Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (4): 678-683. doi: 10.19723/j.issn.1671-167X.2019.04.014
Previous Articles Next Articles
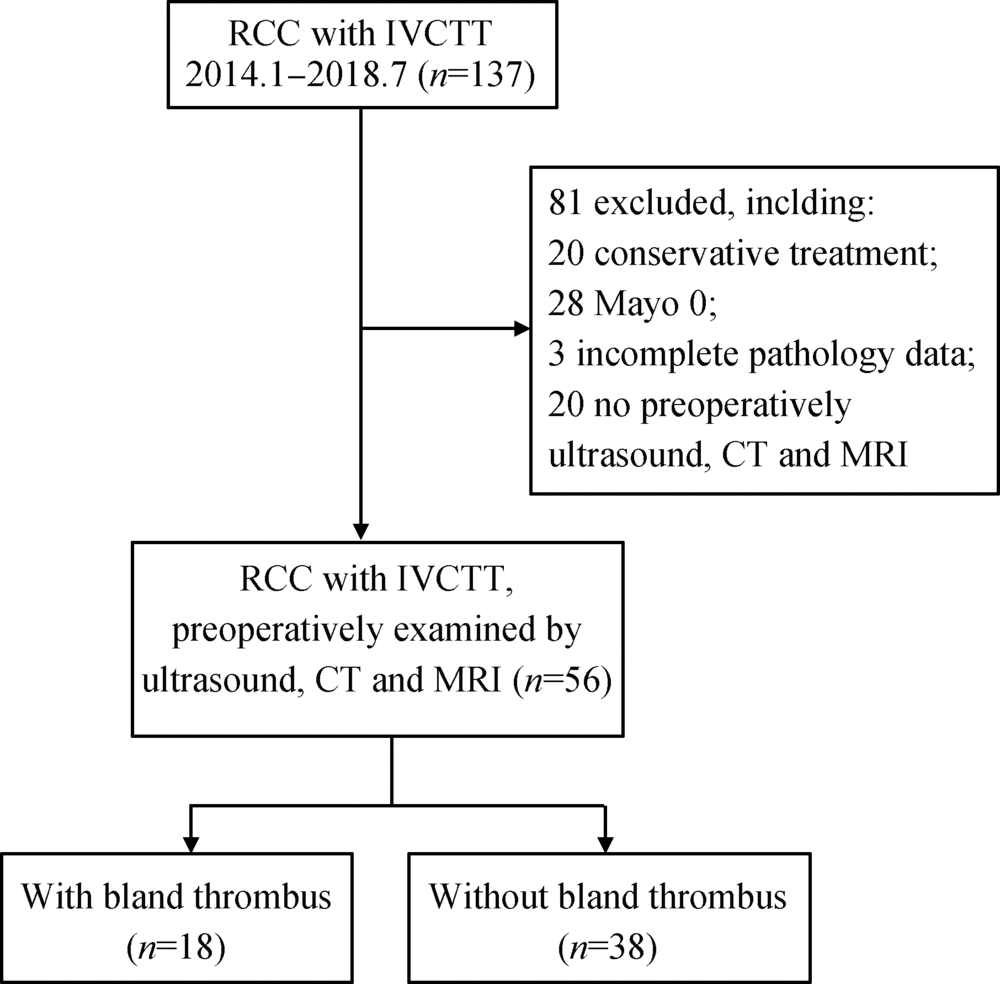
Comparison of various imaging in the diagnosis of renal cell carcinoma with inferior vena cava tumor thrombus combined with bland thrombus
Li-wei LI1,Zhuo LIU2,Guo-liang WANG2,Hua ZHANG3,Wen CHEN1,Jing MA1,Li ZHANG1,Wei HE4,Lu-lin MA2,△( ),Shu-min WANG1,△(
),Shu-min WANG1,△( )
)
- 1. Department of Ultrasound, Peking University Third Hospital, Beijing 100191, China
2. Department of Urology, Peking University Third Hospital, Beijing 100191, China
3. Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing 100191, China
4. Department of Radiology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R737.1
| [1] | 刘茁, 马潞林, 田晓军 , 等. 根治性肾切除术+下腔静脉癌栓取出术治疗Mayo 0~Ⅳ 级下腔静脉癌栓的临床经验[J]. 中华泌尿外科杂志, 2017,38(11):842-847. |
| [2] | 刘茁, 马潞林, 田晓军 , 等. 肾癌根治性切除加癌栓取出术治疗Mayo Ⅲ 级下腔静脉癌栓的手术技术及临床经验[J]. 北京大学学报(医学版), 2017,49(4):597-602. |
| [3] | 刘茁, 田晓军, 马潞林 . 根治性肾切除术联合Mayo 0-Ⅱ 级静脉癌栓取出术的临床麻醉管理[J]. 现代肿瘤医学, 2017,25(16):2672-2677. |
| [4] | 刘茁, 马潞林, 田晓军 , 等. 腹腔镜和开放肾癌根治性切除+Mayo Ⅱ 级下腔静脉癌栓取出术11例临床分析[J]. 现代泌尿外科杂志, 2017,22(8):603-607. |
| [5] | 马潞林, 刘茁 . 肾癌并肝段和肝以上下腔静脉癌栓的诊治体会[J]. 中华泌尿外科杂志, 2017,38(7):481-484. |
| [6] | Blute ML, Leibovich BC, Lohse CM , et al. The mayo clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus[J] . BJU Int, 2004,94(1):33-41. |
| [7] | Wang M, Ping H, Niu Y , et al. Pure conventional laparoscopic radical nephrectomy with level II vena cava tumor thrombectomy[J]. Int Braz J Urol, 2014,40(2):266-273. |
| [8] | 程艳, 蔡欣, 刘基巍 . 恶性肿瘤与血栓形成[J]. 临床肿瘤学杂志, 2010,15(4):376-379. |
| [9] | Ayyathurai R, Garciaroig M, Gorin MA , et al. Bland thrombus association with tumour thrombus in renal cell carcinoma: Analysis of surgical significance and role of inferior vena caval interruption[J]. BJU Int, 2013,110(11b):E449-E455. |
| [10] | Hutchinson R, Rew C, Chen G , et al. The adverse survival implications of bland thrombus in renal cell carcinoma with venous tumor thrombus[J]. Urology, 2018,115:119-124. |
| [11] | Blute ML, Boorjian SA, Leibovich BC , et al. Results of inferior vena caval interruption by greenfield filter, ligation or resection during radical nephrectomy and tumor thrombectomy[J]. J Urol, 2007,178(2):440-445. |
| [12] | 马鑫 . 机器人腹腔镜腔静脉瘤栓取出术:新的思考新的策略[J]. 中华腔镜外科杂志: 电子版, 2017,10(5):272-273. |
| [13] | Quencer KB, Friedman T, Sheth R , et al. Tumor thrombus: Incidence, imaging, prognosis and treatment[J]. Cardiovasc Diagn Ther, 2017,7(Suppl 3):S165-S177. |
| [14] | Mukai M, Oka T . Mechanism and management of cancer-associated thrombosis[J]. J Cardiol, 2018,72(2):89-93. |
| [15] | 肾癌伴静脉瘤栓北京专家共识[J]. 微创泌尿外科杂志, 2017: 6(6):321-327. |
| [16] | 宋奕宁, 赵艺超, 李建国 . 下腔静脉肿瘤的超声影像诊断与鉴别[J]. 中国超声医学杂志, 2018,34(1):37-39. |
| [17] | Tarantino L . Contrast-enhanced ultrasound in differentiating malignant from benign portal vein thrombosis in hepatocellular carcinoma[J]. World J Gastroenterol, 2015,21(32):9457-9460. |
| [18] | Sonavane SN, Malhotra G, Asopa R , et al. Role of fluorine-18 fluorodeoxyglucose positron emission tomography in a case of renal cell carcinoma to differentiate tumor thrombus from bland thrombus[J]. Indian J Nucl Med, 2015,30(4):355-357. |
| [19] | Sharma P, Kumar R, Jeph S , et al. 18F-FDG PET-CT in the diagnosis of tumor thrombus[J]. Nucl Med Commun, 2011,32(9):782-788. |
| [1] | Fan SHU,Yichang HAO,Zhanyi ZHANG,Shaohui DENG,Hongxian ZHANG,Lei LIU,Guoliang WANG,Xiaojun TIAN,Lei ZHAO,Lulin MA,Shudong ZHANG. Functional and oncologic outcomes of partial nephrectomy for cystic renal cell carcinoma: A single-center retrospective study [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 667-672. |
| [2] | Zezhen ZHOU,Shaohui DENG,Ye YAN,Fan ZHANG,Yichang HAO,Liyuan GE,Hongxian ZHANG,Guoliang WANG,Shudong ZHANG. Predicting the 3-year tumor-specific survival in patients with T3a non-metastatic renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 673-679. |
| [3] | Yun-chong LIU,Zong-long WU,Li-yuan GE,Tan DU,Ya-qian WU,Yi-meng SONG,Cheng LIU,Lu-lin MA. Mechanism of nuclear protein 1 in the resistance to axitinib in clear cell renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 781-792. |
| [4] | Dong LAN,Zhuo LIU,Yu-xuan LI,Guo-liang WANG,Xiao-jun TIAN,Lu-lin MA,Shu-dong ZHANG,Hong-xian ZHANG. Risk factors for massive hemorrhage after radical nephrectomy and removal of venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 825-832. |
| [5] | Yun-yi XU,Zheng-zheng SU,Lin-mao ZHENG,Meng-ni ZHANG,Jun-ya TAN,Ya-lan YANG,Meng-xin ZHANG,Miao XU,Ni CHEN,Xue-qin CHEN,Qiao ZHOU. Read-through circular RNA rt-circ-HS promotes hypoxia inducible factor 1α expression and renal carcinoma cell proliferation, migration and invasiveness [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 217-227. |
| [6] | Qi SHEN,Yi-xiao LIU,Qun HE. Mucinous tubular and spindle cell carcinoma of kidney: Clinicopathology and prognosis [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 276-282. |
| [7] | Quan ZHANG,Hai-feng SONG,Bing-lei MA,Zhe-nan ZHANG,Chao-hui ZHOU,Ao-lin LI,Jun LIU,Lei LIANG,Shi-yu ZHU,Qian ZHANG. Pre-operative prognostic nutritional index as a predictive factor for prognosis in non-metastatic renal cell carcinoma treated with surgery [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 149-155. |
| [8] | Yang LIU,Fang CHENG,Yan-ling WANG,Xiang-yan AI,Zhen-hang ZHU,Fu-tao ZHAO. Diagnostic performances of salivary gland ultrasonography for Sjögren's syndrome [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1123-1127. |
| [9] | Shu-heng ZHAI,Pan-pan HU,Xiao-guang LIU. Intraoperative ultrasound assisted circumferential decompression for multilevel ossification of the posterior longitudinal ligament in thoracic vertebrae [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 1021-1027. |
| [10] | Er-shu BO,Peng HONG,Yu ZHANG,Shao-hui DENG,Li-yuan GE,Min LU,Nan LI,Lu-lin MA,Shu-dong ZHANG. Clinicopathological features and prognostic analysis of papillary renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 615-620. |
| [11] | Tian-yu CAI,Zhen-peng ZHU,Chun-ru XU,Xing JI,Tong-de LV,Zhen-ke GUO,Jian LIN. Expression and significance of fibroblast growth factor receptor 2 in clear cell renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 628-635. |
| [12] | Mei-ni ZUO,Yi-qing DU,Lu-ping YU,Xiang DAI,Tao XU. Correlation between metabolic syndrome and prognosis of patients with clear cell renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 636-643. |
| [13] | Cai-peng QIN,Yu-xuan SONG,Meng-ting DING,Fei WANG,Jia-xing LIN,Wen-bo YANG,Yi-qing DU,Qing LI,Shi-jun LIU,Tao XU. Establishment of a mutation prediction model for evaluating the efficacy of immunotherapy in renal carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 663-668. |
| [14] | DENG Xue-rong,SUN Xiao-ying,ZHANG Zhuo-li. Agreement between ultrasound-detected inflammation and clinical signs in ankles and feet joints in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1037-1042. |
| [15] | SONG Zhi-bo,GENG Yan,DENG Xue-rong,ZHANG Xiao-hui,ZHANG Zhuo-li. Benefit of ultrasound in the phenotype recognition of psoriatic arthritis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1061-1066. |
|
||