北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (5): 1005-1009. doi: 10.19723/j.issn.1671-167X.2025.05.029
食管胃结合部具有显著空泡状核特征的神经内分泌癌1例
侯卫华1,*, 宋书杰2,*, 石中月3, 刘露2, 金木兰3,*( )
)
- 1. 襄城县人民医院病理科, 河南许昌 461700
2. 解放军联勤保障部队第九八九医院消化内科, 河南平顶山 467099
3. 首都医科大学附属北京朝阳医院病理科, 北京 100020
Neuroendocrine carcinoma with significantly vacuolar nucleus at the esophagogastric junction: A case report
Weihua HOU1, Shujie SONG2, Zhongyue SHI3, Lu LIU2, Mulan JIN3,*( )
)
- 1. Department of Pathology, Xiangcheng County People's Hospital, Xuchang 461700, Henan, China
2. Department of Gastroenterology, 989 Hospital of Joint Logistic Support Force, Pingdingshan 467099, Henan, China
3. Department of Pathology, Beijing Chaoyang Hospital, Capital Medical University, Beijing 100020, China
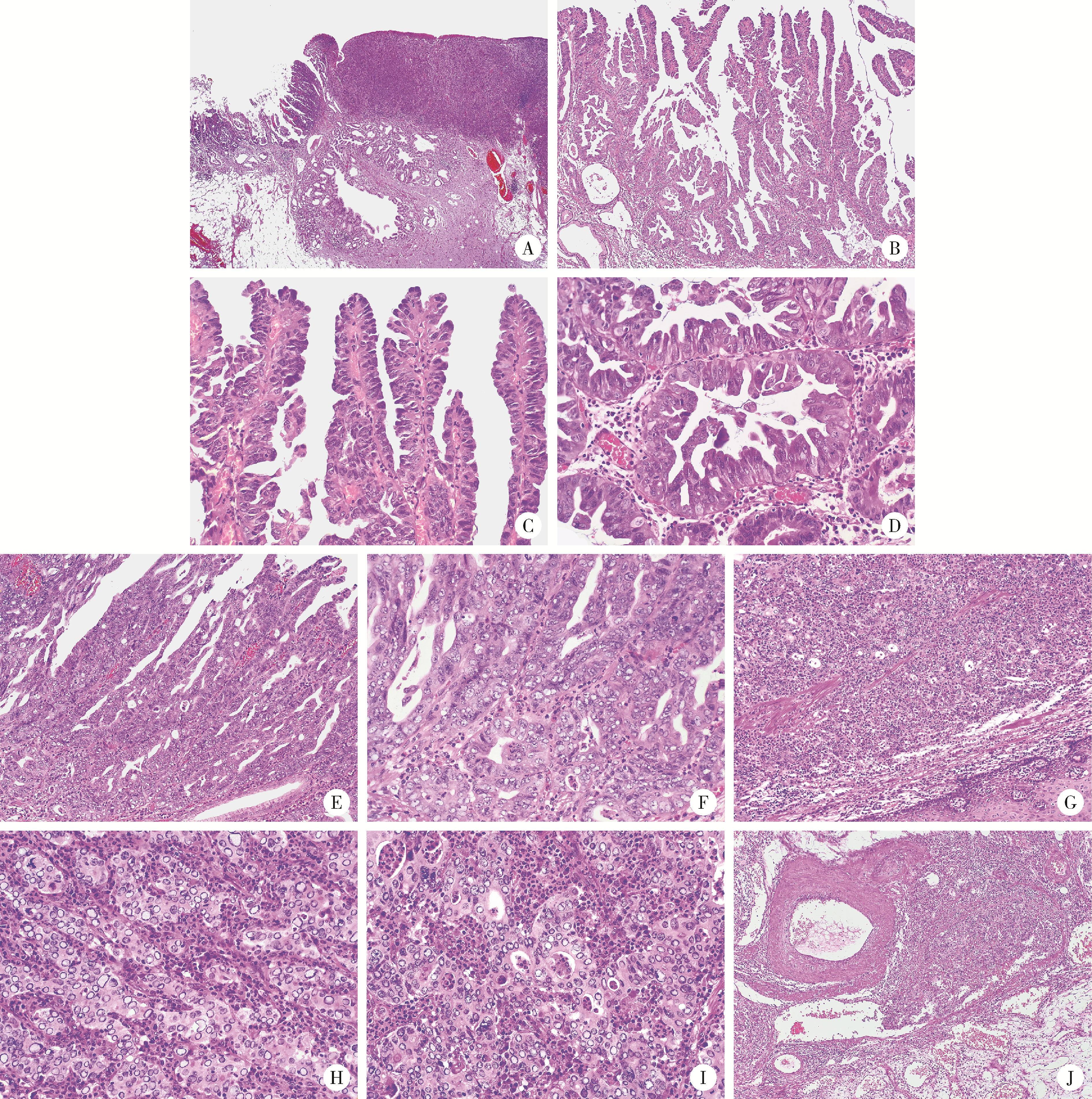
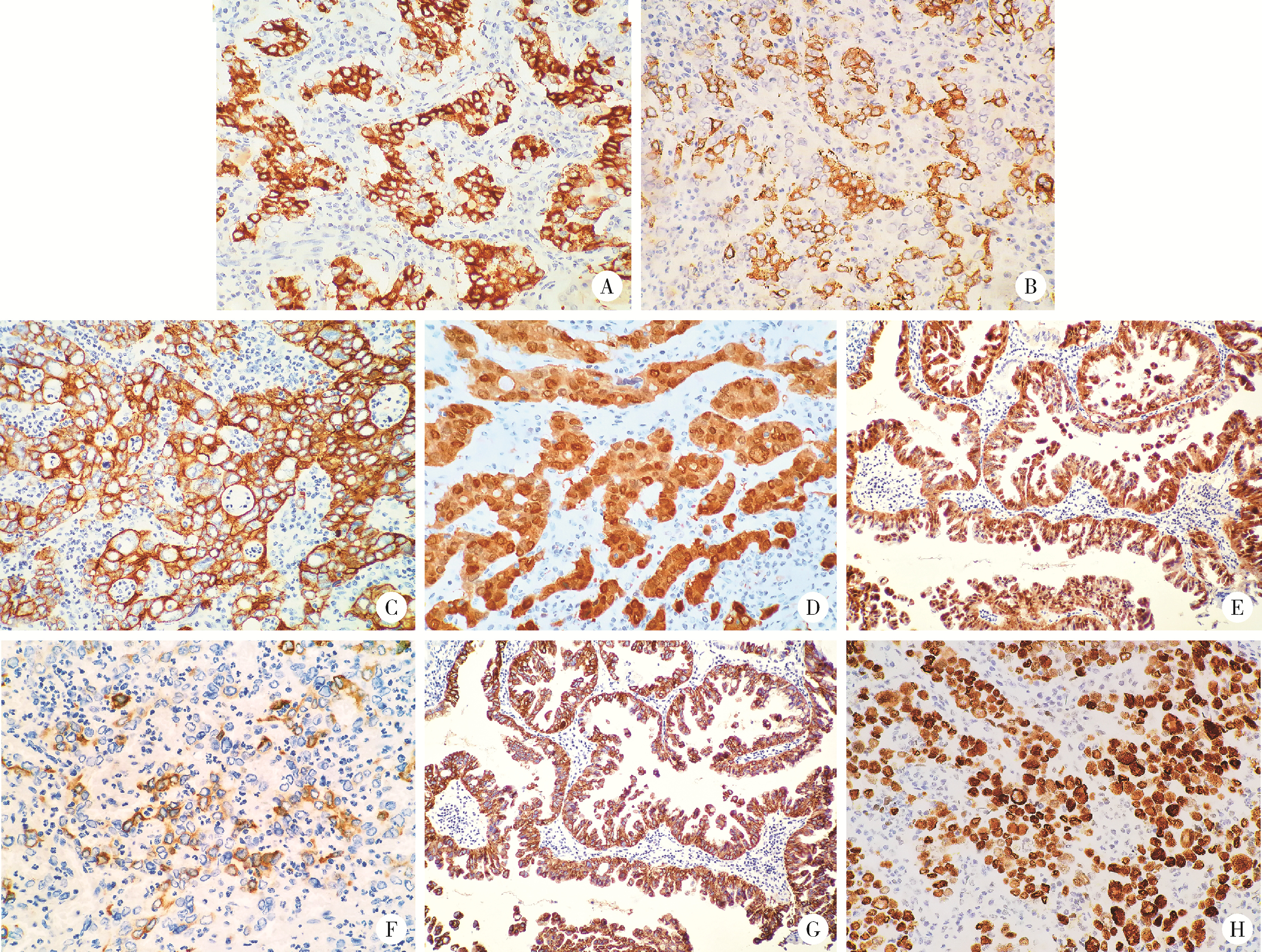
摘要: 以肿瘤细胞中神经内分泌分化标记物的表达为特征的肿瘤被定义为神经内分泌肿瘤。本文报道了1例在食管胃交界处伴有少量乳头状腺癌成分的具有显著空泡核特征的神经内分泌癌(neuroendocrine carcinomas,NECs)。患者为男性,77岁,吞咽不畅1周。内镜检查提示食管胃结合部早期癌,活检诊断为低分化癌,遂行内镜黏膜下剥离术。组织学上,肿瘤呈现出由衬覆靴钉样细胞特征的典型分枝的乳头状结构(高分化),到乳头的衬覆上皮增生形成筛孔状结构(中分化),再到缺乏乳头结构的实性区(低分化)的连续性过程;在此过程中肿瘤细胞核内空泡呈现由轻微到明显,再到显著空泡特征的连续性变化。肿瘤主要由实性区构成(约占95%),细胞单一,细胞体积大,核圆形或卵圆形至不规则形,核呈显著空泡状,空泡较大的核呈圆圈状,空泡内可见少许稀薄的弱嗜碱性或弱嗜酸细颗粒,空泡边缘不光滑。空泡外侧核染色质细颗粒状,核分裂多见(20~30个/mm2),可见非典型核分裂,核仁易见,细胞质弱嗜酸性,细胞的界线不清楚。细胞排列呈巢状、梁索状或弥漫片状,部分排列呈腺管状。黏膜下层静脉内见癌栓;肿瘤内富含毛细血管的间质中伴有大量中性粒细胞浸润。免疫组织化学染色肿瘤实性区细胞突触素(synaptophysin,Syn)和嗜铬粒蛋白A(chromogranin A,CgA)阳性,而乳头状腺癌阴性。黏蛋白5AC(mucin 5AC,MUC5AC)乳头状腺癌弥漫阳性,而肿瘤实性区细胞阳性比例约为10%~15%。总之,该病例展示了NECs空泡状核特征的极端情况,极为罕见,从某种意义上说,扩展了NECs形态谱的边界; 了解这种核的极端空泡状特征有助于做出正确的病理诊断。
中图分类号:
- R735.2
| 1 |
doi: 10.32074/1591-951X-227 |
| 2 |
Klimstra DS, Kloppel G, La Rosa S, et al. Classification of neuroendocrine neoplasms of the digestive system[M]//WHO classification of tumours editorial board. WHO classification of tumours, digestive system tumours. 5th ed. Lyon, France: IARC Press, 2019: 16-19.
|
| 3 |
doi: 10.1007/s11864-022-00968-y |
| 4 |
doi: 10.1007/s12022-016-9432-9 |
| 5 |
doi: 10.3390/jcm9010273 |
| 6 |
doi: 10.3748/wjg.v28.i19.2076 |
| 7 |
doi: 10.3748/wjg.v28.i8.794 |
| 8 |
Lam AK, Kumarasinghe MP. Adenocarcinoma of the oesophagus and oesophagus and oesophagogastric junction NOS[M]//WHO classification of tumours editorial board. WHO classification of tumours, digestive system tumours. 5th ed. Lyon, France: IARC Press, 2019: 38-43.
|
| 9 |
|
| 10 |
doi: 10.1016/j.humpath.2020.12.008 |
| 11 |
doi: 10.1007/s12022-021-09676-z |
| 12 |
|
| 13 |
doi: 10.1097/PAI.0000000000000906 |
| [1] | 李浙民, 季加孚, 李国新, 李子禹, 步召德, 高翔宇, 董迪, 唐磊, 邢晓芳, 贾淑芹, 郭婷, 张连海, 陕飞, 季鑫, 王安强. 胃癌精准诊疗技术的创建与推广[J]. 北京大学学报(医学版), 2025, 57(5): 864-867. |
| [2] | 侯卫华,宋书杰,石中月,金木兰. 幽门螺杆菌阴性早期胃癌的临床病理特征[J]. 北京大学学报(医学版), 2023, 55(2): 292-298. |
| [3] | 刘菊梅,梁丽,张继新,戎龙,张梓怡,吴悠,赵旭东,李挺. 411例早期胃癌及癌前病变内镜黏膜下剥离术标本的病理学评估[J]. 北京大学学报(医学版), 2023, 55(2): 299-307. |
| [4] | 牛占岳,薛艳,张静,张贺军,丁士刚. 胃腺瘤性息肉的内镜和病理特点及癌变的危险因素分析[J]. 北京大学学报(医学版), 2021, 53(6): 1122-1127. |
| [5] | 武颖超,蔡云龙,戎龙,张继新,刘金,汪欣. 早期胃癌淋巴结转移规律及内镜黏膜下剥离术治疗早期胃癌的疗效评价[J]. 北京大学学报(医学版), 2020, 52(6): 1093-1097. |
| [6] | 杨阳,刘毅强,王晓红,季科,李忠武,白健,杨爱蓉,胡颖,韩海勃,李子禹,步召德,吴晓江,张连海,季加孚. 单中心大样本Epstein-Barr病毒相关性胃癌亚型的临床病理及分子特征分析[J]. 北京大学学报(医学版), 2019, 51(3): 451-458. |
| [7] | 刘鑫,张静,王晔,张贺军,丁士刚,周丽雅. 早期胃癌白光内镜下特征分析[J]. 北京大学学报(医学版), 2019, 51(2): 302-306. |
| [8] | 高翔,陈香梅,张婷,张静,陈茉,郭正阳,石岩岩,鲁凤民,丁士刚. 巨噬细胞加帽蛋白与胃癌细胞增殖及迁移能力的关系[J]. 北京大学学报(医学版), 2017, 49(3): 489-494. |
| [9] | 张贺军,刘琳娜,张超,石岩岩,丁士刚. 硫氧还蛋白-1高表达的幽门螺杆菌慢性感染蒙古沙土鼠模型的建立与评价[J]. 北京大学学报(医学版), 2016, 48(5): 766-770. |
| [10] | 李士杰,王警,李子禹,步召德,苏向前,李忠武,吴齐. 内镜黏膜下剥离术在早期胃癌治疗中的应用[J]. 北京大学学报(医学版), 2015, 47(6): 945-951. |
|
||