北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (1): 30-34. doi: 10.19723/j.issn.1671-167X.2020.01.005
唾液腺腺样囊性癌淋巴结转移相关的临床病理分析
- 北京大学口腔医学院·口腔医院,口腔病理科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室,北京 100081
Cervical lymph node metastasis in adenoid cystic carcinoma of the salivary glands: A clinicopathologic study
Ye ZHANG,Ni ZHANG,Xiao-xiao LIU,Chuan-xiang ZHOU( )
)
- Department of Oral Pathology, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
摘要:
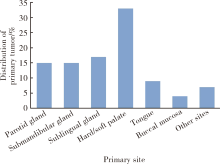
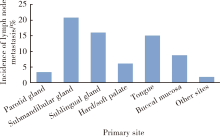
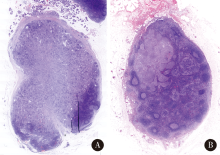
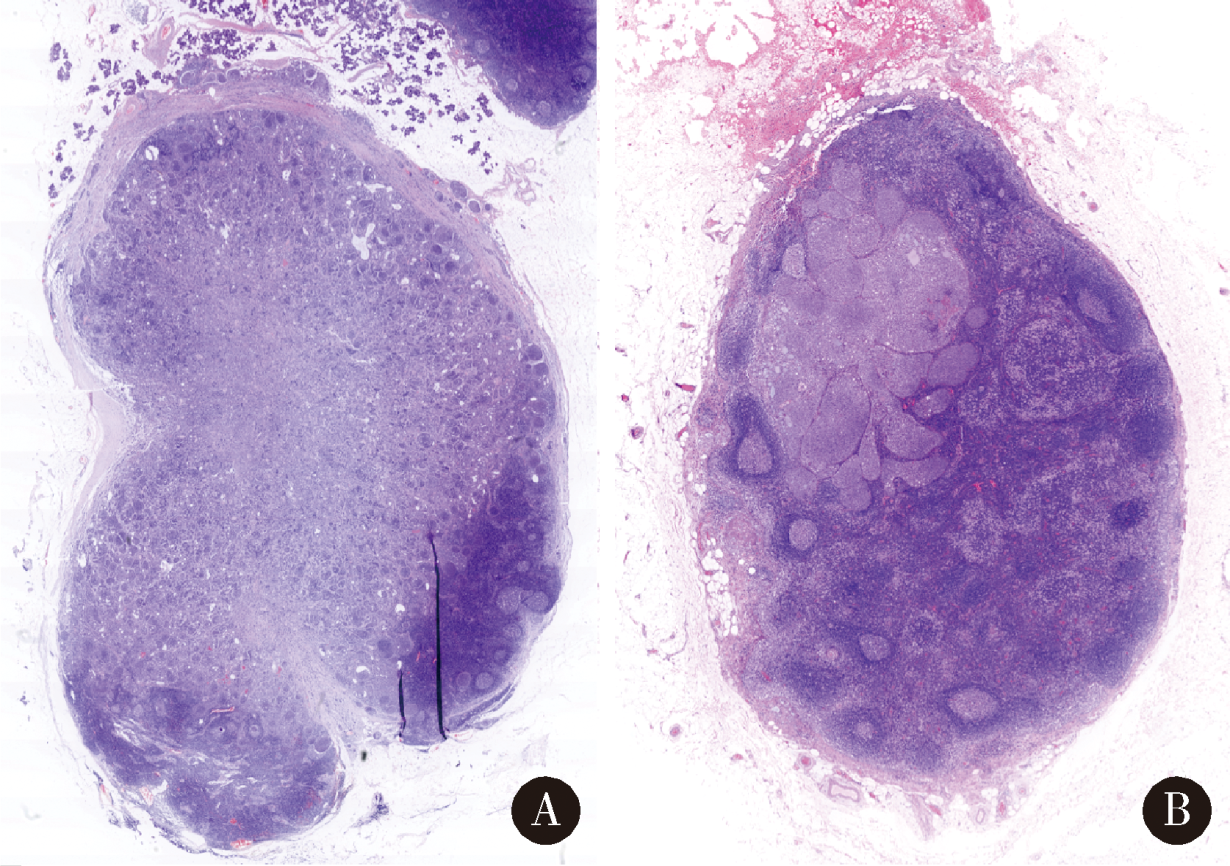
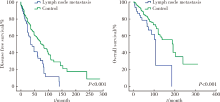
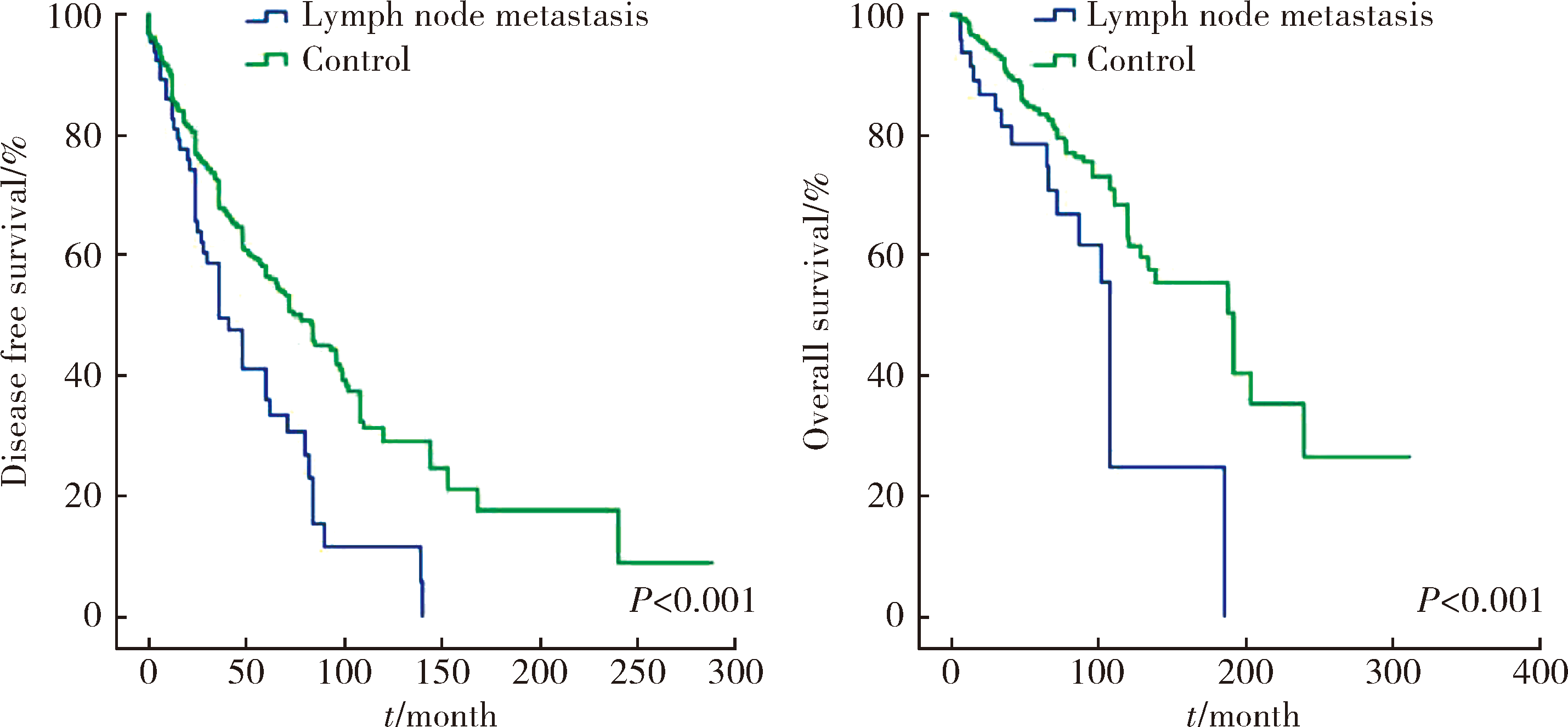
目的:回顾性分析唾液腺腺样囊性癌颈部淋巴结转移的发病率及其临床病理特征。方法:回顾性分析2001年1月至2019年1月在北京大学口腔医院诊治并经病理确诊为腺样囊性癌的798例患者的临床病理资料,对82例发生颈部淋巴结转移的患者进行详细的临床病理及统计学分析。结果:纳入研究的腺样囊性癌患者798例,腭部、舌下口底区域和腮腺区是腺样囊性癌常见的发病部位。经病理学检查证实发生颈部淋巴结转移者82例,总体转移率约10.3%(82/798),其中原发于颌下腺、舌下口底区及舌部的颈部淋巴结转移率较高,分别为20.8%、16.1%、15.1%,而腭部、腮腺原发病例颈部淋巴结转移率较低,分别为6.1%、3.4%。颈Ⅰ、Ⅱ区为常见转移区域,极少累及Ⅳ、Ⅴ区淋巴结。主要转移模式是由癌细胞沿经典的淋巴管/血管通路转移(70.7%),部分颌下及舌下病例不除外直接侵犯淋巴结。82例伴淋巴结转移的患者5年和10年总生存率分别为77.4% 和 20.6%。淋巴结转移阳性组患者总生存率和无瘤生存率均显著低于转移阴性组,且组织学呈现实性型的腺样囊性癌颈部淋巴结转移率显著高于筛孔型和管状型肿瘤。结论:舌下、口底及颌下腺为唾液腺腺样囊性癌颈部淋巴转移常见原发部位,实性型组织学结构与转移率显著正相关,在临床诊治及随访中需要更多关注。
中图分类号:
- R739.87
| [1] | Tian Z, Li L, Wang L , et al. Salivary gland neoplasms in oral and maxillofacial regions: A 23-year retrospective study of 6 982 cases in an eastern Chinese population[J]. Int J Oral Maxillofac Surg, 2010,39(3):235-242. |
| [2] | Gao M, Hao Y, Huang MX , et al. Clinicopathological study of distant metastases of salivary adenoid cystic carcinoma[J]. Int J Oral Maxillofac Surg, 2013,42(8):923-928. |
| [3] | Shen C, Xu T, Huang C , et al. Treatment outcomes and prognostic features in adenoid cystic carcinoma originated from the head and neck[J]. Oral Oncol, 2012,48(5):445-449. |
| [4] | Lloyd S, Yu JB, Wilson LD , et al. Determinants and patterns of survival in adenoid cystic carcinoma of the head and neck, including an analysis of adjuvant radiation therapy[J]. Am J Clin Oncol, 2011,34(1):76-81. |
| [5] | Bhayani MK, Yener M, El-Naggar A , et al. Prognosis and risk factors for early-stage adenoid cystic carcinoma of the major salivary glands[J]. Cancer, 2012,118(11):2872-2878. |
| [6] | Armstrong JG, Harrison LB, Thaler HT , et al. The indications for elective treatment of the neck in cancer of the major salivary glands[J]. Cancer, 1992,69(3):615-619. |
| [7] | Suárez C, Barnes L, Silver CE , et al. Cervical lymph node metastasis in adenoid cystic carcinoma of oral cavity and oropharynx: A collective international review[J]. Auris Nasus Larynx, 2016,43(5):477-484. |
| [8] | Ardekian L, Kokemueller H, Eckardt A , et al. Adenoid cystic carcinoma of the head and neck: A 20 years experience[J]. Int J Oral Maxillofac Surg, 2004,33(1):25-31. |
| [9] | Bianchi B, Copelli C, Cocchi R , et al. Adenoid cystic carcinoma of intraoral minor salivary glands[J]. Oral Oncol, 2008,44(11):1026-1031. |
| [10] | Coca-Pelaz A, Rodrigo JP, Bradley PJ , et al. Adenoid cystic carcinoma of the head and neck: An update[J]. Oral Oncol, 2015,51(7):652-661. |
| [11] | Zhang M, Xu ZF, Tao Y , et al. Clinical analysis of 25 patients with glossal adenoid cystic carcinoma[J]. Int J Stomt, 2009,36(2):148-151. |
| [12] | Min R, Siyi L, Wenjun Y , et al. Salivary gland adenoid cystic carcinoma with cervical lymph node metastasis: A preliminary study of 62 cases[J]. Int J Oral Maxillofac Surg, 2012,41(8):952-957. |
| [13] | Amit M, Binenbaum Y, Sharma K , et al. Incidence of cervical lymph node metastasis and its association with outcomes in patients with adenoid cystic carcinoma. An international collaborative study[J]. Head Neck, 2015,37(7):1032-1037. |
| [14] | Weinreb I, Lee SY, Kim BH , et al. Nineteen-year oncologic outcomes and the benefit of elective neck dissection in salivary gland adenoid cystic carcinoma[J]. Head Neck, 2014,36(12):1796-1801. |
| [15] | Ali S, Palmer FL, Katabi N , et al. Long-term local control rates of patients with adenoid cystic carcinoma of the head and neck managed by surgery and postoperative radiation[J]. Laryngoscope, 2017,127(10):2265-2269. |
| [16] | Nakada M, Nishizaki K, Akagi H , et al. Oncocytic carcinoma of the submandibular gland: a case report and literature review[J]. J Oral Pathol Med, 1998,27(5):225-228. |
| [17] | Amit M, Na’ara S, Sharma K , et al. Elective neck dissection in patients with head and neck adenoid cystic carcinoma: An international collaborative study[J]. Ann Surg Oncol, 2015,22(4):1353-1359. |
| [1] | 杨玉淑, 齐晅, 丁萌, 王炜, 郭惠芳, 高丽霞. 抗唾液腺蛋白1抗体联合抗腮腺分泌蛋白抗体对干燥综合征的诊断价值[J]. 北京大学学报(医学版), 2024, 56(5): 845-852. |
| [2] | 刘东武, 陈杰, 高明利, 于静. 类风湿关节炎伴发淋巴结Castleman样病理改变1例[J]. 北京大学学报(医学版), 2024, 56(5): 928-931. |
| [3] | 黄教悌,胡菁,韩博. 治疗相关神经内分泌前列腺癌机制研究与靶向治疗新进展[J]. 北京大学学报(医学版), 2024, 56(4): 557-561. |
| [4] | 张树栋,谢睿扬. 机器人手术时代的肾癌合并腔静脉瘤栓治疗策略[J]. 北京大学学报(医学版), 2024, 56(4): 562-564. |
| [5] | 邢念增,王明帅,杨飞亚,尹路,韩苏军. 前列腺免活检创新理念的临床实践及其应用前景[J]. 北京大学学报(医学版), 2024, 56(4): 565-566. |
| [6] | 田宇轩,阮明健,刘毅,李德润,吴静云,沈棋,范宇,金杰. 双参数MRI改良PI-RADS评分4分和5分病灶的最大径对临床有意义前列腺癌的预测效果[J]. 北京大学学报(医学版), 2024, 56(4): 567-574. |
| [7] | 颜野,李小龙,夏海缀,朱学华,张羽婷,张帆,刘可,刘承,马潞林. 前列腺癌根治术后远期膀胱过度活动症的危险因素[J]. 北京大学学报(医学版), 2024, 56(4): 589-593. |
| [8] | 于书慧,韩佳凝,钟丽君,陈聪语,肖云翔,黄燕波,杨洋,车新艳. 术前盆底肌电生理参数对前列腺癌根治性切除术后早期尿失禁的预测价值[J]. 北京大学学报(医学版), 2024, 56(4): 594-599. |
| [9] | 刘帅,刘磊,刘茁,张帆,马潞林,田晓军,侯小飞,王国良,赵磊,张树栋. 伴静脉癌栓的肾上腺皮质癌的临床治疗及预后[J]. 北京大学学报(医学版), 2024, 56(4): 624-630. |
| [10] | 舒帆,郝一昌,张展奕,邓绍晖,张洪宪,刘磊,王国良,田晓军,赵磊,马潞林,张树栋. 肾部分切除术治疗囊性肾癌的功能学和肿瘤学结果:单中心回顾性研究[J]. 北京大学学报(医学版), 2024, 56(4): 667-672. |
| [11] | 周泽臻,邓绍晖,颜野,张帆,郝一昌,葛力源,张洪宪,王国良,张树栋. 非转移性T3a肾细胞癌患者3年肿瘤特异性生存期预测[J]. 北京大学学报(医学版), 2024, 56(4): 673-679. |
| [12] | 费秀文,刘斯,汪波,董爱梅. 成人及儿童组织坏死性淋巴结炎临床特征及治疗[J]. 北京大学学报(医学版), 2024, 56(3): 533-540. |
| [13] | 赖展鸿,李嘉辰,贠泽霖,张永刚,张昊,邢晓燕,邵苗,金月波,王乃迪,李依敏,李玉慧,栗占国. 特发性炎性肌病完全临床应答相关因素的单中心真实世界研究[J]. 北京大学学报(医学版), 2024, 56(2): 284-292. |
| [14] | 彭圣嘉,祁雨,孙丽杰,李丹,王新宇,韩江莉,陈宝霞,张媛. 传入压力反射衰竭合并低钠血症1例[J]. 北京大学学报(医学版), 2024, 56(2): 357-361. |
| [15] | 俞光岩. 儿童唾液腺疾病[J]. 北京大学学报(医学版), 2024, 56(1): 1-3. |
|
||