北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (2): 293-297. doi: 10.19723/j.issn.1671-167X.2021.02.010
Oxford膝关节单间室置换术后内翻多因素分析
- 北京积水潭医院矫形骨科,北京 100035
Multivariate analysis of varus after Oxford unicompartmental knee arthroplasty
JI Song-jie,HUANG Ye,WANG Xing-shan,LIU Jian,DOU Yong,JIANG Xu,ZHOU Yi-xin( )
)
- Department of Adult Joint Reconstruction Surgery, Beijing Jishuitan Hospital, Beijing 100035, China
摘要:
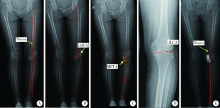
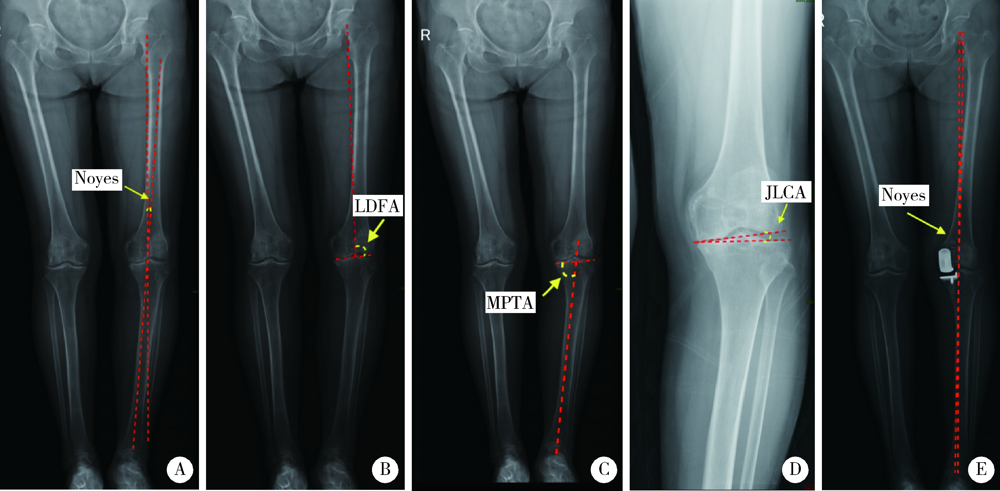
目的: 分析使用Oxford膝关节单间室假体置换术后出现内翻的术前影响因素。方法: 选择北京积水潭医院矫形骨科2018年1月至2019年12月施行的660例(767膝)Oxford单间室置换患者的病例资料进行回顾性分析。根据术后力线X线片分为内翻组(Noyes≥3°)和正常组(Noyes<3°)两组。比较两组患者性别、年龄、体重指数(body mass index,BMI)、膝关节活动度(range of motion,ROM)、术前屈曲畸形(flexion deformity,FD)、膝关节疼痛评分(American Knee Society pain score,AKS)和功能评分(American Knee Society function score,AKS function), 测量术前Noyes角、股骨远端外侧角(lateral distal femoral angle,LDFA)、胫骨近端内侧角(medial proximal tibial angle,MPTA)、关节线相交角(joint line converge angle,JLCA), 并对以上术前因素进行分析。结果: 患者的性别、术侧、年龄、BMI、术前ROM、术前膝关节疼痛评分和功能评分不是术后力线内翻的危险因素(P>0.05)。术后内翻的影响因素依次为MPTA<84°(P=0.018,OR=3.712,95%CI:1.250~11.027), 术前Noyes>5°(P=0.000,OR=3.105,95%CI:1.835~5.254),术前FD>5°(P=0.001,OR=1.976,95%CI:1.326~3.234)。术前LDFA(P=0.146)和术前JLCA(P=0.709)对术后力线都没有表现出统计学意义的影响。结论: 术前内翻较重的患者,尤其内翻畸形主要来自胫骨侧的患者,以及术前有屈曲畸形的患者更容易出现Oxford单间室置换术后力线内翻。
中图分类号:
- R687.4
| [1] |
Berger RA, Meneghini RM, Jacobs JJ, et al. Results of unicom-partmental knee arthroplasty at a minimum of ten years of follow-up[J]. J Bone Joint Surg Am, 2005,87(5):999-1006.
doi: 10.2106/JBJS.C.00568 pmid: 15866962 |
| [2] |
Kim MS, Koh IJ, Choi YJ, et al. Differences in patient-reported outcomes between unicompartmental and total knee arthroplasties: a propensity score-matched analysis[J]. J Arthroplasty, 2017,32(5):1453-1459.
doi: 10.1016/j.arth.2016.11.034 pmid: 27979407 |
| [3] |
van der List JP, Chawla H, Zuiderbaan HA, et al. Patients with isolated lateral osteoarthritis: Unicompartmental or total knee arthroplasty[J]. Knee, 2016,23(6):968-974.
doi: 10.1016/j.knee.2016.06.007 |
| [4] |
Ko YB, Gujarathi MR, Oh KJ. Outcome of unicompartmental knee arthroplasty: a systematic review of comparative studies between fixed and mobile bearings focusing on complications[J]. Knee Surg Relat Res, 2015,27(3):141-148.
doi: 10.5792/ksrr.2015.27.3.141 pmid: 26389066 |
| [5] |
Kim KT, Lee S, Kim TW, et al. The influence of postoperative tibiofemoral alignment on the clinical results of unicompartmental knee arthroplasty[J]. Knee Surg Relat Res, 2012,24(2):85-90.
doi: 10.5792/ksrr.2012.24.2.85 pmid: 22708108 |
| [6] |
Bruni D, Iacono F, Russo A, et al. Minimally invasive unicom-partmental knee replacement: retrospective clinical and radiographic evaluation of 83 patients[J]. Knee Surg Sports Traumatol Arthrosc, 2010,18(6):710-717.
doi: 10.1007/s00167-009-0895-9 pmid: 19763541 |
| [7] | Ewald FC. The knee society total knee arthroplasty roentgenographic evaluation and scoring system[J]. Clin Orthop Relat Res, 1989,248(11):9-12. |
| [8] | Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length[J]. Clin Orthop Relat Res, 1992,274(1):248-264. |
| [9] |
Price AJ, O’Connor JJ, Murray DW, et al. A history of Oxford unicompartmental knee arthroplasty[J]. Orthopedics, 2007,30(Suppl 5):7-10.
doi: 10.3928/01477447-20070101-01 |
| [10] |
Choy WS, Kim KJ, Lee SK, et al. Mid-term results of oxford medial unicompartmental knee arthroplasty[J]. Clin Orthop Surg, 2011,3(3):178-183.
doi: 10.4055/cios.2011.3.3.178 pmid: 21909464 |
| [11] |
Mercier N, Wimsey S, Saragaglia D. Long-term clinical results of the Oxford medial unicompartmental knee arthroplasty[J]. Int Orthop, 2010,34(8):1137-1143.
doi: 10.1007/s00264-009-0869-z pmid: 19838707 |
| [12] |
Kuipers BM, Kollen BJ, Bots PC, et al. Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement[J]. Knee, 2010,17(1), 48-52.
doi: 10.1016/j.knee.2009.07.005 |
| [13] | 及松洁, 黄野, 王达成, 等. 胫骨高位闭合截骨与开放截骨对胫骨后倾及髌骨高度的影响[J]. 基础医学与临床, 2020,40(10):1394-1398. |
| [14] |
Aleto TJ, Berend ME, Ritter MA, et al. Early failure of unicom-partmental knee arthroplasty leading to revision[J]. J Arthroplasty, 2008,23(2):159-163.
doi: 10.1016/j.arth.2007.03.020 |
| [15] |
Hernigou P, Deschamps G. Alignment influences wear in the knee after medial unicompartmental arthroplasty[J]. Clin Orthop Relat Res, 2004,423(6):161-165.
doi: 10.1097/01.blo.0000128285.90459.12 |
| [16] | Squire MW, Callaghan JJ, Goetz DD, et al. Unicompartmental knee replacement. A minimum 15 year followup study[J]. Clin Orthop Relat Res, 1999,367(10):61-72. |
| [17] |
Cartier P, Sanouiller JL, Grelsamer RP. Unicompartmental knee arthroplasty surgery. 10-year minimum follow-up period[J]. J Arthroplasty, 1996,11(7):782-788.
doi: 10.1016/s0883-5403(96)80177-x pmid: 8934317 |
| [18] |
Tashiro Y, Matsuda S, Okazaki K, et al. The coronal alignment after medial unicompartmental knee arthroplasty can be predicted: usefulness of full-length valgus stress radiography for evaluating correctability[J]. Knee Surg Sports Traumatol Arthrosc, 2014,22(12):3142-3249.
doi: 10.1007/s00167-014-3248-2 pmid: 25155051 |
| [19] |
Robinson BJ, Rees JL, Price AJ, et al. Dislocation of the bearing of the Oxford lateral unicompartmental arthroplasty. A radiological assessment[J]. J Bone Joint Surg Br, 2002,84(5):653-657.
doi: 10.1302/0301-620x.84b5.12950 pmid: 12188479 |
| [20] |
Scott CE, Eaton MJ, Nutton RW, et al. Proximal tibial strain in medial unicompartmental knee replacements: a biomechanical study of implant design[J]. Bone Joint J, 2013,95B(10):1339-1347.
doi: 10.1302/0301-620X.95B10.31644 |
| [21] |
Sawatari T, Tsumura H, Iesaka K, et al. Three-dimensional finite element analysis of unicompartmental knee arthroplasty: the influence of tibial component inclination[J]. J Orthop Res, 2005,23(3):549-554.
doi: 10.1016/j.orthres.2004.06.007 pmid: 15885474 |
| [22] |
Simpson DJ, Price AJ, Gulati A, et al. Elevated proximal tibial strains following unicompartmental knee replacement: a possible cause of pain[J]. Med Eng Phys, 2009,31(7):752-757.
doi: 10.1016/j.medengphy.2009.02.004 pmid: 19278893 |
| [23] |
Pandit HG, Campi S, Hamilton TW, et al. Five-year experience of cementless Oxford unicompartmental knee replacement[J]. Knee Surg Sports Traumatol Arthrosc, 2017,25(3):694-702.
doi: 10.1007/s00167-015-3879-y pmid: 26611902 |
| [1] | 赵然,刘延青,田华. 应用累积和控制图分析全膝关节置换术中电子压力垫片指导软组织平衡的学习曲线[J]. 北京大学学报(医学版), 2023, 55(4): 658-664. |
| [2] | 叶一林,刘恒,潘利平,柴卫兵. 全膝关节置换术后假体周围痛风发作误诊1例[J]. 北京大学学报(医学版), 2023, 55(2): 362-365. |
| [3] | 李志昌,侯云飞,周之伟,姜龙,张舒,林剑浩. 影响全膝关节置换术患者术前预期的患者因素[J]. 北京大学学报(医学版), 2022, 54(1): 170-176. |
| [4] | 吴浩,潘利平,刘恒,塔拉提百克·买买提居马,王洪彬,宁太国,曹永平. 胫骨假体的不同后倾角度对内侧间室单髁置换术后膝关节功能的影响[J]. 北京大学学报(医学版), 2021, 53(5): 877-882. |
| [5] | 刘恒,李卓扬,曹永平,崔云鹏,吴浩. 胫骨侧徒手截骨的膝关节置换术后力线测量及其影响因素分析[J]. 北京大学学报(医学版), 2018, 50(5): 850-854. |
| [6] | 李杨,李邦国,赵然,田华,张克. 综合止血措施下自体血回输装置对全膝关节置换术失血控制的有效性分析[J]. 北京大学学报(医学版), 2018, 50(4): 651-656. |
| [7] | 张洪,马云青. 直接前入路人工全髋关节置换术[J]. 北京大学学报(医学版), 2017, 49(2): 185-187. |
| [8] | 王浩洋,康鹏德,聂涌,赵海燕,杨周源,裴福兴. 直接前入路全髋关节置换后早期三维步态分析[J]. 北京大学学报(医学版), 2017, 49(2): 196-200. |
| [9] | 张永进,李甲,綦珂,薛晨晨,徐卫东. 全髋关节置换术中直接前方入路与后外侧入路的疗效及安全性分析[J]. 北京大学学报(医学版), 2017, 49(2): 201-205. |
| [10] | 吕明, 张金庆, 王兴山, 黄野, 李为, 张春雨. 直接前入路髋关节置换术及其早期临床疗效[J]. 北京大学学报(医学版), 2017, 49(2): 206-213. |
| [11] | 徐杰,庄伟达,李新炜,俞国雨,林院,罗奋棋,肖毓华. 直接前入路和后外侧保留梨状肌入路全髋关节置换术的疗效对比[J]. 北京大学学报(医学版), 2017, 49(2): 214-220. |
| [12] | 唐竞,吕明,周一新,张纪. 直接前入路双髋关节同时置换22例临床分析[J]. 北京大学学报(医学版), 2017, 49(2): 221-225. |
| [13] | 李杨,李子剑,张克,田华,刘延青,蔡宏,李锋,赵旻暐. 膝髋关节置换术非计划性暂停手术的原因分析[J]. 北京大学学报(医学版), 2017, 49(2): 231-235. |
| [14] | 龚晓峰,吕艳伟,王金辉,王岩,武勇,王满宜. 踝关节CT与踝关节骨折分型的相关性研究[J]. 北京大学学报(医学版), 2017, 49(2): 281-285. |
| [15] | 邓莹,姜天乐,杨晓霞,李民,王军,郭向阳. 连续股神经阻滞联合关节周围浸润镇痛对全膝关节置换术后关节早期功能恢复的影响[J]. 北京大学学报(医学版), 2017, 49(1): 137-141. |
|
||