北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (5): 996-1001. doi: 10.19723/j.issn.1671-167X.2025.05.027
姑息治疗对晚期癌症患者药物使用和医疗资源利用的影响
陈定一1, 杜浩鑫1, 张逸晨1, 王闫飞2, 刘巍2, 焦园园2, 史录文1,3, 管晓东1,3, 卢新璞2,*( )
)
- 1. 北京大学药学院药事管理与临床药学系, 北京 100191
2. 北京大学肿瘤医院暨北京市肿瘤防治研究所, 恶性肿瘤发病机制及转化研究教育部重点实验室, 北京 100142
3. 北京大学医药管理国际研究中心, 北京 100191
Impact of palliative care on medication use and medical utilization in patients with advanced cancer
Dingyi CHEN1, Haoxin DU1, Yichen ZHANG1, Yanfei WANG2, Wei LIU2, Yuanyuan JIAO2, Luwen SHI1,3, Xiaodong GUAN1,3, Xinpu LU2,*( )
)
- 1. Department of Pharmacy Administration and Clinical Pharmacy, Peking University School of Pharmaceutical sciences, Beijing 100191, China
2. Key Laboratory of Carcinogenesis and Translational Research(Ministry of Education/Beijing), Peking University Cancer Hospital & Institute, Beijing 100142, China
3. International Research Center for Medicinal Administration, Peking University, Beijing 100191, China
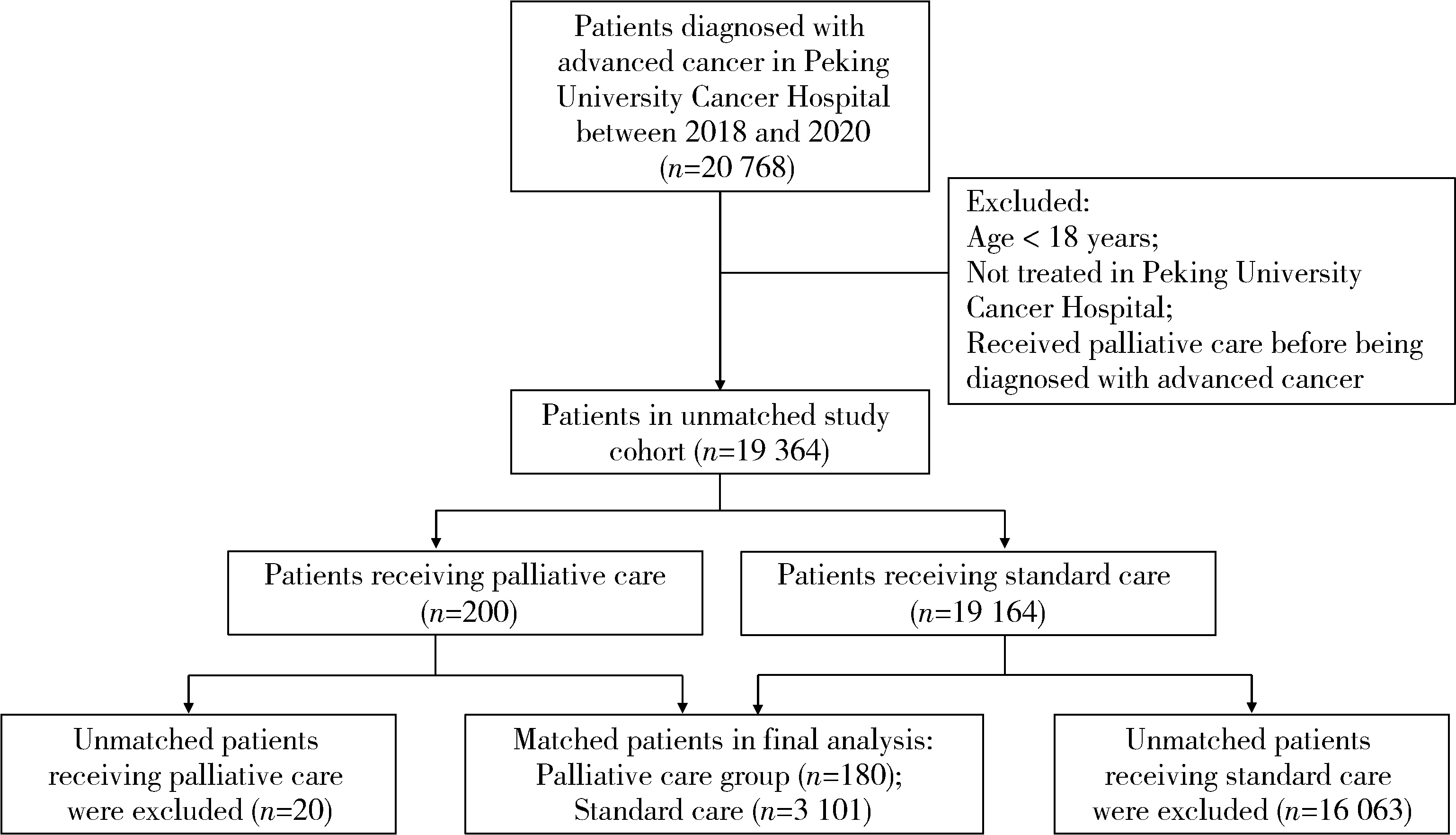
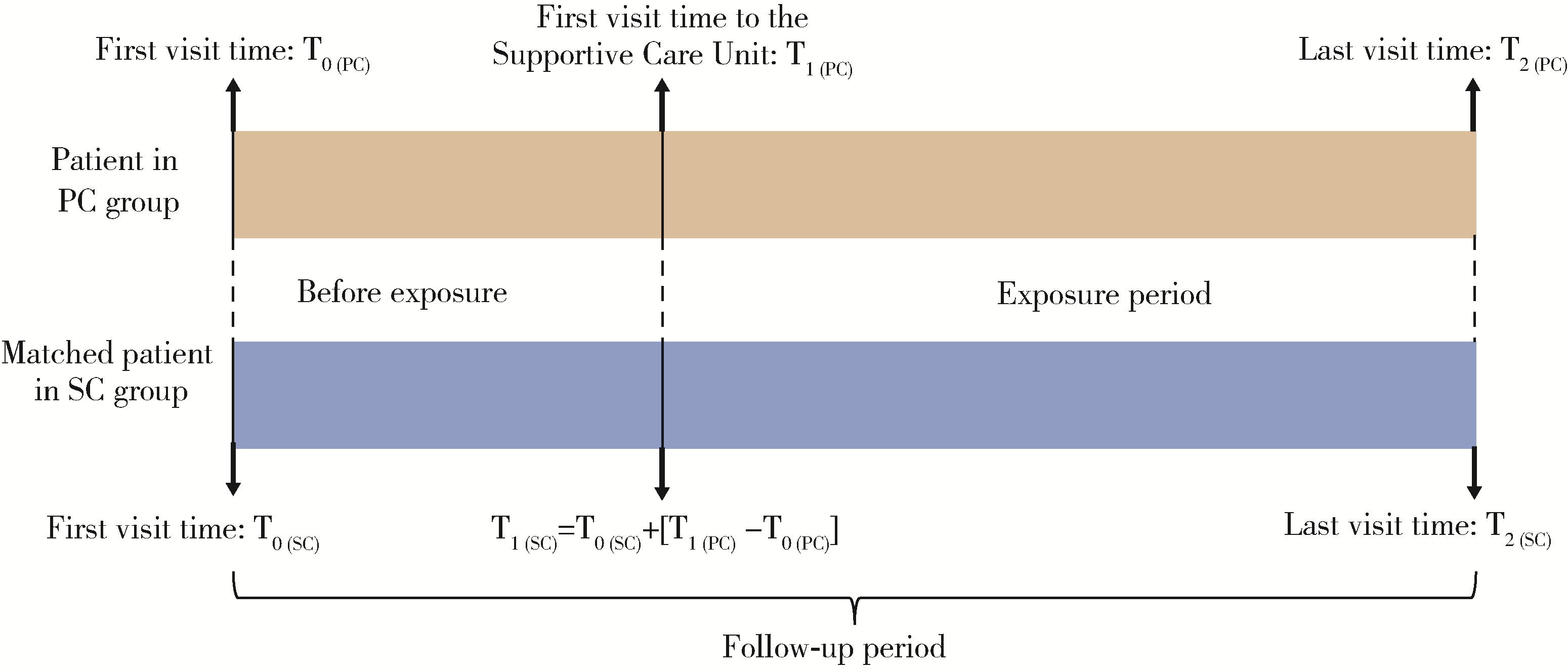
摘要: 目的: 评价姑息治疗对晚期癌症患者药物使用、医疗服务利用及医疗费用的影响。方法: 基于2018—2020年北京大学肿瘤医院患者就诊记录,采用广义精确匹配法构建包括姑息治疗与常规治疗两组患者队列,分别选取阿片类镇痛药物月均使用量、住院率、重症监护室(intensive care unit,ICU)率、手术率、月均总费用等指标评价药物使用、医疗服务利用与医疗费用,采用卡方检验和Wilcoxon符号秩检验比较暴露前后两组患者结局指标差异及姑息治疗组患者结局指标变化,采用倍差法测算姑息治疗对患者各结局指标的净影响值。结果: 最终纳入180例姑息治疗组患者与3 101例常规治疗组患者,组间匹配效果良好(L1 < 0.1)。暴露前后,姑息治疗组阿片类药物月均使用量均显著高于常规治疗组(暴露前:0.3 DDD/人月vs. 0.1 DDD/人月,P < 0.01;暴露后:0.7 DDD/人月vs. 0.1 DDD/人月,P < 0.01;DDD为限定日剂量,defined daily dose),姑息治疗显著增加了患者的阿片类药物月均使用量(增加0.3 DDD/人月,P < 0.01)。暴露后,姑息治疗组住院率和手术率均显著低于常规治疗组(48.9% vs. 74.3%,3.9% vs. 8.8%,P均 < 0.01),两组患者的ICU率相似(1.1% vs. 1.6%,P=0.634)。姑息治疗显著降低了患者的住院率、ICU率和手术率,分别降低25.6%、4.9%和14.5%(P均 < 0.01)。暴露前后,姑息治疗组月均总费用均略高于常规治疗组(暴露前:20 092.3元vs. 19 132.8元,P=0.725;暴露后:9 719.8元vs. 8 818.8元,P=0.165),但姑息治疗对患者的月均总费用无显著影响(增加2 208.8元,P=0.316)。结论: 姑息治疗可以增加晚期癌症患者阿片类药物使用量,降低住院率、ICU率和手术率,而对患者医疗费用无显著影响。
中图分类号:
- R730.5
| 1 |
WHO. Detail of Palliative Care[EB/OL]. (2020-08-05)[2022-05-01]. https://www.who.int/news-room/fact-sheets/detail/palliative-care.
|
| 2 |
刘佩, 蒲嘉泽, 黄雯. 晚期恶性肿瘤患者采用姑息治疗的临床效果[J]. 临床合理用药杂志, 2021, 14 (8): 169- 170.
|
| 3 |
赵杰. 安宁疗护和姑息治疗对直肠癌晚期患者临终期生活质量的影响[J]. 中国肛肠病杂志, 2022, 42 (3): 62- 63.
|
| 4 |
郭敏, 孟华, 张庆波. 姑息治疗老年恶性肿瘤患者的临床效果观察[J]. 中国社区医师, 2021, 37 (10): 15- 16.
|
| 5 |
doi: 10.1200/JCO.19.00013 |
| 6 |
王茜, 林天华, 张仑. 晚期癌症患者的姑息护理研究进展分析[J]. 实用临床护理学电子杂志, 2018, 3 (15): 193- 198.
|
| 7 |
doi: 10.1200/JOP.2017.020883 |
| 8 |
doi: 10.1200/EDBK_175474 |
| 9 |
宁晓红. 中国缓和医疗的发展和思考[J]. 中国医学科学院学报, 2019, 41 (5): 723- 725.
|
| 10 |
张丽艳, 沈美玲. 积极养老视角下我国安宁疗护政策研究——基于2012-2019年政策文本分析[J]. 科学与管理, 2021, 41 (2): 49- 54.
|
| 11 |
|
| 12 |
doi: 10.2478/jccm-2022-0009 |
| 13 |
|
| 14 |
doi: 10.1089/pmr.2020.0051 |
| 15 |
doi: 10.1093/pan/mpr013 |
| 16 |
doi: 10.1159/000500783 |
| 17 |
doi: 10.1097/j.pain.0000000000001459 |
| 18 |
doi: 10.1089/jpm.2007.0055 |
| 19 |
doi: 10.1001/jama.2014.16153 |
| 20 |
doi: 10.1016/j.jpainsymman.2015.12.340 |
| 21 |
王薇. 北京市癌痛治疗现状调查分析及草乌甲素治疗轻中度癌痛的临床研究[D]. 北京: 中国中医科学院, 2019.
|
| 22 |
海峡两岸医药卫生交流协会全科医学分会. 姑息治疗与安宁疗护基本用药指南[J]. 中国全科医学, 2021, 24 (14): 1717- 1734.
|
| 23 |
NCCN. NCCN clinical practice guidelines in oncology: Palliative care[M/OL]. (2020-02-27)[2022-03-04]. https://www.nccn.org/professionals/physician_gls/pdf/palliative_enhanced.pdf.
|
| 24 |
doi: 10.1016/j.currproblcancer.2020.100655 |
| 25 |
doi: 10.1001/jama.2020.14205 |
| 26 |
doi: 10.1200/JCO.2012.43.6055 |
| 27 |
doi: 10.1001/jama.2014.14950 |
| 28 |
doi: 10.1016/S2213-2600(14)70226-7 |
| 29 |
doi: 10.1186/s12904-020-00579-0 |
| 30 |
杨晓燕. ICU危重患者机械通气后常见并发症护理[J]. 医药论坛杂志, 2009, 30 (10): 127- 128.
|
| 31 |
荆明远. 腹腔镜胃癌手术常见并发症及其防治对策[J]. 中国卫生标准管理, 2014, 5 (20): 120- 121.
|
| 32 |
舒芳芳, 包磊, 朱蓓, 等. 成人择期手术患者术前焦虑现状、恐惧焦点及影响因素的横断面调查研究[J]. 实用临床医药杂志, 2022, 26 (6): 72-76, 108.
|
| 33 |
doi: 10.1513/AnnalsATS.202001-038OC |
| [1] | 杨小勇, 张帆, 马潞林, 刘承. 前列腺导管腺癌临床特征及腺外侵犯的影响因素[J]. 北京大学学报(医学版), 2025, 57(5): 956-960. |
| [2] | 宁家昕, 王浩然, 罗书航, 敬吉波, 王建业, 侯惠民, 刘明. 氧化应激相关基因与前列腺癌关系的多组学分析[J]. 北京大学学报(医学版), 2025, 57(4): 633-643. |
| [3] | 王泽远, 于栓宝, 郑浩轲, 陶金, 范雅峰, 张雪培. 基于临床特征和多参数MRI的前列腺癌盆腔淋巴结转移的术前预测模型[J]. 北京大学学报(医学版), 2025, 57(4): 684-691. |
| [4] | 缪祺, 洪保安, 张学舟, 孙志鹏, 王维, 王宇轩, 薄予轩, 赵佳晖, 张宁. 膀胱癌合并冠心病患者行经尿道膀胱肿瘤切除术围手术期抗血小板药物管理[J]. 北京大学学报(医学版), 2025, 57(4): 698-703. |
| [5] | 刘帅, 刘茁, 管允鹤, 王国良, 田晓军, 张洪宪, 刘磊, 马潞林, 张树栋. 机器人辅助腹腔镜下腔静脉节段性切除术治疗肾肿瘤瘤栓侵犯血管壁[J]. 北京大学学报(医学版), 2025, 57(4): 796-802. |
| [6] | 韩丹, 次仁央金, 李秋红, 李军. 高海拔地区结直肠良恶性肿瘤患者肠道菌群差异及其与低海拔地区正常人群的比较[J]. 北京大学学报(医学版), 2025, 57(3): 578-583. |
| [7] | 杨源源, 张珊珊, 俞光岩, 杨辉俊, 杨宏宇. 部分下颌下腺切除术治疗下颌下腺良性肿瘤的临床效果[J]. 北京大学学报(医学版), 2025, 57(2): 334-339. |
| [8] | 田素青, 孙海涛, 赵田地, 王巍. 6D治疗床辅助影像引导下放射治疗头颈部肿瘤摆位误差分析[J]. 北京大学学报(医学版), 2024, 56(6): 1097-1100. |
| [9] | 李志存, 吴天俣, 梁磊, 范宇, 孟一森, 张骞. 穿刺活检单针阳性前列腺癌术后病理升级的危险因素分析及列线图模型构建[J]. 北京大学学报(医学版), 2024, 56(5): 896-901. |
| [10] | 刘家骏, 刘国康, 朱玉虎. 免疫相关性重症肺炎1例[J]. 北京大学学报(医学版), 2024, 56(5): 932-937. |
| [11] | 黄教悌,胡菁,韩博. 治疗相关神经内分泌前列腺癌机制研究与靶向治疗新进展[J]. 北京大学学报(医学版), 2024, 56(4): 557-561. |
| [12] | 田宇轩,阮明健,刘毅,李德润,吴静云,沈棋,范宇,金杰. 双参数MRI改良PI-RADS评分4分和5分病灶的最大径对临床有意义前列腺癌的预测效果[J]. 北京大学学报(医学版), 2024, 56(4): 567-574. |
| [13] | 姚凯烽,阮明健,李德润,田宇轩,陈宇珂,范宇,刘毅. 靶向穿刺联合区域系统穿刺对PI-RADS 4~5分患者的前列腺癌诊断效能[J]. 北京大学学报(医学版), 2024, 56(4): 575-581. |
| [14] | 欧俊永,倪坤明,马潞林,王国良,颜野,杨斌,李庚午,宋昊东,陆敏,叶剑飞,张树栋. 肌层浸润性膀胱癌合并中高危前列腺癌患者的预后因素[J]. 北京大学学报(医学版), 2024, 56(4): 582-588. |
| [15] | 王滨帅,邱敏,张前进,田茂锋,刘磊,王国良,陆敏,田晓军,张树栋. 6例肾尤文肉瘤伴静脉瘤栓的诊治[J]. 北京大学学报(医学版), 2024, 56(4): 636-639. |
|
||