北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (1): 113-118. doi: 10.19723/j.issn.1671-167X.2020.01.018
下颌后缩伴颞下颌关节重度骨关节病患者正颌术后颌骨稳定性及髁突体积变化的评价
- 北京大学口腔医学院·口腔医院,口腔颌面外科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室,北京 100081
Evaluation of mandibular stability and condylar volume after orthognathic surgery in patients with severe temporomandibular joint osteoarthrosis
Lei HOU,Guo-hua YE,Xiao-jing LIU,Zi-li LI( )
)
- Department of Oral and Maxillofacial Surgery,Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
摘要:
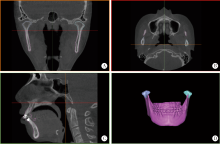
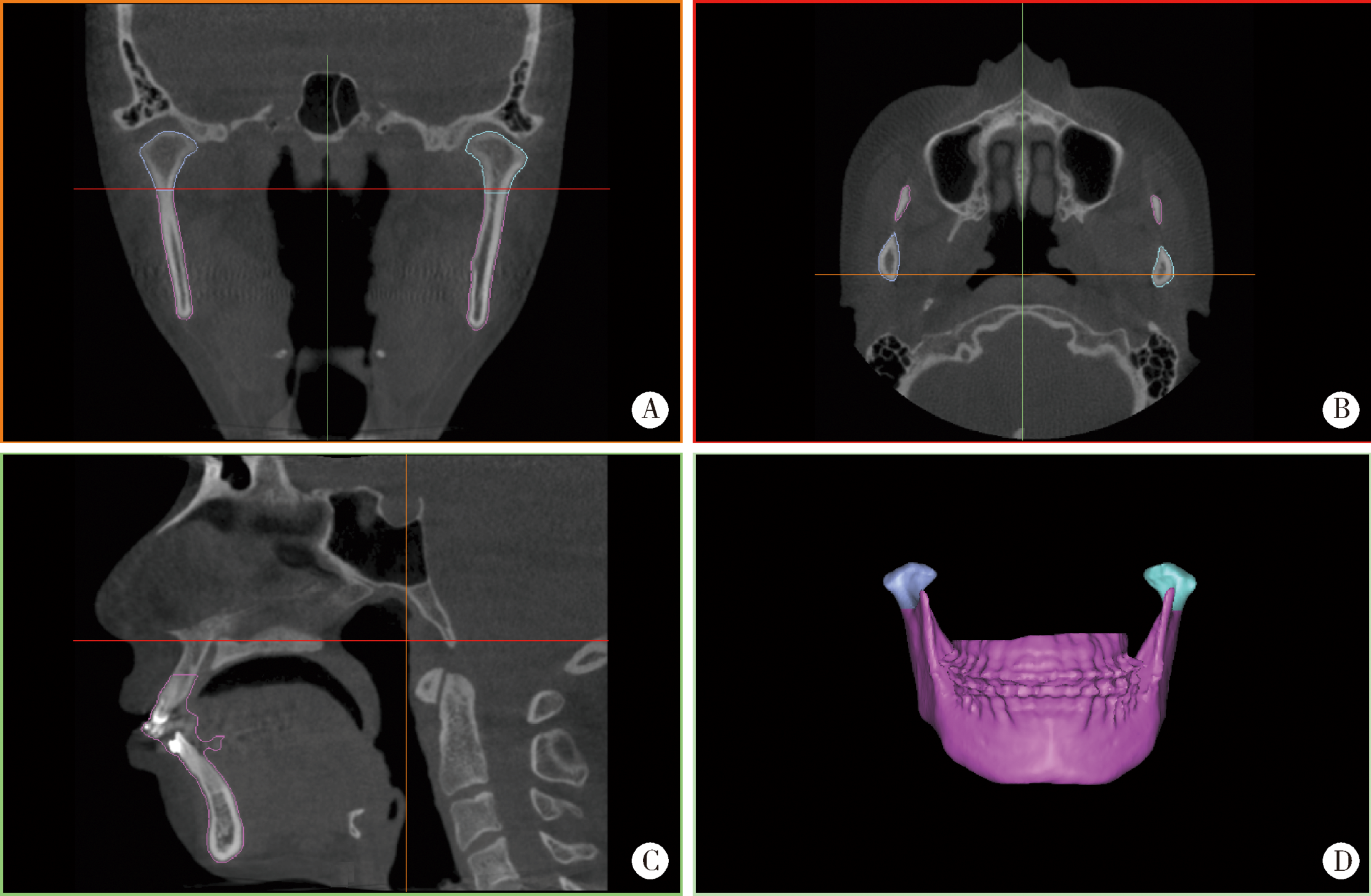
目的:探讨下颌后缩伴颞下颌关节重度骨关节病患者正颌手术前的髁突表面骨质结构完整性对术后颌骨稳定性及髁突体积变化的影响。方法:选择2014年至2019年就诊于北京大学口腔医院诊断为下颌后缩畸形伴颞下颌关节重度骨关节病,并接受正颌手术且满足条件的患者37例进行回顾性分析,其中男性1例,女性36例,年龄(28.03±6.52)岁(21~34岁),依据术前髁突表面骨质情况分为表面光滑组和表面不光滑组,其中光滑组19例,不光滑组18例,分别于术前1周,术后1周、3个月、6个月及1年拍摄头颅侧位片及锥形束CT(cone-beam computed tomography,CBCT), 对头颅侧位片进行坐标系建立及头影测量分析明确术后颌骨稳定性,对CBCT进行三维重建分割获取髁突的三维模型及体积,评价术后髁突体积的变化,通过CBCT影像资料评估术后髁突骨质改变情况,明确术后髁突骨质改变与颌骨稳定性的相关性,应用SPSS 20.0软件,采用Fisher确切概率法、Spearman相关系数分析及Mann-Whitney检验对所获数据进行统计学分析。结果:术前髁突表面光滑组在术后3个月(T1)、术后6个月(T2)、术后12个月(T3)颌骨复发率分别为36.85%、47.37%、42.11%,术前髁突表面不光滑组T1、T2、T3颌骨复发率分别为27.78%、44.44%、55.56%,两组在各时间段的复发率差异无统计学意义,术前髁突表面光滑组与不光滑组在各时间段的髁突体积的变化差异无统计学意义,不光滑组术后3个月的髁突进展与颌骨的稳定性有相关性。结论:对于下颌后缩伴颞下颌关节重度骨关节病且术前观察髁突一年无显著变化者,术前髁突表面是否光滑对于术后颌骨的稳定性没有确切影响,对于术前髁突不光滑的重度骨关节病患者,术后3个月出现髁突吸收会引起正颌术后颌骨位置的不稳定,术前髁突表面是否光滑对术后髁突体积的改建没有明确的影响。
中图分类号:
- R782
| [1] | Rocha VA, Neto AI, Rebello IM , et al. Skeletal stability in orthognathic surgery: evaluation of methods of rigid internal fixation after counterclockwise rotation in patients with class Ⅱ deformities[J]. Br J Oral Maxillofac Surg, 2015,53(8):730-735. |
| [2] | Krisjane Z, Urtane I, Krumina G , et al. The prevalence of TMJ osteoarthritis in asymptomatic patients with dentofacial deformities: a cone-beam CT study[J]. Int J Oral Maxillofac Surg, 2012,41(6):690-695. |
| [3] | Chen S, Lei J, Fu KY , et al. Cephalometric analysis of the facial skeletal morphology of female patients exhibiting skeletal class ii deformity with and without temporomandibular joint osteoarthrosis[J]. PLoS One, 2015,10(10):e0139743. |
| [4] | Nogami S, Yamauchi K, Satomi N , et al. Risk factors related to aggressive condylar resorption after orthognathic surgery for females: retrospective study[J]. Cranio, 2017,35(4):250-258. |
| [5] | Posnick JC, Fantuzzo JJ . Idiopathic condylar resorption: current clinical perspectives[J]. J Oral Maxillofac Surg, 2007,65(8):1617-1623. |
| [6] | Honey OB, Scarfe WC, Hilgers MJ , et al. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparisons with panoramic radiology and linear tomography[J]. Am J Orthod Dentofacial Orthop, 2007,132(4):429-438. |
| [7] | Bayram M, Kayipmaz S, Sezgin OS , et al. Volumetric analysis of the mandibular condyle using cone beam computed tomography[J]. Eur J Radiol, 2012,81(8):1812-1816. |
| [8] | Kadesjo N, Benchimol D, Falahat B , et al. Evaluation of the effective dose of cone beam CT and multislice CT for temporomandibular joint examinations at optimized exposure levels [J]. Dentomaxillofac Radiol, 2015, 44(8): 20150041[2019-09-10]. |
| [9] | Tecco S, Saccucci M, Nucera R , et al. Condylar volume and surface in Caucasian young adult subjects[J]. BMC Med Imaging, 2010,31(10):28. |
| [10] | Xi T, Schreurs R, van Loon B , et al. 3D analysis of condylar remodelling and skeletal relapse following bilateral sagittal split advancement osteotomies[J]. J Craniomaxillofac Surg, 2015,43(4):462-468. |
| [11] | Jung J, Kim J H, Lee J W , et al. Three-dimensional volumetric analysis of condylar head and glenoid cavity after mandibular advancement[J]. J Craniomaxillofac Surg, 2018,46(9):1470-1475. |
| [12] | da Silva RJ, Valadares Souza CV, Souza GA , et al. Changes in condylar volume and joint spaces after orthognathic surgery[J]. Int J Oral Maxillofac Surg, 2018,47(4):511-517. |
| [13] | 雷杰, 秦思思, 傅开元 . 锥体束CT影像评估颞下颌关节重度骨关节病髁突骨改变的稳定性[J]. 中华口腔正畸学杂志, 2017,24(4):212-216. |
| [14] | Alexiou K, Stamatakis H, Tsiklakis K . Evaluation of the severity of temporomandibular joint osteoarthritic changes related to age using cone beam computed tomography[J]. Dentomaxillofac Radiol, 2009,38(3):141-147. |
| [15] | Ahmad M, Hollender L, Anderson Q , et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2009,107(6):844-860. |
| [16] | Talaat W, Al Bayatti S, Al Kawas S . CBCT analysis of bony changes associated with temporomandibular disorders[J]. Cranio, 2016,34(2):88-94. |
| [17] | Tamimi D, Jalali E, Hatcher D . Temporomandibular joint imaging[J]. Radiol Clin North Am, 2018,56(1):157-175. |
| [18] | Proffit WR, Turvey TA, Phillips C . The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension[J]. Head Face Med, 2007,30(3):21. |
| [19] | Massilla Mani F, Sivasubramanian SS . A study of temporoman-dibular joint osteoarthritis using computed tomographic imaging[J]. Biomed J, 2016,39(3):201-206. |
| [20] | Joss CU, Vassalli IM . Stability after bilateral sagittal split osteotomy advancement surgery with rigid internal fixation: a systematic review[J]. J Oral Maxillofac Surg, 2009,67(2):301-313. |
| [21] | Zarb GA, Carlsson GE . Temporomandibular disorders: osteoarthritis[J]. J Orofac Pain, 1999,13(4):295-306. |
| [22] | Hoppenreijs TJ, Stoelinga PJ, Grace KL , et al. Long-term evaluation of patients with progressive condylar resorption following orthognathic surgery[J]. Int J Oral Maxillofac Surg, 1999,28(6):411-418. |
| [23] | Kobayashi T, Izumi N, Kojima T , et al. Progressive condylar resorption after mandibular advancement[J]. Br J Oral Maxillofac Surg, 2012,50(2):176-180. |
| [24] | Hussain AM, Packota G, Major PW , et al. Role of different imaging modalities in assessment of temporomandibular joint erosions and osteophytes: a systematic review[J]. Dentomaxillofac Radiol, 2008,37(2):63-71. |
| [25] | Valladares-Neto J, Cevidanes LH, Rocha WC , et al. TMJ response to mandibular advancement surgery: an overview of risk factors[J]. J Appl Oral Sci, 2014,22(1):2-14. |
| [26] | He Z, Ji H, Du W , et al. Management of condylar resorption before or after orthognathic surgery: a systematic review[J]. J Craniomaxillofac Surg, 2019,47(7):1007-1014. |
| [27] | 秦思思, 雷杰, 傅开元 . 锥形束CT评估颞下颌关节重度骨关节病患者正颌术后髁突骨质再吸收[J]. 现代口腔医学杂志, 2016,30(5):261-265. |
| [28] | Haas Junior OL, Guijarro-Martinez R, de Sousa Gil AP , et al. Hierarchy of surgical stability in orthognathic surgery: overview of systematic reviews[J]. Int J Oral Maxillofac Surg, 2019,48(11):1415-1433. |
| [29] | Bailey L, Cevidanes LH, Proffit WR . Stability and predictability of orthognathic surgery[J]. Am J Orthod Dentofacial Orthop, 2004,126(3):273-277. |
| [30] | Franco AA, Cevidanes LH, Phillips C , et al. Long-term 3-dimensional stability of mandibular advancement surgery[J]. J Oral Maxillofac Surg, 2013,71(9):1588-1597. |
| [1] | 李雨清,王飚,乔鹏,王玮,关星. 经耻骨后尿道中段悬吊带术治疗女性复发性压力性尿失禁的中长期疗效[J]. 北京大学学报(医学版), 2024, 56(4): 600-604. |
| [2] | 姚中强,李常虹,李欣艺,郭苇,翟佳羽,刘蕊,魏慧,穆荣. 抗磷脂酰丝氨酸/凝血酶原抗体与不明原因复发性流产的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 1058-1061. |
| [3] | 陈素华,杨军,陈新,杨辰龙,孙建军,林国中,于涛,杨欣,韩芸峰,吴超,司雨,马凯明. 大型、巨大型上矢状窦中后1/3侵犯颅外复发脑膜瘤的手术治疗[J]. 北京大学学报(医学版), 2022, 54(5): 1006-1012. |
| [4] | 王跃,张爽,张虹,梁丽,徐玲,程元甲,段学宁,刘荫华,李挺. 激素受体阳性/人表皮生长因子受体2阴性乳腺癌临床病理特征及预后[J]. 北京大学学报(医学版), 2022, 54(5): 853-862. |
| [5] | 森本智惠子,王益勤,周蓉,王建六. 子宫内膜非典型增生及子宫内膜癌患者保留生育功能治疗的临床研究[J]. 北京大学学报(医学版), 2022, 54(5): 936-942. |
| [6] | 刘磊,秦艳春,王国良,张树栋,侯小飞,马潞林. 嗜铬细胞瘤和副神经节瘤二次手术策略[J]. 北京大学学报(医学版), 2021, 53(4): 793-797. |
| [7] | 于焕斌,伍文杰,吕晓鸣,石妍,郑磊,张建国. 125I粒子近距离治疗外放疗后复发唾液腺癌[J]. 北京大学学报(医学版), 2020, 52(5): 919-923. |
| [8] | 熊盛炜,王杰,朱伟杰,程嗣达,张雷,李学松,周利群. 二次肾盂成形术在复发性肾盂输尿管连接部梗阻中的研究进展[J]. 北京大学学报(医学版), 2020, 52(4): 794-798. |
| [9] | 张旭初,张建华,王荣福,范岩,付占立,闫平,赵光宇,白艳霞. 18F-FDG PET/CT联合多种肿瘤标志物在结直肠中分化腺癌术后复发及转移中的应用价值[J]. 北京大学学报(医学版), 2019, 51(6): 1071-1077. |
| [10] | 唐琦,林榕城,姚林,张争,郝瀚,张崔建,蔡林,李学松,何志嵩,周利群. 肾癌术后局部复发患者的临床病理特征及预后分析[J]. 北京大学学报(医学版), 2019, 51(4): 628-631. |
| [11] | 朱冉,倪照军,张顺,庞良俊,王传升,鲍彦平,孙洪强. 临床特征对酒精依赖复发的影响:前瞻性队列研究[J]. 北京大学学报(医学版), 2019, 51(3): 519-524. |
| [12] | 王秀婧,张怡美,周彦恒. 骨性Ⅲ类错牙合畸形患者正畸-正颌联合治疗的稳定性[J]. 北京大学学报(医学版), 2019, 51(1): 86-92. |
| [13] | 李欣艺,赵金霞,刘湘源. 抗磷脂抗体相关性复发性流产的诊治:附75例抗磷脂综合征患者妊娠期用药和结局分析[J]. 北京大学学报(医学版), 2018, 50(6): 956-961. |
| [14] | 邢云超,熊耕砚,方东,张争,蔡林,张雷,何志嵩,李学松,周利群. 上尿路尿路上皮癌术前预后相关因素分析及初步风险分层模型构建[J]. 北京大学学报(医学版), 2016, 48(6): 1032-1037. |
| [15] | 陈硕, 刘筱菁, 李自力, 梁成, 王晓霞, 傅开元, 伊彪. 下颌后缩畸形患者正颌外科术后髁突改建的三维影像评价[J]. 北京大学学报(医学版), 2015, 47(4): 703-707. |
|
||