Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (1): 9-15. doi: 10.19723/j.issn.1671-167X.2021.01.003
Previous Articles Next Articles
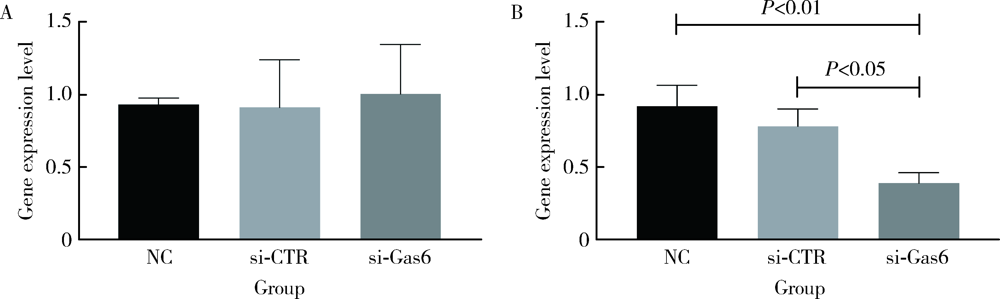
Role of growth arrest-specific protein 6 in migration and osteogenic differentiation of human periodontal ligament cells
ZHANG Sheng-nan1,AN Na2,Δ( ),OUYANG Xiang-ying1,Δ(
),OUYANG Xiang-ying1,Δ( ),LIU Ying-jun2,WANG Xue-kui1
),LIU Ying-jun2,WANG Xue-kui1
- 1. Department of Periodontology, , Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
2. Department of General Dentistry Ⅱ, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R781.42
| [1] |
Jönsson D, Nebel D, Bratthall G, et al. The human periodontal ligament cell: A fibroblast-like cell acting as an immune cell[J]. J Periodontal Res, 2011,46(2):153-157.
doi: 10.1111/j.1600-0765.2010.01331.x |
| [2] |
Somerman MJ, Young MF, Foster RA, et al. Characteristics of human periodontal ligament cells in vitro[J]. Arch Oral Biol, 1990,35(3):241-247.
doi: 10.1016/0003-9969(90)90062-f pmid: 2161648 |
| [3] |
Liu F, Wang X, Zheng B, et al. USF2 enhances the osteogenic differentiation of PDLCs by promoting ATF4 transcriptional activities[J]. J Periodontal Res, 2020,55(1):68-76.
doi: 10.1111/jre.12689 pmid: 31448831 |
| [4] |
Manokawinchoke J, Pavasant P, Sawangmake C, et al. Intermittent compressive force promotes osteogenic differentiation in human periodontal ligament cells by regulating the transforming growth factor-β pathway[J]. Cell Death Dis, 2019,10(10):761.
doi: 10.1038/s41419-019-1992-4 pmid: 31591384 |
| [5] |
Xu Y, Ren C, Zhao X, et al. MicroRNA-132 inhibits osteogenic differentiation of periodontal ligament stem cells via GDF5 and the NF-κB signaling pathway[J]. Pathol Res Pract, 2019,215(12):152722.
doi: 10.1016/j.prp.2019.152722 pmid: 31718857 |
| [6] |
Liu S, Zhou M, Li J, et al. LIPUS inhibited the expression of inflammatory factors and promoted the osteogenic differentiation capacity of hPDLCs by inhibiting the NF-κB signaling pathway[J]. J Periodontal Res, 2020,55(1):125-140.
doi: 10.1111/jre.12696 pmid: 31541455 |
| [7] |
Schneider C, King RM, Philipson L. Genes specifically expressed at growth arrest of mammalian cells[J]. Cell, 1988,54(6):787-793.
doi: 10.1016/s0092-8674(88)91065-3 pmid: 3409319 |
| [8] |
Manfioletti G, Brancolini C, Avanzi G, et al. The protein encoded by a growth arrest-specific gene (gas6) is a new member of the vitamin K-dependent proteins related to protein S, a negative coregulator in the blood coagulation cascade[J]. Mol Cell Biol, 1993,13(8):4976-4985.
doi: 10.1128/mcb.13.8.4976 pmid: 8336730 |
| [9] | 刘颖君, 欧阳翔英, 安娜, 等. 生长停滞特异性蛋白6在牙龈卟啉单胞菌脂多糖诱导内皮细胞黏附分子及趋化因子表达中的作用[J]. 北京大学学报(医学版), 2018,50(1):20-25. |
| [10] |
Collett G, Wood A, Alexander MY, et al. Receptor tyrosine kinase Axl modulates the osteogenic differentiation of pericytes[J]. Circ Res, 2003,92(10):1123-1129.
doi: 10.1161/01.RES.0000074881.56564.46 pmid: 12730092 |
| [11] |
Katagiri M, Hakeda Y, Chikazu D, et al. Mechanism of stimulation of osteoclastic bone resorption through Gas6/Tyro 3, a receptor tyrosine kinase signaling, in mouse osteoclasts[J]. J Biol Chem, 2001,276(10):7376-7382.
doi: 10.1074/jbc.M007393200 pmid: 11084030 |
| [12] |
Kim YS, Jung SH, Jung DH, et al. Gas6 stimulates angiogenesis of human retinal endothelial cells and of zebrafish embryos via ERK1/2 signaling[J]. PLoS One, 2014,9(1):e83901.
doi: 10.1371/journal.pone.0083901 pmid: 24409287 |
| [13] |
Mao S, Wu Y, Wang R, et al. Overexpression of GAS6 promotes cell proliferation and invasion in bladder cancer by activation of the PI3K/AKT pathway[J]. Onco Targets Ther, 2020,13:4813-4824.
doi: 10.2147/OTT.S237174 pmid: 32547108 |
| [14] |
Lemke G. Biology of the TAM receptors[J]. Cold Spring Harb Perspect Biol, 2013,5(11):a009076.
doi: 10.1101/cshperspect.a009076 pmid: 24186067 |
| [15] |
Xu J, Li Z, Hou Y, et al. Potential mechanisms underlying the Runx2 induced osteogenesis of bone marrow mesenchymal stem cells[J]. Am J Transl Res, 2015,7(12):2527-2535.
pmid: 26885254 |
| [16] |
Ciceri P, Elli F, Braidotti P, et al. Iron citrate reduces high phosphate-induced vascular calcification by inhibiting apoptosis[J]. Atherosclerosis, 2016,254:93-101.
doi: 10.1016/j.atherosclerosis.2016.09.071 pmid: 27716569 |
| [17] |
Badi I, Mancinelli L, Polizzotto A, et al. miR-34a promotes vascular smooth muscle cell calcification by downregulating SIRT1 (Sirtuin 1) and Axl (AXL receptor tyrosine kinase)[J]. Arterioscler Thromb Vasc Biol, 2018,38(9):2079-2090.
doi: 10.1161/ATVBAHA.118.311298 pmid: 30026277 |
| [18] |
Goruppi S, Ruaro E, Varnum B, et al. Gas6-mediated survival in NIH3T3 cells activates stress signalling cascade and is independent of Ras[J]. Oncogene, 1999,18(29):4224-4236.
doi: 10.1038/sj.onc.1202788 pmid: 10435635 |
| [19] | Hasanbasic I, Cuerquis J, Varnum B, et al. Intracellular signaling pathways involved in Gas6-Axl-mediated survival of endothelial cells[J]. Am J Physiol Heart Circ Physiol, 2004,287(3):1207-1213. |
| [20] |
Allen MP, Linseman DA, Udo H, et al. Novel mechanism for gonadotropin-releasing hormone neuronal migration involving Gas6/Ark signaling to p38 mitogen-activated protein kinase[J]. Mol Cell Biol, 2002,22(2):599-613.
doi: 10.1128/mcb.22.2.599-613.2002 pmid: 11756555 |
| [21] |
Li H, Deng Y, Tan M, et al. Low-intensity pulsed ultrasound upregulates osteogenesis under inflammatory conditions in periodontal ligament stem cells through unfolded protein response[J]. Stem Cell Res Ther, 2020,11(1):215.
doi: 10.1186/s13287-020-01732-5 pmid: 32493507 |
| [22] |
Chang M, Lin H, Fu H, et al. MicroRNA-195-5p regulates osteogenic differentiation of periodontal ligament cells under mechanical loading[J]. J Cell Physiol, 2017,232(12):3762-3774.
doi: 10.1002/jcp.25856 pmid: 28181691 |
| [1] | Yuanzhi JIAN,Fei WANG,Ning YIN,Ruoyu ZHOU,Junbo WANG. Developmental toxicity of Cry1Ab protein in the embryonic stem-cell model [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 213-222. |
| [2] | Yuan PAN,Hang GU,Han XIAO,Lijun ZHAO,Yiman TANG,Wenshu GE. Ubiquitin-specific protease 42 regulates osteogenic differentiation of human adipose-derived stem cells [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 9-16. |
| [3] | XUE Jiang,ZHANG Jian-yun,SHI Rui-rui,XIE Xiao-yan,BAI Jia-ying,LI Tie-jun. Clinicopathological analysis of 105 patients with fibrous dysplasia of cranio-maxillofacial region [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 54-61. |
| [4] | DU Wen-yu,YANG Jing-wen,JIANG Ting. Early constant observation of the effect of deferoxamine mesylate on improvement of vascularized bone regeneration in SD rat skull critical size defect model [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1171-1177. |
| [5] | GAO Hong-yu,MENG Huan-xin,HOU Jian-xia,HUANG Bao-xin,LI Wei. Expression and distribution of calprotectin in healthy and inflamed periodontal tissues [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 744-749. |
| [6] | WANG Jing-qi,WANG Xiao. In vivo study of strontium-doped calcium phosphate cement for biological properties [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 378-383. |
| [7] | Mei WANG, Bo-wen LI, Si-wen WANG, Yu-hua LIU. Preparation and osteogenic effect study of small intestinal submucosa sponge [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 952-958. |
| [8] | Ying CHEN,Zhong-ning LIU,Bo LI,Ting JIANG. Preparation of aspirin sustained-release microsphere and its in vitro releasing [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 907-912. |
| [9] | SUI Hua-xin, LV Pei-jun, WANG Yong, FENG Yu-chi. Effects of low level laser irradiation on the osteogenic capacity of sodium alginate/gelatin/human adipose-derived stem cells 3D bio-printing construct [J]. Journal of Peking University(Health Sciences), 2018, 50(5): 868-875. |
| [10] | ZHU Yun-yan, LI Qian, ZHANG Yi-mei, ZHOU Yan-heng. Decreased phosphorylation of mitogen activated protein kinase and protein kinase B contribute to the inhibition of osteogenic differentiation mediated by activation of Toll like receptor in human periodontal ligament stem cells#br# [J]. Journal of Peking University(Health Sciences), 2018, 50(1): 33-41. |
| [11] | LIU Jing-yin, CHEN Fei, GE Yan-jun, WEI Ling, PAN Shao-xia, FENG Hai-lan. Influence of implants prepared by selective laser melting on early bone healing [J]. Journal of Peking University(Health Sciences), 2018, 50(1): 117-122. |
| [12] | . Stress change of periodontal ligament of the anterior teeth at the stage of space closure in lingual appliances: a 3-dimensional finite element analysis [J]. Journal of Peking University(Health Sciences), 2018, 50(1): 141-147. |
| [13] | SUI Hua-xin, LV Pei-jun, WANG Yu-guang, WANG Yong, SUN Yu-chun. Effect of lowlevel laser irradiation on proliferation and osteogenic differentiation of human adipose-derived stromal cells [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 337-343. |
| [14] | ZHAO Yi-jiao, WANG Si-wei, LIU Yi, WANG Yong. A method for rapid extracting three-dimensional root model of vivo tooth from cone beam computed tomography data based on the anatomical characteristics of periodontal ligament [J]. Journal of Peking University(Health Sciences), 2017, 49(1): 54-059. |
| [15] | LING Long, ZHAO Yu-ming, GE Li-hong. Impact of different degree pulpitis on cell proliferation and osteoblastic differentiation of dental pulp stem cell in Beagle immature premolars [J]. Journal of Peking University(Health Sciences), 2016, 48(5): 878-883. |
|
||