombach J , et al. COVID-19 concerns and worries in patients with mental illness[J]. Psychiatr Prax, 2020, 47 (5): 267- 272.
doi: 10.1055/a-1179-4230 |
| 21 |
Wang Y , Yang Y , Yan C , et al. COVID-induced 3 weeks' treatment delay may exacerbate breast cancer patient's psychological symptoms[J]. Front Psychol, 2022, 13, 1003016.
doi: 10.3389/fpsyg.2022.1003016 |
| [1] | 王敏, 李倩. 青少年抑郁症患者心理弹性影响因素的路径分析[J]. 北京大学学报(医学版), 2024, 56(5): 809-814. |
| [2] | 陈敬,单蕊,肖伍才,张晓蕊,刘峥. 青春期和成年早期自制力与抑郁症状和超重肥胖共病风险的关联:基于全国调查的十年前瞻性队列研究[J]. 北京大学学报(医学版), 2024, 56(3): 397-402. |
| [3] | 汤华萌,袁典琪,王明星,杨晗冰,郭超. 数字融入和健康生活方式对社会经济状况与老年人抑郁关系的序列中介作用[J]. 北京大学学报(医学版), 2024, 56(2): 230-238. |
| [4] | 李建斌,吕梦娜,池强,彭一琳,刘鹏程,吴锐. 干燥综合征患者发生重症新型冠状病毒肺炎的早期预测[J]. 北京大学学报(医学版), 2023, 55(6): 1007-1012. |
| [5] | 祝春素,连至炜,崔一民. 中国中老年人抑郁和慢性病的关联[J]. 北京大学学报(医学版), 2023, 55(4): 606-611. |
| [6] | 王婷,李乔晟,刘皓冉,简伟研. 人格特征、城乡差异与抑郁症状变化的关系[J]. 北京大学学报(医学版), 2023, 55(3): 385-391. |
| [7] | 袁雯,张奕,陈力,蒋家诺,陈曼曼,刘婕妤,马涛,马奇,崔孟杰,郭桐君,王鑫鑫,董彦会,马军. 儿童青少年身体脂肪分布与抑郁和社交焦虑的关联:基于双能X线检测的横断面研究[J]. 北京大学学报(医学版), 2023, 55(3): 429-435. |
| [8] | 张紫薇,花语蒙,刘爱萍. 中国中老年人群抑郁症状、缺血性心血管疾病10年风险对心血管疾病的联合影响[J]. 北京大学学报(医学版), 2023, 55(3): 465-470. |
| [9] | 陆林,刘晓星,袁凯. 中国脑科学计划进展[J]. 北京大学学报(医学版), 2022, 54(5): 791-795. |
| [10] | 康志宇,王磊磊,韩永正,郭向阳. 北京冬季奥林匹克运动会运动员手术的麻醉管理[J]. 北京大学学报(医学版), 2022, 54(4): 770-773. |
| [11] | 刘熠华,云青萍,张蓝超,张晓悦,林郁婷,刘芳静,郑志杰,常春. 久坐行为与体育锻炼行为对职业人群焦虑倾向的联合作用[J]. 北京大学学报(医学版), 2022, 54(3): 490-497. |
| [12] | 陈明隆,刘笑晗,郭静. 新型冠状病毒肺炎疫情下儿童父母社会支持与养育倦怠的关系[J]. 北京大学学报(医学版), 2022, 54(3): 520-525. |
| [13] | 樊理诗,高敏,Edwin B.FISHER,孙昕霙. 北京市通州区和顺义区747例2型糖尿病患者生存质量影响因素[J]. 北京大学学报(医学版), 2021, 53(3): 523-529. |
| [14] | 耿研,宋志博,张晓慧,邓雪蓉,王昱,张卓莉. 银屑病关节炎抑郁和焦虑患病情况及相关因素[J]. 北京大学学报(医学版), 2020, 52(6): 1048-1055. |
| [15] | 王一帆,范稹,成姚斌,金月波,霍阳,何菁. 原发性干燥综合征患者睡眠障碍的相关影响因素[J]. 北京大学学报(医学版), 2020, 52(6): 1063-1068. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 162
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 280
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||