北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (5): 853-862. doi: 10.19723/j.issn.1671-167X.2022.05.013
激素受体阳性/人表皮生长因子受体2阴性乳腺癌临床病理特征及预后
王跃1,张爽1,张虹1,梁丽1,徐玲2,程元甲2,段学宁2,刘荫华2,李挺1,*( )
)
- 1. 北京大学第一医院病理科,北京 100034
2. 北京大学第一医院乳腺疾病中心,北京 100034
Clinicopathological features and prognosis of hormone receptor-positive/human epidermal growth factor receptor 2-negative breast cancer
Yue WANG1,Shuang ZHANG1,Hong ZHANG1,Li LIANG1,Ling XU2,Yuan-jia CHENG2,Xue-ning DUAN2,Yin-hua LIU2,Ting LI1,*( )
)
- 1. Department of Pathology, Peking University First Hospital, Beijing 100034, China
2. Breast Disease Center, Peking University First Hospital, Beijing 100034, China
摘要:
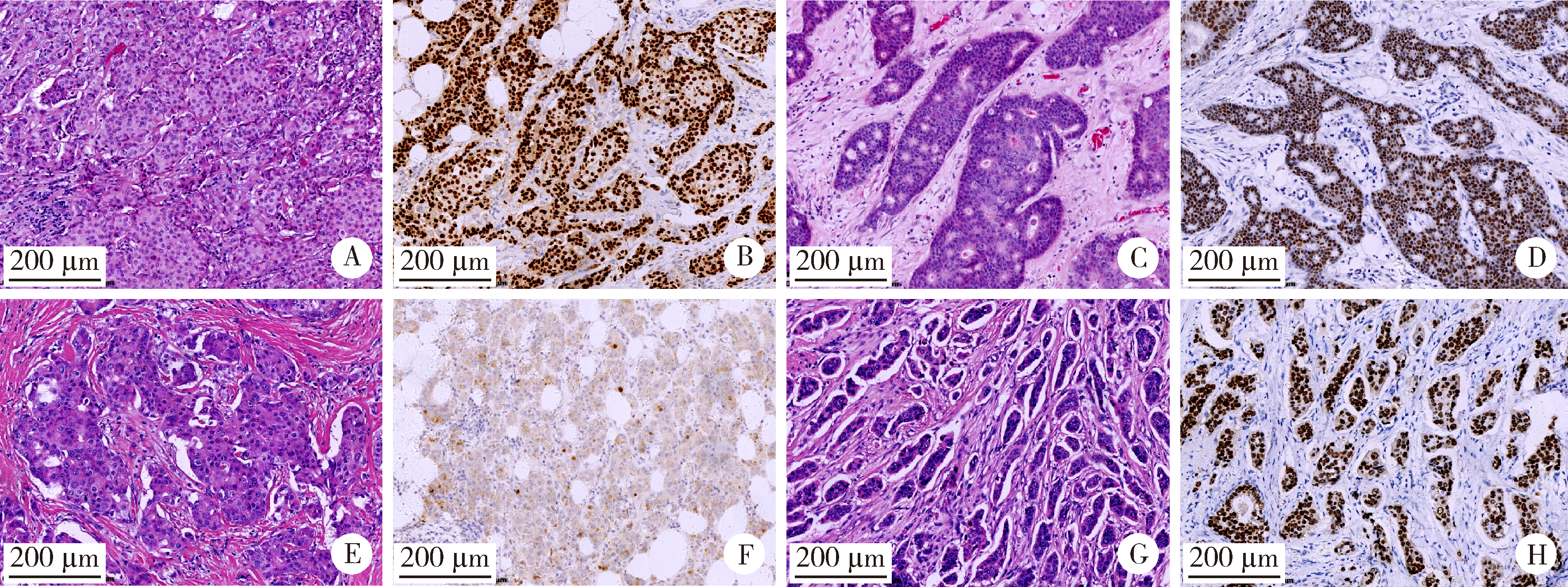
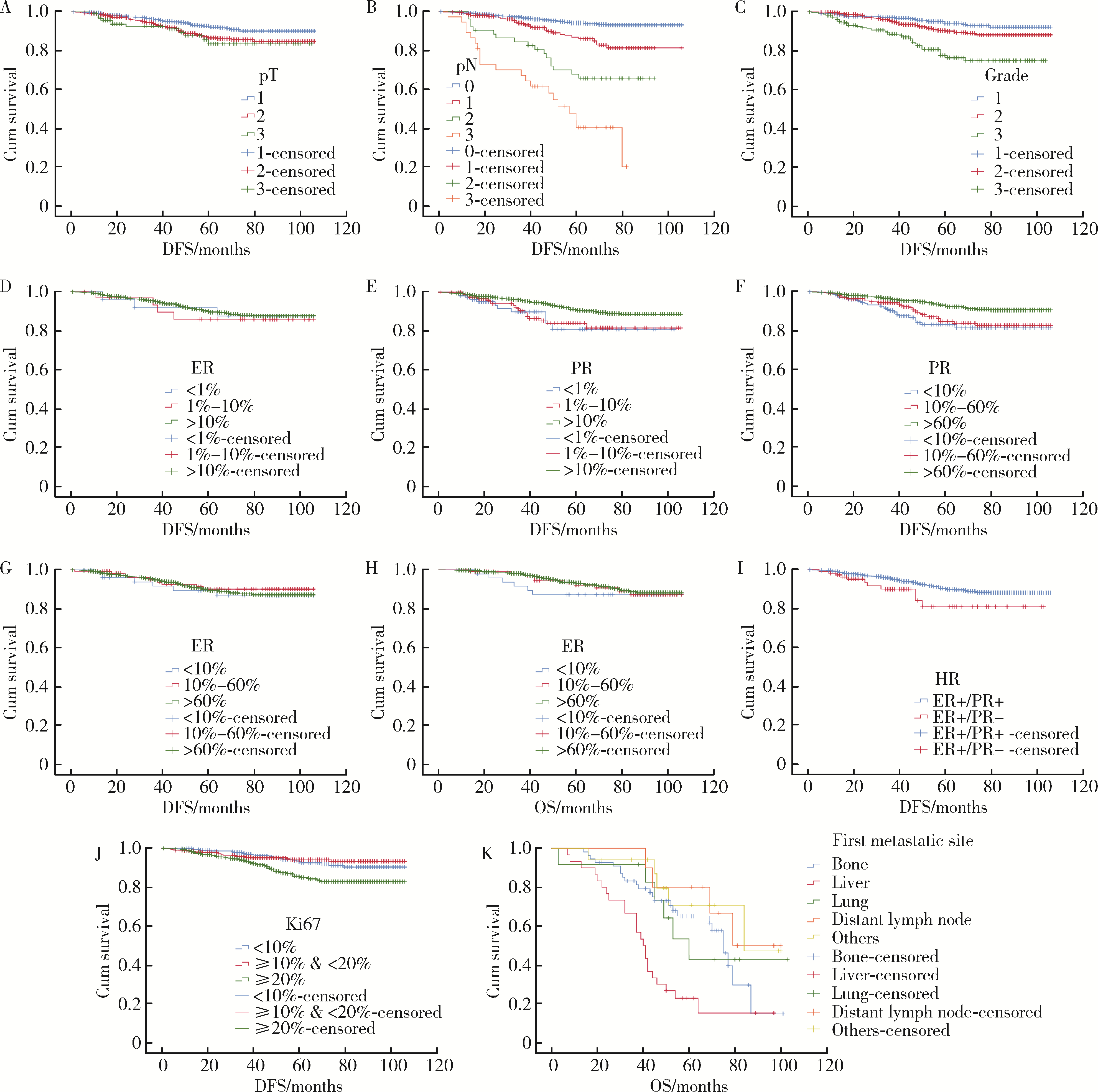
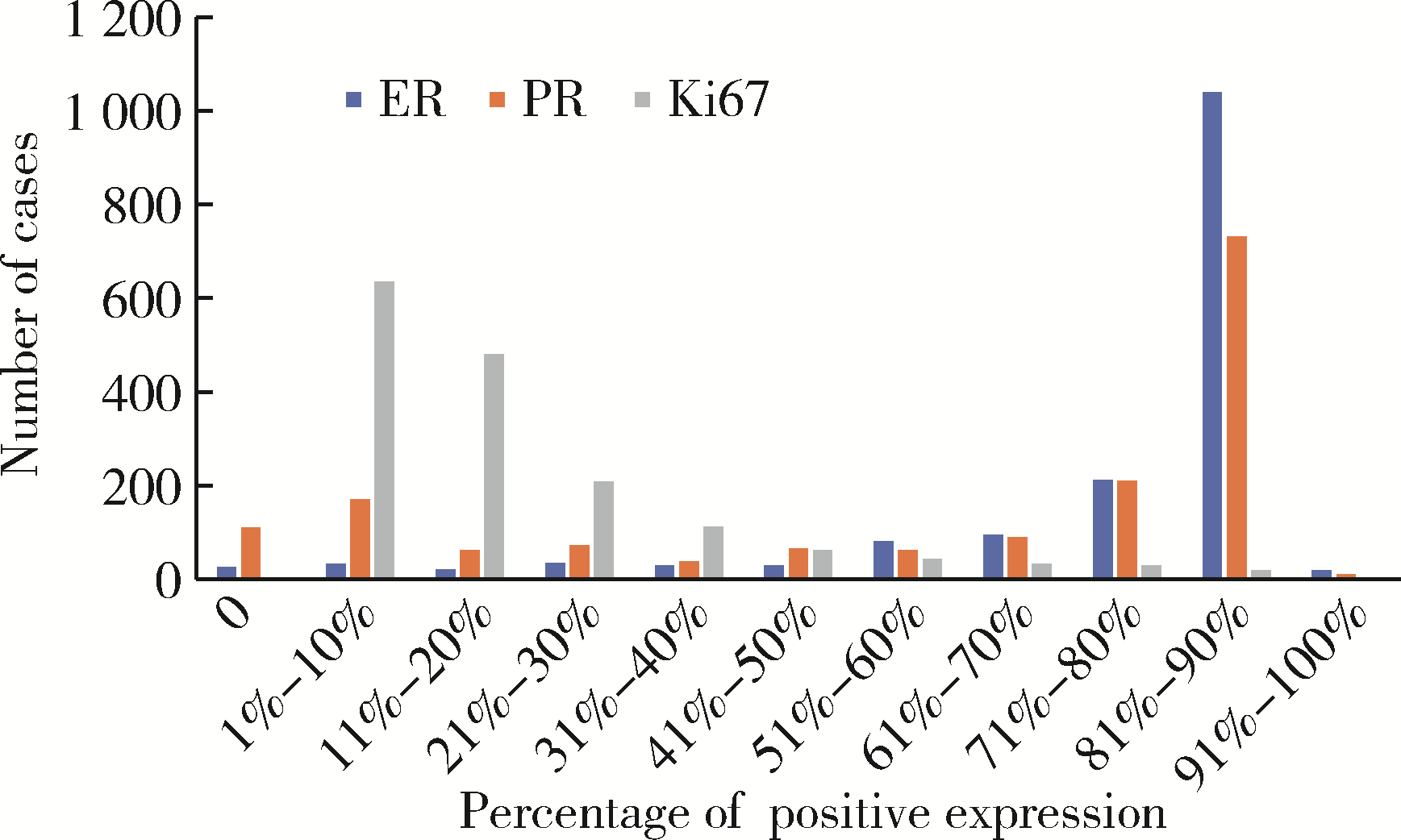
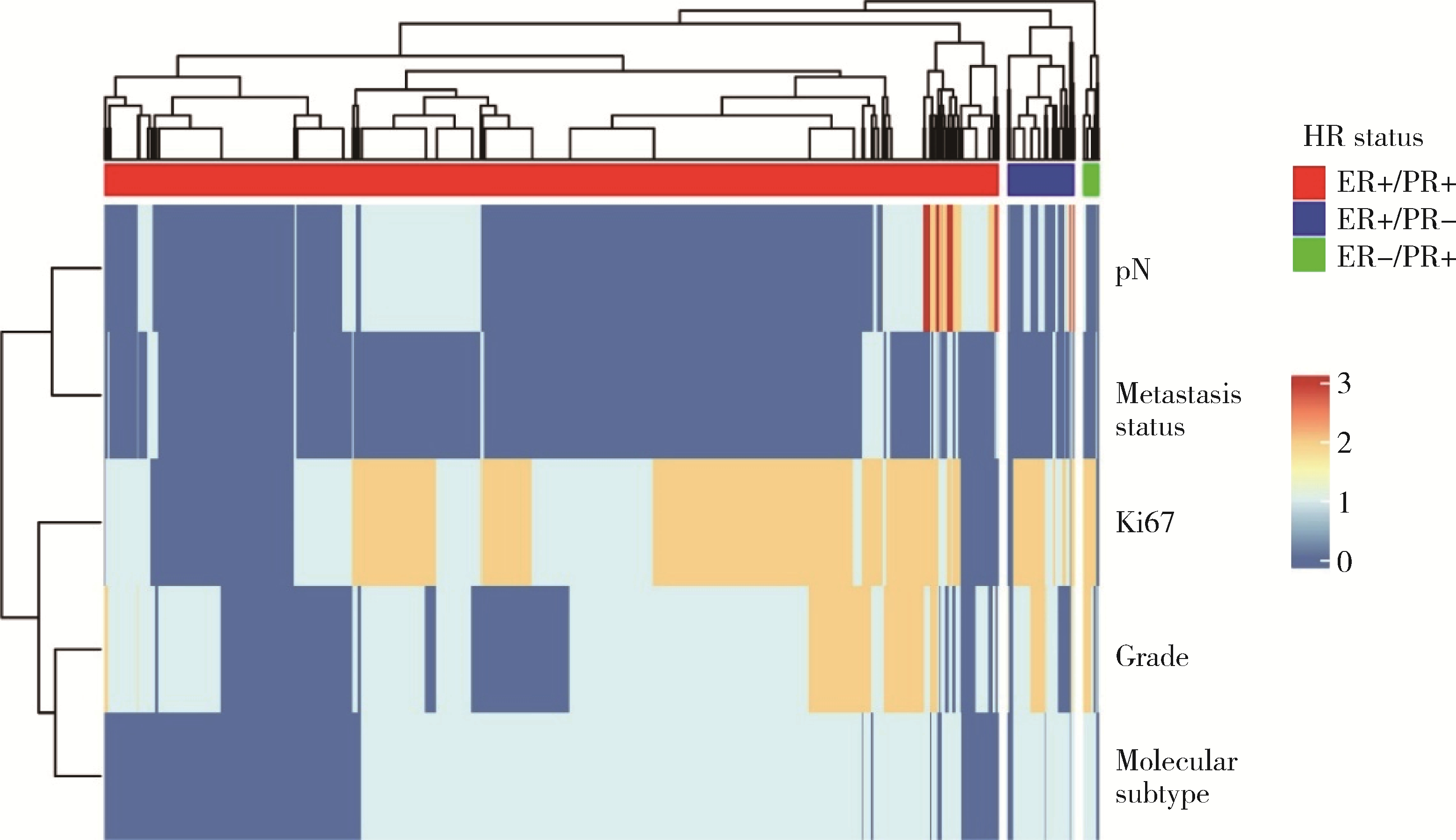
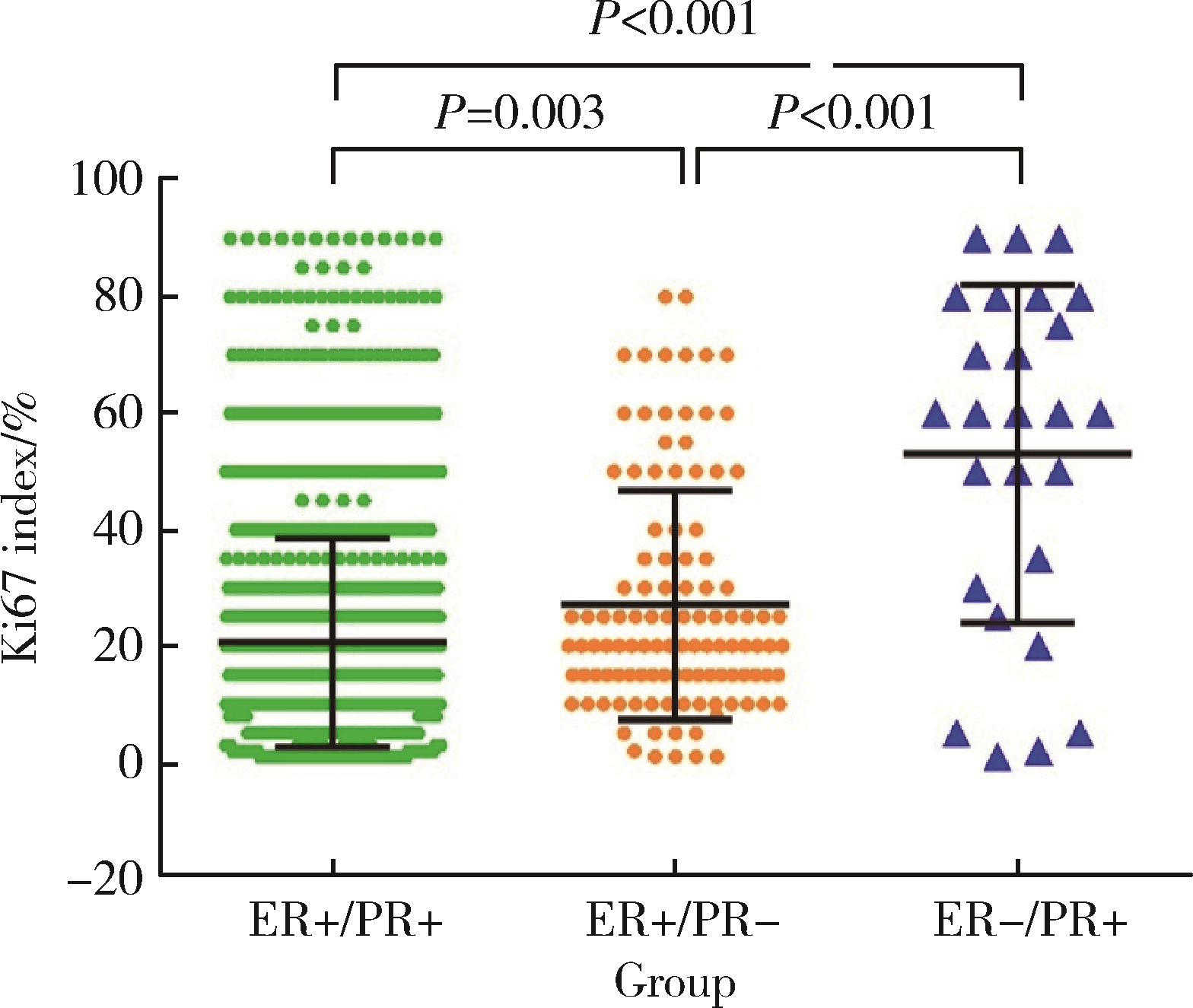
目的: 探讨激素受体阳性/人表皮生长因子受体2阴性(hormone receptor-positive/human epidermal growth factor receptor 2-negative, HR +/HER2 -)乳腺癌患者临床病理特征及预后。方法: 收集2008年1月至2017年12月北京大学第一医院乳腺疾病中心连续诊治的3 035例浸润性乳腺癌患者,对临床病理信息完善的HR +/HER2 -患者的重要临床病理参数及其预后意义进行分析。结果: 1 920例(63.26%)HR +/HER2 -乳腺癌患者中资料完善者1 624例,其中124例(7.64%)出现复发转移,63例死于该病,5年总生存率和无病生存率分别为93.0%及92.6%。pT1及2期占92.80%,pN0期占69.03%;组织学非特殊型占89.66%,分级1、2、3级分别为30.11%、55.60%和14.29%;ER阴性、低表达、高表达患者分别占1.60%、2.09%、96.31%,PR阴性、低表达、高表达分别占6.83%、10.47%、82.70%;Ki67指数<10%、≥10%且 < 20%、≥20%者分别占19.52%、32.02%和48.46%。预后及生存分析显示, pT1期复发转移风险较pT3组低,pT2和pT3组较pT1组无病生存期(disease-free survival,DFS)短,易复发转移;pN0、pN1及pN2期复发转移风险均较pN3期低,与DFS呈负相关;组织学1及2级复发转移风险较3级低,与DFS呈负相关;Ki67指数≥20%更易复发转移。ER在HR +/HER2 -乳腺癌中预后意义不明显,但PR阴性和低表达更易复发转移,生存分析显示,PR表达水平<10%患者的DFS及总生存期(overall survival,OS)最短,10%~60%次之,>60%最长。124例复发转移者以骨转移多见(55例,44.35%),而肝转移者(30例,24.20%)预后最差。结论: 本研究表明,pT分期、pN分期、组织学分级、HR表达水平、Ki67指数等临床病理参数是HR +/HER2 -乳腺癌的重要预后因素,但意义有所不同,其中pN分期和组织学分级有独立预后价值,PR阳性表达水平具有重要预后和风险预测价值,随PR表达水平升高(<10%、10%~60%、>60%),DFS及OS递增,复发转移风险递减,PR表达>60%者DFS及OS最长,复发转移风险最低,PR危险性分层具有独立预后意义。
中图分类号:
- R737.9
| 1 |
Cao W , Chen HD , Yu YW , et al. Changing profiles of cancer burden worldwide and in China: A secondary analysis of the global cancer statistics 2020[J]. Chin Med J (Engl), 2021, 134 (7): 783- 791.
doi: 10.1097/CM9.0000000000001474 |
| 2 |
Wolff AC , Hammond ME , Schwartz JN , et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer[J]. J Clin Oncol, 2007, 25 (1): 118- 145.
doi: 10.1200/JCO.2006.09.2775 |
| 3 | WHO Classification of Tumours Editorial Board . WHO classification of tumours[M]. 5th ed Lyon: IARC Press, 2019. |
| 4 | Amin MB , Edge SB , Greene FL , et al. AJCC cancer staging ma-nual[M]. 8th ed New York: Springer, 2017. |
| 5 |
Goldhirsch A , Wood WC , Coates AS , et al. Strategies for subtypes-dealing with the diversity of breast cancer: Highlights of the St. Gallen international expert consensus on the primary therapy of early breast cancer 2011[J]. Ann Oncol, 22 (8): 1736- 1747.
doi: 10.1093/annonc/mdr304 |
| 6 |
Hammond ME , Hayes DF , Dowsett M , et al. American Society of Clinical Oncology/College of American Pathologists guideline re-commendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer[J]. J Clin Oncol, 2010, 28 (16): 2784- 2795.
doi: 10.1200/JCO.2009.25.6529 |
| 7 |
Wolff AC , Hammond ME , Hicks DG , et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Patho-logists clinical practice guideline update[J]. Arch Pathol Lab Med, 2014, 138 (2): 241- 256.
doi: 10.5858/arpa.2013-0953-SA |
| 8 | Cheang MC , Chia SK , Voduc D , et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer[J]. J Nat Cancer Inst, 2009, 101 (10): 731- 750. |
| 9 |
Wolff AC , Hammond MEH , Allison KH , et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update[J]. J Clin Oncol, 2018, 36 (20): 2105- 2122.
doi: 10.1200/JCO.2018.77.8738 |
| 10 |
李挺. 乳腺癌异质性的分子遗传学基础及临床应用[J]. 中华外科杂志, 2017, 55 (2): 104- 108.
doi: 10.3760/cma.j.issn.0529-5815.2017.02.006 |
| 11 | 李挺. 乳腺癌病理诊断评估与治疗决策[J]. 中国实用外科杂志, 2008, 28 (7): 74- 76. |
| 12 |
Perou CM , Sorlie T , Eisen MB , et al. Molecular portraits of human breast tumours[J]. Nature, 2000, 406 (6797): 747- 752.
doi: 10.1038/35021093 |
| 13 | Zhang S , Huang S , Zhang H , et al. Histo-and clinico-pathological analysis of a large series of triple-negative breast cancer in a single center in China: Evidences on necessity of histological subtyping and grading[J]. Chin J Cancer Res, 2020, 32 (5): 580- 595. |
| 14 |
André F , Ciruelos E , Rubovszky G , et al. Alpelisib for PIK3CA-mutated, hormone receptor-positive advanced breast cancer[J]. N Engl J Med, 2019, 380 (20): 1929- 1940.
doi: 10.1056/NEJMoa1813904 |
| 15 |
van't Veer LJ , Dai H , van de Vijver MJ , et al. Gene expression profiling predicts clinical outcome of breast cancer[J]. Nature, 2002, 415 (6871): 530- 536.
doi: 10.1038/415530a |
| 16 |
Sparano JA , Crager MR , Tang G , et al. Development and validation of a tool integrating the 21-gene recurrence score and clinical-pathological features to individualize prognosis and prediction of chemotherapy benefit in early breast cancer[J]. J Clin Oncol, 2021, 39 (6): 557- 564.
doi: 10.1200/JCO.20.03007 |
| 17 |
Pan H , Gray R , Braybrooke J , et al. 20-year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years[J]. N Engl J Med, 2017, 377 (19): 1836- 1846.
doi: 10.1056/NEJMoa1701830 |
| 18 |
Duffy MJ , Harbeck N , Nap M , et al. Clinical use of biomarkers in breast cancer: Updated guidelines from the European Group on Tumor Markers (EGTM)[J]. Eur J Cancer, 2017, 75, 284- 298.
doi: 10.1016/j.ejca.2017.01.017 |
| 19 |
Zhao H , Gong Y . The prognosis of single hormone receptor-positive breast cancer stratified by HER2 status[J]. Front Oncol, 2021, 11, 643956.
doi: 10.3389/fonc.2021.643956 |
| 20 |
Dauphine C , Moazzez A , Neal J , et al. Single hormone receptor-positive breast cancers have distinct characteristics and survival[J]. Ann Surg Oncol, 2020, 27 (12): 4687- 4694.
doi: 10.1245/s10434-020-08898-5 |
| 21 |
Li Z , Tu Y , Wu Q , et al. Clinical characteristics and outcomes of single versus double hormone receptor-positive breast cancer in 2 large databases[J]. Clin Breast Cancer, 2020, 20 (2): e151- e163.
doi: 10.1016/j.clbc.2019.07.002 |
| 22 | Ye J , Wang W , Xin L , et al. The clinicopathological factors associated with disease progression in luminal A breast cancer and characteristics of metastasis: A retrospective study from a single center in China[J]. Anticancer Res, 2017, 37 (8): 4549- 4556. |
| 23 |
Yamamura J , Kamigaki S , Fujita J , et al. New insights into patterns of first metastatic sites influencing survival of patients with hormone receptor-positive, HER2-negative breast cancer: A multicenter study of 271 patients[J]. BMC Cancer, 2021, 21 (1): 476.
doi: 10.1186/s12885-021-08219-3 |
| [1] | 马建勋,夏有辰,李比,赵红梅,雷玉涛,布希. 乳腺癌改良根治术后即刻乳房重建的方式选择[J]. 北京大学学报(医学版), 2023, 55(4): 612-618. |
| [2] | 张云静,乔丽颖,祁萌,严颖,亢伟伟,刘国臻,王明远,席云峰,王胜锋. 乳腺癌患者新发心血管疾病预测模型的建立与验证:基于内蒙古区域医疗数据[J]. 北京大学学报(医学版), 2023, 55(3): 471-479. |
| [3] | 朱晓娟,张虹,张爽,李东,李鑫,徐玲,李挺. 人表皮生长因子受体2低表达乳腺癌的临床病理学特征及预后[J]. 北京大学学报(医学版), 2023, 55(2): 243-253. |
| [4] | 宋国红,李惠平,邸立军,严颖,姜晗昉,徐玲,万冬桂,李瑛,王墨培,肖宇,张如艳,冉然,王环. 真实世界吡咯替尼治疗HER2阳性转移性乳腺癌的疗效及安全性[J]. 北京大学学报(医学版), 2020, 52(2): 254-260. |
| [5] | 张晔,张妮,刘晓筱,周传香. 唾液腺腺样囊性癌淋巴结转移相关的临床病理分析[J]. 北京大学学报(医学版), 2020, 52(1): 30-34. |
| [6] | 张旭初,张建华,王荣福,范岩,付占立,闫平,赵光宇,白艳霞. 18F-FDG PET/CT联合多种肿瘤标志物在结直肠中分化腺癌术后复发及转移中的应用价值[J]. 北京大学学报(医学版), 2019, 51(6): 1071-1077. |
| [7] | 黄子雄,杜依青,张晓鹏,刘士军,徐涛. 肾细胞癌骨转移的临床与病理分析[J]. 北京大学学报(医学版), 2018, 50(5): 811-815. |
| [8] | 黄子雄,张晓鹏,董森,刘士军,杨荣利,周宇石,马伟国. 肾黏液性小管和梭形细胞癌合并骨转移1例及文献回顾[J]. 北京大学学报(医学版), 2018, 50(4): 732-735. |
| [9] | 朱燕,石永进,赵玉亮,朱平. 拓扑异构酶抑制剂通过ATM/ATR和NF-κB途径上调乳腺癌细胞MICA/B 的表达[J]. 北京大学学报(医学版), 2018, 50(2): 318-325. |
| [10] | 康磊,霍焱,王荣福,张春丽,闫平,徐小洁. MicroRNA-155靶向的放射性标记探针对乳腺癌小鼠模型的活体显像[J]. 北京大学学报(医学版), 2018, 50(2): 326-330. |
| [11] | 赵轶国,杨晓东,张雁凯,宁宁,邢兆东,叶颖江. 美克尔憩室癌变及肝多发转移并消化道出血1例[J]. 北京大学学报(医学版), 2017, 49(6): 1095-1097. |
| [12] | 郭福新,姜玉良,吉喆,彭冉,孙海涛,王俊杰. 3D打印非共面模板辅助CT引导125Ⅰ粒子植入治疗锁骨上复发转移癌的剂量学研究[J]. 北京大学学报(医学版), 2017, 49(3): 506-511. |
| [13] | 王威,郑磊,刘树铭,黄明伟,石妍,吕晓鸣,张杰,张建国. 单纯放射性粒子治疗后的头颈部腺源性癌远处转移[J]. 北京大学学报(医学版), 2017, 49(3): 547-550. |
| [14] | 方伟岗,田新霞. 肿瘤微环境中一种新型促侵袭因子的发现——细胞外ATP功能及机制的研究进展[J]. 北京大学学报(医学版), 2017, 49(2): 188-195. |
| [15] | 李秀楠,刘爱蕙,唐欣,任宇. 尿路上皮癌相关1基因通过竞争性抑制miR-18a增强乳腺癌细胞的他莫昔芬治疗耐药[J]. 北京大学学报(医学版), 2017, 49(2): 295-302. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 189
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 567
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||