北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (2): 299-306. doi: 10.19723/j.issn.1671-167X.2024.02.015
胫距跟融合治疗终末期踝和后足病变的中短期临床结果
李文菁,张保宙,李恒,赖良鹏,杜辉,孙宁,龚晓峰,李莹*( ),王岩,武勇
),王岩,武勇
- 首都医科大学附属北京积水潭医院足踝外科, 北京 100035
Tibiotalocalcaneal arthrodesis for end-stage ankle and hindfoot arthropathy: Short- and mid-term clinical outcomes
Wenjing LI,Baozhou ZHANG,Heng LI,Liangpeng LAI,Hui DU,Ning SUN,Xiaofeng GONG,Ying LI*( ),Yan WANG,Yong WU
),Yan WANG,Yong WU
- Department of Foot and Ankle Surgery, Beijing Jishuitan Hospital, Capital Medical University, Beijing 100035, China
摘要:
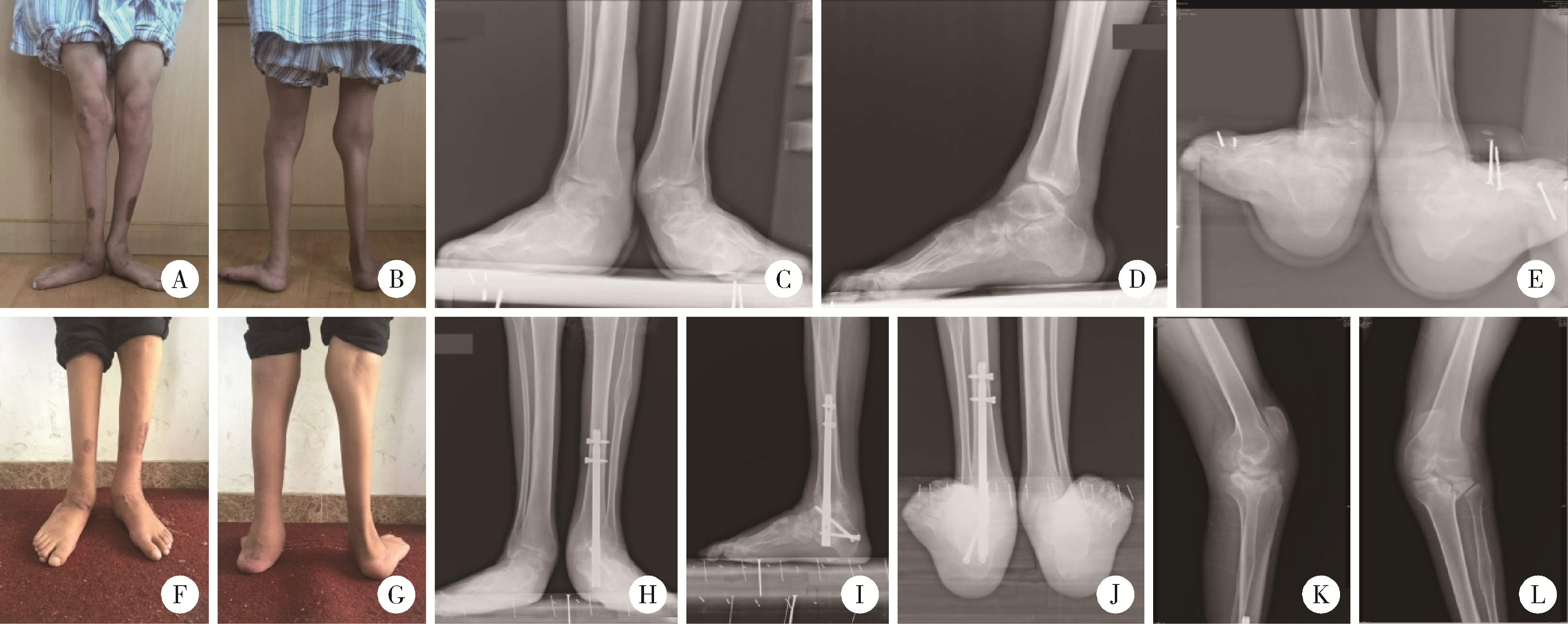
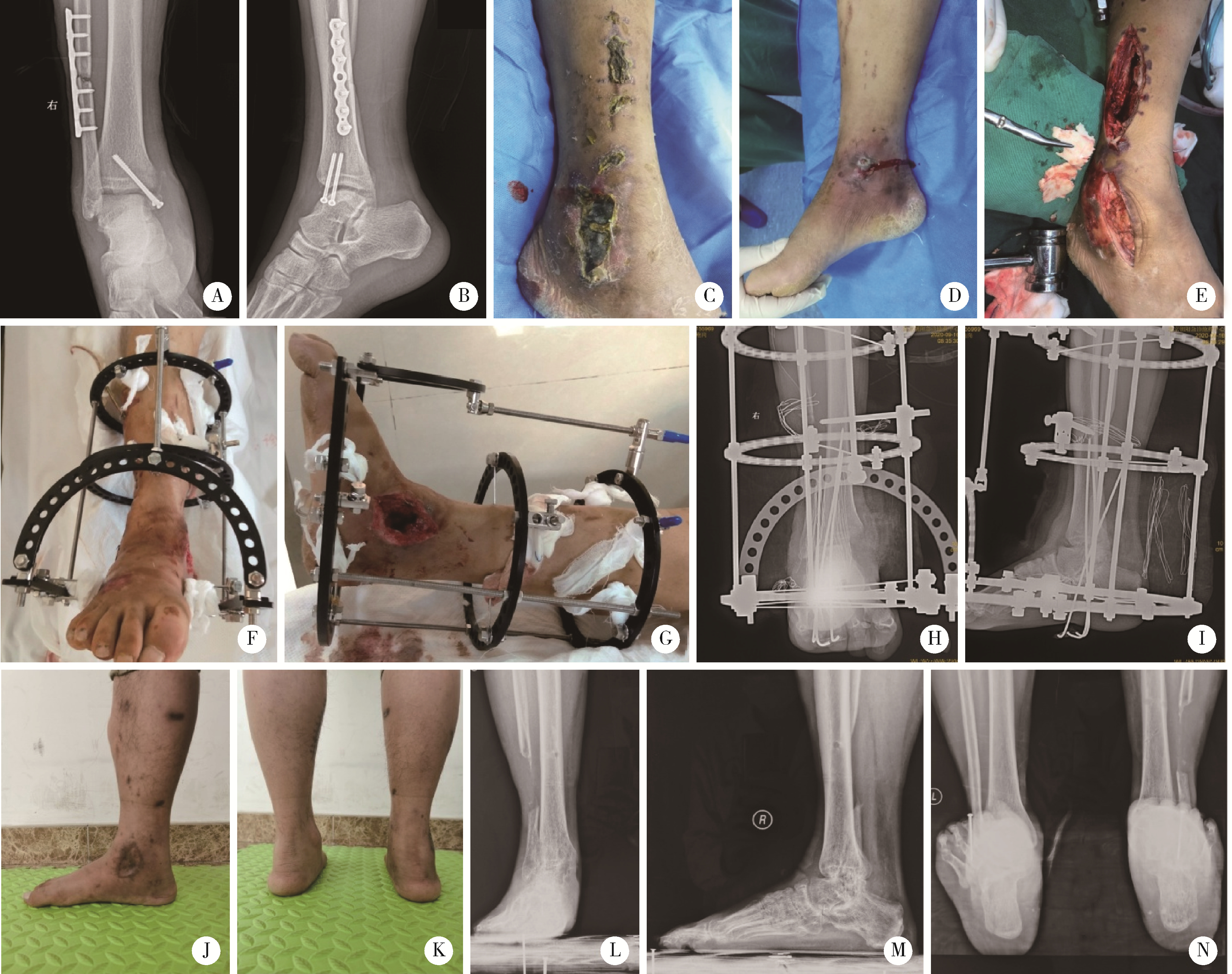
目的: 分析同一术者行胫距跟(tibiotalocalcaneal, TTC)融合手术的患者临床资料,探讨患者临床结果、并发症和功能改善情况,分析TTC融合手术的临床预后及注意事项。方法: 回顾性分析2011年3月至2020年12月由同一术者行TTC融合手术治疗的40例患者的临床资料,其中男23例,女17例,平均年龄(49.1±16.0)岁,均为单侧手术。记录患者一般临床特征、影像学表现、主要诊断、具体手术方式。对比术前及末次随访时患者的美国足踝外科协会(American Orthopaedic Foot and Ankle Society, AOFAS)踝-后足评分、疼痛视觉模拟评分(visual analogue scale,VAS),记录融合愈合时间、症状较术前改善情况(明显改善、部分改善、无改善或恶化)以及术后并发症的发生情况。结果: 患者的术后中位随访时间为38.0(26.3, 58.8)个月;术前中位VAS评分为6.0(4.0, 7.0)分,中位AOFAS评分为33.0(25.3, 47.3)分;末次随访时患者的中位VAS评分为0(0, 3.0)分,中位AOFAS评分为80.0(59.0, 84.0)分;均较术前明显改善(P < 0.05)。所有患者均无切口坏死及感染,1例发生距下关节不愈合,为梅毒夏科氏(Charcot)关节,其余患者中位骨愈合时间为15.0(12.0, 20.0)周。所有患者中,较术前有明显改善者25例,部分改善者8例,改善不明显者4例,症状较术前加重者3例。结论: TTC融合术是治疗后足终末期病变的可靠方法,多数患者术后功能有改善,日常生活影响不大,预后差的原因包括足趾僵硬、邻近膝关节应力集中、不愈合及不明原因疼痛等。
中图分类号:
- R687.4
| 1 |
Brage ME , Mathews CS . Ankle and tibiotalocalcaneal fusion[J]. Foot Ankle Clin, 2022, 27 (2): 343- 353.
doi: 10.1016/j.fcl.2021.11.020 |
| 2 |
Stołtny T , Dugiełło B , Pasek J , et al. Tibiotalocalcaneal arthrodesis in osteoarthritis deformation of ankle and subtalar joint: Evaluation of treatment results[J]. J Foot Ankle Surg, 2022, 61 (1): 205- 211.
doi: 10.1053/j.jfas.2021.09.005 |
| 3 |
Yao Y , Mo Z , Wu G , et al. A personalized 3D-printed plate for tibiotalocalcaneal arthrodesis: Design, fabrication, biomechanical evaluation and postoperative assessment[J]. Comput Biol Med, 2021, 133, 104368.
doi: 10.1016/j.compbiomed.2021.104368 |
| 4 |
Perez-Aznar A , Gonzalez-Navarro B , Bello-Tejeda LL , et al. Tibiotalocalcaneal arthrodesis with a retrograde intramedullary nail: A prospective cohort study at a minimum five year follow-up[J]. Int Orthop, 2021, 45 (9): 2299- 2305.
doi: 10.1007/s00264-020-04904-3 |
| 5 |
Pitts C , Alexander B , Washington J , et al. Factors affecting the outcomes of tibiotalocalcaneal fusion[J]. Bone Joint J, 2020, 102-B (3): 345- 351.
doi: 10.1302/0301-620X.102B3.BJJ-2019-1325.R1 |
| 6 |
Kitaoka HB , Alexander IJ , Adelaar RS , et al. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes[J]. Foot Ankle Int, 1994, 15 (7): 349- 353.
doi: 10.1177/107110079401500701 |
| 7 |
Reed MD , van Nostran W . Assessing pain intensity with the visual analog scale: A plea for uniformity[J]. J Clin Pharmacol, 2014, 54 (3): 241- 244.
doi: 10.1002/jcph.250 |
| 8 |
Martínez-de-Albornoz P , Monteagudo M . Tibiotalocalcaneal arthrodesis in severe hindfoot deformities[J]. Foot Ankle Clin, 2022, 27 (4): 847- 866.
doi: 10.1016/j.fcl.2022.08.008 |
| 9 |
Burns PR , Dunse A . Tibiotalocalcaneal arthrodesis for foot and ankle deformities[J]. Clin Podiatr Med Surg, 2017, 34 (3): 357- 380.
doi: 10.1016/j.cpm.2017.02.007 |
| 10 |
Monteagudo M , Martínez-de-Albornoz P . Deciding between ankle and tibiotalocalcaneal arthrodesis for isolated ankle arthritis[J]. Foot Ankle Clin, 2022, 27 (1): 217- 231.
doi: 10.1016/j.fcl.2021.11.012 |
| 11 |
Rana B , Patel S . Results of ankle and hind foot arthrodesis in diabetic Charcot neuroarthropathy: A retrospective analysis of 44 patients[J]. J Clin Orthop Trauma, 2021, 23, 101637.
doi: 10.1016/j.jcot.2021.101637 |
| 12 |
Chraim M , Krenn S , Alrabai HM , et al. Mid-term follow-up of patients with hindfoot arthrodesis with retrograde compression intramedullary nail in Charcot neuroarthropathy of the hindfoot[J]. Bone Joint J, 2018, 100-B (2): 190- 196.
doi: 10.1302/0301-620X.100B2.BJJ-2017-0374.R2 |
| 13 |
Kollig E , Esenwein SA , Muhr G , et al. Fusion of the septic ankle: Experience with 15 cases using hybrid external fixation[J]. J Trauma, 2003, 55 (4): 685- 691.
doi: 10.1097/01.TA.0000051933.83342.E4 |
| 14 |
Hartmann R , Grubhofer F , Waibel FWA , et al. Treatment of hindfoot and ankle infections with Ilizarov external fixator or spacer, followed by secondary arthrodesis[J]. J Orthop Res, 2021, 39 (10): 2151- 2158.
doi: 10.1002/jor.24938 |
| 15 |
Baumbach SF , Massen FK , Hörterer S , et al. Comparison of arthroscopic to open tibiotalocalcaneal arthrodesis in high-risk patients[J]. Foot Ankle Surg, 2019, 25 (6): 804- 811.
doi: 10.1016/j.fas.2018.10.006 |
| 16 |
Rausch S , Loracher C , Fröber R , et al. Anatomical evaluation of different approaches for tibiotalocalcaneal arthrodesis[J]. Foot Ankle Int, 2014, 35 (2): 163- 167.
doi: 10.1177/1071100713517095 |
| 17 |
Wu M , Scott D , Abar B , et al. Does a fibula-sparing approach improve outcomes in tibiotalocalcaneal arthrodesis?[J]. Foot Ankle Surg, 2023, 29 (1): 90- 96.
doi: 10.1016/j.fas.2022.11.001 |
| 18 |
Carranza-Bencano A , Tejero S , Del CG , et al. Minimal incision surgery for tibiotalocalcaneal arthrodesis[J]. Foot Ankle Int, 2014, 35 (3): 272- 284.
doi: 10.1177/1071100713515447 |
| 19 |
Pellegrini MJ , Schiff AP , Adams SJ , et al. Outcomes of tibiotalocalcaneal arthrodesis through a posterior Achilles tendon-splitting approach[J]. Foot Ankle Int, 2016, 37 (3): 312- 319.
doi: 10.1177/1071100715615398 |
| 20 |
Eckholt S , Garcia-Elvira R , Fontecilla N , et al. Role of extra-articular tibiotalocalcaneal arthrodesis and posterior approach in highly complex cases[J]. Foot Ankle Int, 2018, 39 (2): 219- 225.
doi: 10.1177/1071100717737973 |
| 21 |
Gong J , Zhou B , Tao X , et al. Tibiotalocalcaneal arthrodesis with headless compression screws[J]. J Orthop Surg Res, 2016, 11 (1): 91.
doi: 10.1186/s13018-016-0425-7 |
| 22 |
Gutteck N , Schilde S , Reichel M , et al. Posterolateral plate fixation with Pantalarlock® is more stable than nail fixation in tibiotalocalcaneal arthrodesis in a biomechanical cadaver study[J]. Foot Ankle Surg, 2020, 26 (3): 328- 333.
doi: 10.1016/j.fas.2019.04.006 |
| 23 |
Richman J , Cota A , Weinfeld S . Intramedullary nailing and external ring fixation for tibiotalocalcaneal arthrodesis in Charcot arthropathy[J]. Foot Ankle Int, 2017, 38 (2): 149- 152.
doi: 10.1177/1071100716671884 |
| [1] | 邹雪,白小娟,张丽卿. 艾拉莫德联合托法替布治疗难治性中重度类风湿关节炎的疗效[J]. 北京大学学报(医学版), 2023, 55(6): 1013-1021. |
| [2] | 薛蔚,董樑,钱宏阳,费笑晨. 前列腺癌新辅助治疗与辅助治疗的现状及进展[J]. 北京大学学报(医学版), 2023, 55(5): 775-780. |
| [3] | 邱敏,宗有龙,王滨帅,杨斌,徐楚潇,孙争辉,陆敏,赵磊,卢剑,刘承,田晓军,马潞林. 腹腔镜肾部分切除术治疗中高复杂程度肾肿瘤的效果[J]. 北京大学学报(医学版), 2023, 55(5): 833-837. |
| [4] | 王磊,韩天栋,江卫星,李钧,张道新,田野. 主动迁移技术与原位碎石技术在输尿管软镜治疗1~2 cm输尿管上段结石中的安全性和有效性比较[J]. 北京大学学报(医学版), 2023, 55(3): 553-557. |
| [5] | 熊士凯,史尉利,王安鸿,谢兴,郭秦炜. 腓骨远端撕脱骨折的影像学诊断:踝关节X线与CT三维重建的比较[J]. 北京大学学报(医学版), 2023, 55(1): 156-159. |
| [6] | 李伟浩,李伟,张学民,李清乐,焦洋,张韬,蒋京军,张小明. 去分支杂交手术和传统手术治疗胸腹主动脉瘤的结果比较[J]. 北京大学学报(医学版), 2022, 54(1): 177-181. |
| [7] | 邓雪蓉,孙晓莹,张卓莉. 类风湿关节炎患者足踝部体征和超声下病变的一致性[J]. 北京大学学报(医学版), 2021, 53(6): 1037-1042. |
| [8] | 敖明昕,李学民,于媛媛,时会娟,黄红拾,敖英芳,王薇. 视觉重建对老年人行走动态足底压力的影响[J]. 北京大学学报(医学版), 2021, 53(5): 907-914. |
| [9] | 朱正达,高岩,何汶秀,方鑫,刘洋,魏攀,闫志敏,华红. 红色诺卡氏菌细胞壁骨架治疗糜烂型口腔扁平苔藓的疗效及安全性[J]. 北京大学学报(医学版), 2021, 53(5): 964-969. |
| [10] | 刘立立,刘志科,张良,李宁,方挺,张栋梁,许国章,詹思延. 2016—2019年宁波市5岁及以下儿童手足口病流行病学特征[J]. 北京大学学报(医学版), 2021, 53(3): 491-497. |
| [11] | 武竞衡, 田光磊, 田萌萌, 陈山林. 170例巨指(趾)患者临床特点分析[J]. 北京大学学报(医学版), 2021, 53(3): 590-593. |
| [12] | 侯宗辰,敖英芳,胡跃林,焦晨,郭秦炜,黄红拾,任爽,张思,谢兴,陈临新,赵峰,皮彦斌,李楠,江东. 慢性踝关节不稳患者足底压力特征及相关因素分析[J]. 北京大学学报(医学版), 2021, 53(2): 279-285. |
| [13] | 李潇,苏家增,张严妍,张丽琪,张亚琼,柳登高,俞光岩. 131I相关唾液腺炎的炎症分级及内镜治疗[J]. 北京大学学报(医学版), 2020, 52(3): 586-590. |
| [14] | 王莹,李明慧,张岩,胡晓燕,马瑞霞. 狼疮性肾炎患者足细胞损伤与肾组织巨噬细胞浸润的关系[J]. 北京大学学报(医学版), 2019, 51(4): 723-727. |
| [15] | 詹颖,杜祎甜,仰浈臻,张春丽,齐宪荣. 紫杉醇微球-原位凝胶的制备及其局部注射的抗肿瘤药效[J]. 北京大学学报(医学版), 2019, 51(3): 477-486. |
|
||