北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (4): 734-739. doi: 10.19723/j.issn.1671-167X.2021.04.019
内镜治疗中青年双节段腰椎间盘突出症患者的手术策略
越雷,王月田,白纯碧,陈浩,付豪永,于峥嵘,李淳德,孙浩林( )
)
- 北京大学第一医院骨科,北京 100034
Analysis of surgical strategy of percutaneous endoscopic lumbar discectomy in young and middle-aged double-segment patients with lumbar disc herniation
YUE Lei,WANG Yue-tian,BAI Chun-bi,CHEN Hao,FU Hao-yong,YU Zheng-rong,LI Chun-de,SUN Hao-lin( )
)
- Department of 0rthopaedics,Peking University First Hospital,Beijing 100034, China
摘要:
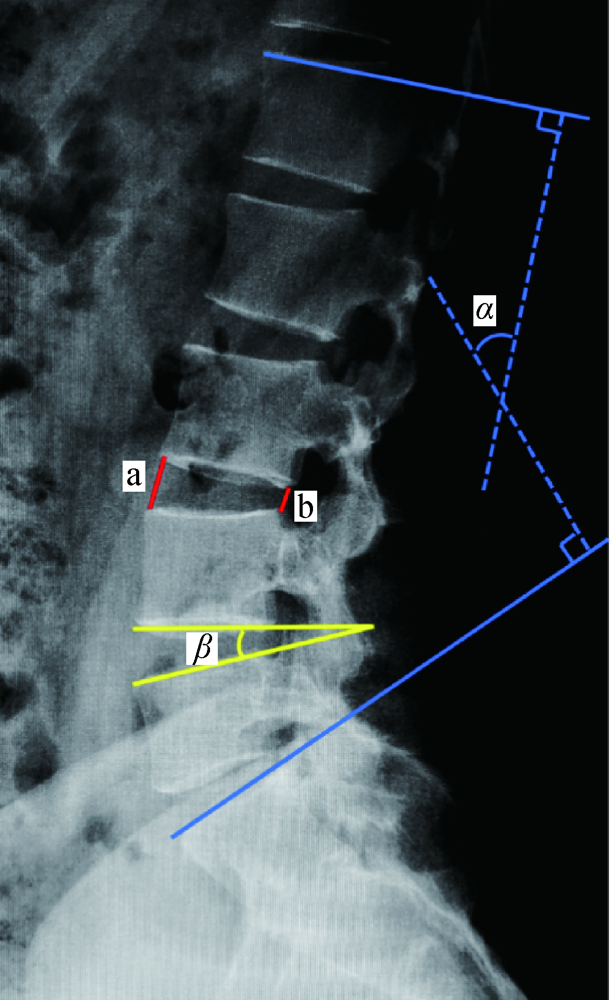
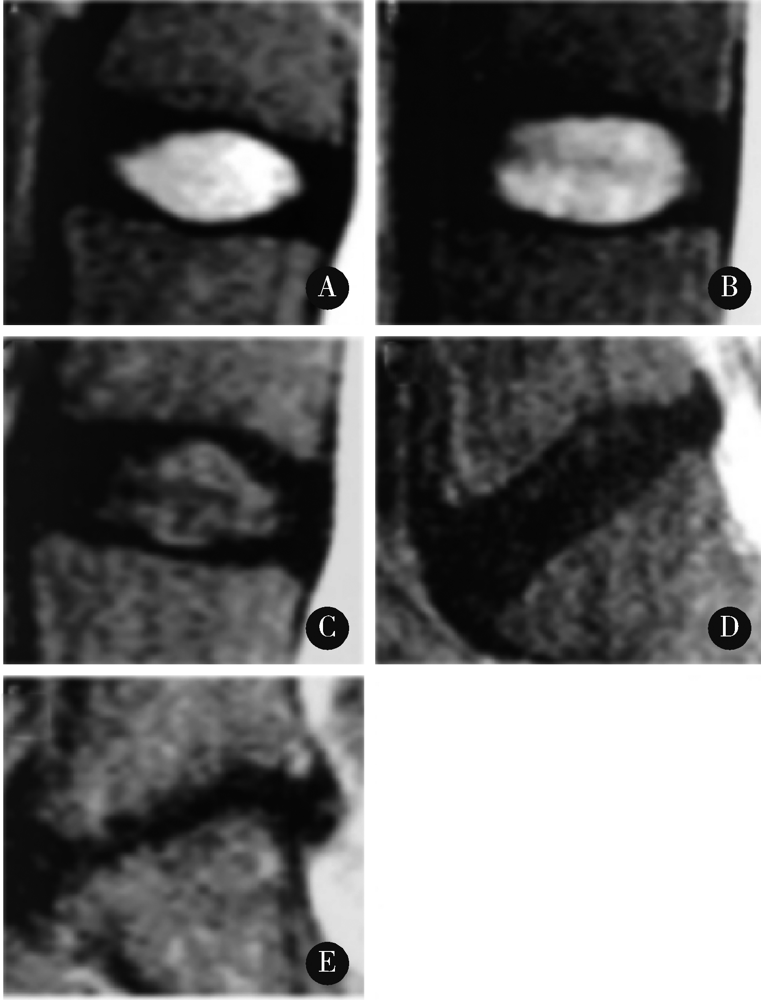
目的: 比较针对中青年双节段腰椎间盘突出症患者分别采用经皮内镜下腰椎间盘单节段责任病灶切除与双节段病灶全部切除的临床疗效与安全性。方法: 选择北京大学第一医院2015年1月至2018年10月应用经皮内镜下腰椎间盘切除术治疗中青年双节段腰椎间盘突出症患者32例进行回顾性分析,其中单节段责任病灶治疗组(单节段组)18例,双节段病灶治疗组(双节段组)14例。临床评价采用腰腿痛视觉模拟量表评分(visual analogue score,VAS)和 oswestry功能障碍指数(oswestry disability index,ODI),分别于术前、术后3个月、末次随访时比较两组患者的临床症状转归,同时采用Macnab标准评价患者术后总体满意度;影像学参数包括X线片的腰椎前凸角、病灶节段椎间高度、病灶节段终板角,以及磁共振成像(magnetic resonance imaging, MRI)的腰椎间盘突出程度密歇根州立大学(Michigan State University,MSU)分级和T2序列上椎间盘退变程度的Pfirrmann分级;围手术期参数包括手术医师、麻醉方式、手术时间、术后住院天数、术后支具佩戴时间及围手术期并发症。结果: 最终纳入患者平均随访(26.78±10.64)个月,两组之间随访时间和基线信息差异无统计学意义(P>0.05)。临床症状评估方面,双节段组在术后3个月和末次随访的ODI相比于单节段组明显更低(P<0.05),同时双节段组末次随访ODI相较于术前缓解强于单节段组(P<0.05);影像学方面,术前两组X线和MRI影像学参数在主要病灶和次要病灶上均无明显差异。两组主要病灶的MSU突出分级在术后分别较术前均明显降低(P<0.05)。次要病灶的MSU突出分级双节段组术后较术前明显降低(P<0.05), 而单节段组次要病灶MSU突出分级术后较术前差异并无统计学意义(P>0.05);围术期参数方面,单节段组手术时间明显短于双节段组(P<0.001),两组均未发现围手术期并发症,但单节段组术后随访期间内3例患者接受了二次腰椎手术治疗。结论: 对于中青年双节段腰椎间盘突出症患者,双节段病灶同期切除在中长期可能有更好的功能改善而不增加相关手术并发症的风险。
中图分类号:
- R681.5
| [1] |
Frymoyer JW, Pope MH, Clements JH, et al. Risk factors in low-back pain. An epidemiological survey [J]. J Bone Joint Surg Am, 1983, 65(2):213-218.
pmid: 6218171 |
| [2] |
Andersson GB. Epidemiological features of chronic low-back pain [J]. Lancet, 1999, 354(9178):581-585.
pmid: 10470716 |
| [3] |
Amin RM, Andrade NS, Neuman BJ. Lumbar disc herniation [J]. Curr Rev Musculoskelet Med, 2017, 10(4):507-516.
doi: 10.1007/s12178-017-9441-4 pmid: 28980275 |
| [4] | Lee DY, Ahn Y, Lee SH. Percutaneous endoscopic lumbar discectomy for adolescent lumbar disc herniation: surgical outcomes in 46 consecutive patients [J]. Mt Sinai J Med, 2006, 73(6):864-870. |
| [5] |
Forst R, Hausmann B. Nucleoscopy: a new examination technique [J]. Arch Orthop Trauma Surg, 1983, 101(3):219-221.
doi: 10.1007/BF00436774 |
| [6] |
Jasper GP, Francisco GM, Telfeian AE. Clinical success of transforaminal endoscopic discectomy with foraminotomy: a retrospective evaluation [J]. Clin Neurol Neurosurg, 2013, 115(10):1961-1965.
doi: 10.1016/j.clineuro.2013.05.033 |
| [7] |
Mysliwiec LW, Cholewicki J, Winkelpleck MD, et al. MSU classification for herniated lumbar discs on MRI: toward developing objective criteria for surgical selection [J]. Eur Spine J, 2010, 19(7):1087-1093.
doi: 10.1007/s00586-009-1274-4 pmid: 20084410 |
| [8] |
Pfirrmann CW, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration [J]. Spine (Phila Pa 1976), 2001, 26(17):1873-1878.
doi: 10.1097/00007632-200109010-00011 |
| [9] | Brayda-Bruno M, Tibiletti M, Ito K, et al. Advances in the diagnosis of degenerated lumbar discs and their possible clinical application [J]. Eur Spine J, 2014, 23(Suppl 3):S315-323. |
| [10] |
Colombier P, Clouet J, Hamel O, et al. The lumbar intervertebral disc: from embryonic development to degeneration [J]. Joint Bone Spine, 2014, 81(2):125-129.
doi: 10.1016/j.jbspin.2013.07.012 pmid: 23932724 |
| [11] |
Shin KH, Chang HG, Rhee NK, et al. Revisional percutaneous full endoscopic disc surgery for recurrent herniation of previous open lumbar discectomy [J]. Asian Spine J, 2011, 5(1):1-9.
doi: 10.4184/asj.2011.5.1.1 |
| [12] |
Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nono-perative treatment for lumbar disk herniation: the spine patient outcomes research trial (SPORT): a randomized trial [J]. JAMA, 2006, 296(20):2441-2450.
pmid: 17119140 |
| [13] |
Osterman H, Seitsalo S, Karppinen J, et al. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up [J]. Spine (Phila Pa 1976), 2006, 31(21):2409-2414.
doi: 10.1097/01.brs.0000239178.08796.52 |
| [14] |
Parker SL, Xu R, McGirt MJ, et al. Long-term back pain after a single-level discectomy for radiculopathy: incidence and health care cost analysis [J]. J Neurosurg Spine, 2010, 12(2):178-182.
doi: 10.3171/2009.9.SPINE09410 |
| [15] | 彭耀庆, 杨檑, 江皓. 显微内窥镜下治疗多节段腰椎间盘突出症的手术策略 [J]. 中国脊柱脊髓杂志, 2003, 13(2):79-81. |
| [16] |
Kleinig TJ, Brophy BP, Maher CG. Practical neurology-3: back pain and leg weakness [J]. Med J Aust, 2011, 195(8):454-457.
doi: 10.5694/mja2.2011.195.issue-8 |
| [17] |
Beynon R, Hawkins J, Laing R, et al. The diagnostic utility and cost-effectiveness of selective nerve root blocks in patients consi-dered for lumbar decompression surgery: a systematic review and economic model [J]. Health Technol Assess, 2013, 17(19):1-88.
doi: 10.3310/hta17190 pmid: 23673151 |
| [18] | 阮狄克, 周鸿奇. 椎间盘摘除术对腰椎稳定性的影响 [J]. 中国脊柱脊髓杂志, 1993, 3(4):159-162. |
| [19] | 关家文, 刘继财, 张洪涛, 等. 双节段腰椎间盘突出症的“责任靶点”诊断和内窥镜治疗 [J]. 中国矫形外科杂志, 2018, 26(11):967-971. |
| [20] | Wilmink JT. The normal aging spine and degenerative spinal disease [J]. Neuroradiology, 2011, 53(Suppl 1):S181-183. |
| [21] |
Ekman P, Möller H, Shalabi A, et al. A prospective randomised study on the long-term effect of lumbar fusion on adjacent disc degeneration [J]. Eur Spine J, 2009, 18(8):1175-1186.
doi: 10.1007/s00586-009-0947-3 pmid: 19337757 |
| [1] | 林国中,马长城,吴超,司雨. 经锁孔入路显微外科切除腰椎管肿瘤54例临床研究[J]. 北京大学学报(医学版), 2022, 54(2): 315-319. |
| [2] | 许志锋,凌云鹏,崔仲奇,赵鸿,宫一辰,傅元豪,杨航,万峰. 经左胸前外侧微创冠脉搭桥治疗冠心病多支病变[J]. 北京大学学报(医学版), 2020, 52(5): 863-869. |
| [3] | 熊盛炜,王杰,朱伟杰,程嗣达,张雷,李学松,周利群. 二次肾盂成形术在复发性肾盂输尿管连接部梗阻中的研究进展[J]. 北京大学学报(医学版), 2020, 52(4): 794-798. |
| [4] | 易端,朱薇,孟秀丽,刘晓光,李水清,祝斌,贾东林. 慢性腰腿痛患者微创术前焦虑,抑郁状态及相关影响因素分析[J]. 北京大学学报(医学版), 2020, 52(2): 285-289. |
| [5] | 段登辉,王恩博,崔念晖,翟新利,刘宇,孟娟红,张伟,张益. 下颌阻生智齿拔除手术的可预期微创化[J]. 北京大学学报(医学版), 2020, 52(2): 395-403. |
| [6] | 丁光璞,程嗣达,方冬,杨昆霖,李学松,周辉霞,张骞,叶雄俊,周利群. 上尿路微创手术的技术改良[J]. 北京大学学报(医学版), 2019, 51(4): 610-614. |
| [7] | 熊盛炜,杨昆霖,丁光璞,郝瀚,李学松,周利群,郭应禄. 输尿管损伤外科修复治疗的研究进展[J]. 北京大学学报(医学版), 2019, 51(4): 783-789. |
| [8] | 刘冰川,杨钟玮,周方,姬洪全,张志山,郭琰,田耘. 肱骨近端骨折微创锁定钢板改良内固定的疗效分析[J]. 北京大学学报(医学版), 2019, 51(2): 277-282. |
| [9] | 张铃福,侯纯升,黄永辉,徐智,王立新,凌晓锋,王港,崔龙,修典荣. 胃空肠吻合术后胆总管结石腹腔镜手术取石和内镜取石的比较[J]. 北京大学学报(医学版), 2019, 51(2): 345-348. |
| [10] | 张鲁锋,凌云鹏, 杨航, 宫一辰, 宋之明, 万峰. 两种微创旁路移植手术治疗多支冠状动脉病变效果的对比[J]. 北京大学学报(医学版), 2017, 49(6): 1066-1070. |
| [11] | 徐杰,庄伟达,李新炜,俞国雨,林院,罗奋棋,肖毓华. 直接前入路和后外侧保留梨状肌入路全髋关节置换术的疗效对比[J]. 北京大学学报(医学版), 2017, 49(2): 214-220. |
| [12] | 张洪,马云青. 直接前入路人工全髋关节置换术[J]. 北京大学学报(医学版), 2017, 49(2): 185-187. |
| [13] | 赵丽萍, 詹雅琳, 胡文杰, 王浩杰, 危伊萍, 甄敏, 徐涛, 刘云松. 磨牙位点保存后进行种植修复及软组织增量的1例报告[J]. 北京大学学报(医学版), 2016, 48(6): 1090-1094. |
| [14] | 刘波,陈山林,朱瑾,王志新,杨辰,沈杰,田光磊. 腕关节镜辅助微创治疗月骨周围脱位[J]. 北京大学学报(医学版), 2016, 48(2): 234-236. |
| [15] | 张英泽. 观察、思考与创新在我国骨科发展中的重要作用[J]. 北京大学学报(医学版), 2016, 48(2): 189-190. |
|
||