北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (1): 119-125. doi: 10.19723/j.issn.1671-167X.2022.01.019
种植体周病非手术治疗中联合应用甘氨酸粉喷砂的临床效果评价
- 北京大学口腔医学院·口腔医院牙周科,国家口腔医学中心,国家口腔疾病临床医学研究中心,口腔数字化医疗技术和材料国家工程实验室,国家卫生健康委员会口腔医学计算机应用工程技术研究中心,北京 100081
Efficacy of combined application of glycine powder air-polishing in non-surgical treatment of peri-implant diseases
Fei SUN,Si-qi LI,Yi-ping WEI,Jin-sheng ZHONG,Cui WANG( ),Wen-jie HU(
),Wen-jie HU( )
)
- Department of Periodontology, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry, Beijing 100081, China
摘要:
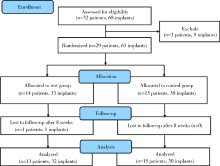
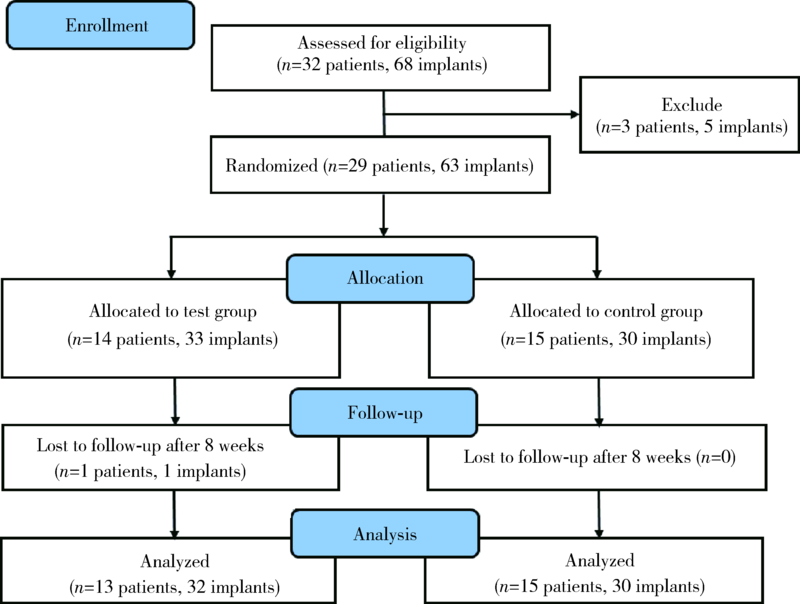
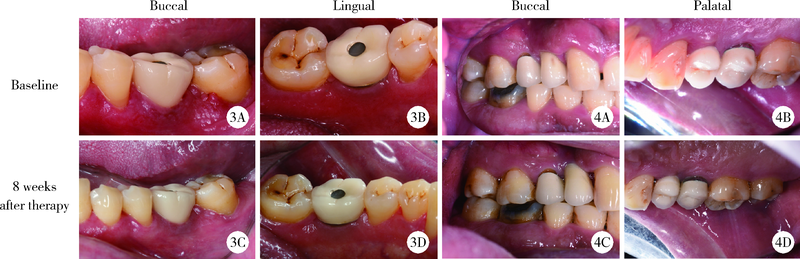
目的: 比较单纯手工黏膜下刮治与联合应用甘氨酸粉喷砂在非手术治疗种植体周病中的临床疗效。方法: 本研究为随机临床对照研究,研究对象为2020年5月至2021年6月就诊于北京大学口腔医院牙周科的种植体周病患者。共纳入28例患者的62颗种植体,采用随机数字表法将患者随机分为试验组和对照组,其中试验组(13例/32颗种植体)采用钛刮治器行黏膜下刮治联合应用甘氨酸粉喷砂治疗,对照组(15例/30颗种植体)单纯使用钛刮治器行黏膜下刮治。分别记录基线期和治疗后8周种植体周探诊深度(peri-implant probing depth,PPD)、出血指数(bleeding index,BI)、菌斑指数(plaque index,PLI)和探诊溢脓种植体占该组总种植体数目的百分比(suppuration on probing %,SoP%),比较治疗前后种植体周临床指标的变化及治疗后组间差异。结果: 治疗后8周两组种植体的平均PLI、PPD、BI均下降,差异具有统计学意义(P<0.05)。与对照组相比,治疗后试验组BI更低(2.7±0.8 vs. 2.2±0.7,P<0.05),BI改善值更大(0.6±0.7 vs. 1.1±0.6,P<0.01),SoP%降低更多(21.9% vs. 10.0%, P<0.05),差异均具有统计学意义。其中罹患种植体周黏膜炎的种植体,试验组BI及SoP%改善值大于对照组(1.0±0.7 vs. 0.4±0.7,P=0.02;6.3% vs. 0,P=0.012),差异具有统计学意义,而两组间PLI和PPD改善值差异均无统计学意义(P>0.05)。罹患种植体周炎的种植体,两组间PLI、PPD、BI及SoP%改善值差异均无统计学意义(P>0.05)。结论: 联合应用甘氨酸粉喷砂和单纯手工黏膜下刮治均可改善种植体周软组织炎症,而前者在改善种植体周软组织出血及探诊溢脓,特别是罹患种植体周黏膜炎的效果方面更佳。
中图分类号:
- R781.42
| [1] |
Howe M-S, Keys W, Richards D. Long-term (10-year) dental implant survival: A systematic review and sensitivity meta-analysis[J]. J Dent, 2019, 84:9-21.
doi: 10.1016/j.jdent.2019.03.008 |
| [2] |
Adler L, Buhlin K, Jansson L. Survival and complications: A 9- to 15-year retrospective follow-up of dental implant therapy[J]. J Oral Rehabil, 2020, 47(1):67-77.
doi: 10.1111/joor.v47.1 |
| [3] |
Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology[J]. J Clin Periodontol, 2015, 42(Suppl 16):S158-S171.
doi: 10.1111/jcpe.12334 |
| [4] |
Lupi SM, Granati M, Butera A, et al. Air-abrasive debridement with glycine powder versus manual debridement and chlorhexidine administration for the maintenance of peri-implant health status: A six-month randomized clinical trial[J]. Int J Dent Hyg, 2017, 15(4):287-294.
doi: 10.1111/idh.12206 pmid: 26842543 |
| [5] |
Jepsen S, Berglundh T, Genco R, et al. Primary prevention of peri-implantitis: Managing peri-implant mucositis[J]. J Clin Periodontol, 2015, 42(Suppl 16):S152-S157.
doi: 10.1111/jcpe.12369 |
| [6] | 靖无迪, 王宪娥, 谢也斯, 等. 甘氨酸龈下喷砂治疗早期种植体周围病的疗效观察[J]. 中华口腔医学杂志, 2017, 52(8):480-485. |
| [7] |
Sahm N, Becker J, Santel T, et al. Non-surgical treatment of peri-implantitis using an air-abrasive device or mechanical debridement and local application of chlorhexidine: A prospective, randomized, controlled clinical study[J]. J Clin Periodontol, 2011, 38(9):872-878.
doi: 10.1111/jcpe.2011.38.issue-9 |
| [8] |
Berglundh T, Armitage G, Araujo M G, et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions[J]. J Clin Periodontol, 2018, 45(Suppl 20):S286-S291.
doi: 10.1111/jcpe.2018.45.issue-S20 |
| [9] |
Shrivastava D, Natoli V, Srivastava KC, et al. Novel approach to dental biofilm management through guided biofilm therapy (GBT): A review[J]. Microorganisms, 2021, 9(9):1966.
doi: 10.3390/microorganisms9091966 |
| [10] | Renvert S, Quirynen M. Risk indicators for peri-implantitis. A narrative review[J]. Clin Oral Implants Res, 2015, 26(Suppl 11):15-44. |
| [11] |
Renvert S, Polyzois I. Risk indicators for peri-implant mucositis: A systematic literature review[J]. J Clin Periodontol, 2015, 42(Suppl 16):S172-S186.
doi: 10.1111/jcpe.12346 |
| [12] |
Steiger-Ronay V, Merlini A, Wiedemeier DB, et al. Location of unaccessible implant surface areas during debridement in simulated peri-implantitis therapy[J]. BMC Oral Health, 2017, 17(1):137.
doi: 10.1186/s12903-017-0428-8 pmid: 29183313 |
| [13] | Cha JK, Paeng K, Jung UW, et al. The effect of five mechanical instrumentation protocols on implant surface topography and roughness: A scanning electron microscope and confocal laser scanning microscope analysis[J]. Clin Oral Implants Res, 2019, 30(6):578-587. |
| [14] |
Tong Z, Fu R, Zhu W, et al. Changes in the surface topography and element proportion of clinically failed SLA implants after in vitro debridement by different methods[J]. Clin Oral Implants Res, 2021, 32(3):263-273.
doi: 10.1111/clr.v32.3 |
| [15] | Ronay V, Merlini A, Attin T, et al. In vitro cleaning potential of three implant debridement methods. Simulation of the non-surgical approach[J]. Clin Oral Implants Res, 2017, 28(2):151-155. |
| [16] |
Schwarz F, Becker K, Renvert S. Efficacy of air polishing for the non-surgical treatment of peri-implant diseases: A systematic review[J]. J Clin Periodontol, 2015, 42(10):951-959.
doi: 10.1111/jcpe.12454 pmid: 26362615 |
| [17] | Ji YJ, Tang ZH, Wang R, et al. Effect of glycine powder air-polishing as an adjunct in the treatment of peri-implant mucositis: A pilot clinical trial[J]. Clin Oral Implants Res, 2014, 25(6):683-689. |
| [18] |
Iatrou P, Chamilos C, Nickles K, et al. In vitro efficacy of three different nonsurgical implant surface decontamination methods in three different defect configurations[J]. Int J Oral Maxillofac Implants, 2021, 36(2):271-280.
doi: 10.11607/jomi.8864 |
| [19] |
John G, Sahm N, Becker J, et al. Nonsurgical treatment of peri-implantitis using an air-abrasive device or mechanical debridement and local application of chlorhexidine. Twelve-month follow-up of a prospective, randomized, controlled clinical study[J]. Clin Oral Investig, 2015, 19(8):1807-1814.
doi: 10.1007/s00784-015-1406-7 |
| [20] | Heitz-Mayfield LJ, Trombelli L, Heitz F, et al. A systematic review of the effect of surgical debridement vs. non-surgical debridement for the treatment of chronic periodontitis[J]. J Clin Perio-dontol, 2002, 29(Suppl 3):92-102. |
| [1] | 张瑶,郭金鑫,战世佳,洪恩宇,杨慧,贾安娜,常艳,郭永丽,张璇. 富含半胱氨酸和甘氨酸蛋白2在神经母细胞瘤恶性进展中的功能和机制[J]. 北京大学学报(医学版), 2024, 56(3): 495-504. |
| [2] | 孙菲,刘建,李思琪,危伊萍,胡文杰,王翠. 种植体黏膜下微生物在健康种植体和种植体周炎中的构成与差异:一项横断面研究[J]. 北京大学学报(医学版), 2023, 55(1): 30-37. |
| [3] | 孟令玮,李雪,高胜寒,李悦,曹瑞涛,张毅,潘韶霞. 三种方法建立大鼠种植体周炎模型的比较[J]. 北京大学学报(医学版), 2023, 55(1): 22-29. |
| [4] | 刘意,王赛楠,崔彩云,董艳梅. 精氨酸-甘氨酸-天冬氨酸-丝氨酸序列在生物活性玻璃对人牙髓细胞生物作用中的影响[J]. 北京大学学报(医学版), 2017, 49(2): 326-330. |
| [5] | 吕冬梅. 肺部给药疫苗装置的研究进展[J]. 北京大学学报(医学版), 2012, 44(5): 683-687. |
|
||