Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (6): 1097-1104. doi: 10.19723/j.issn.1671-167X.2023.06.022
Previous Articles Next Articles
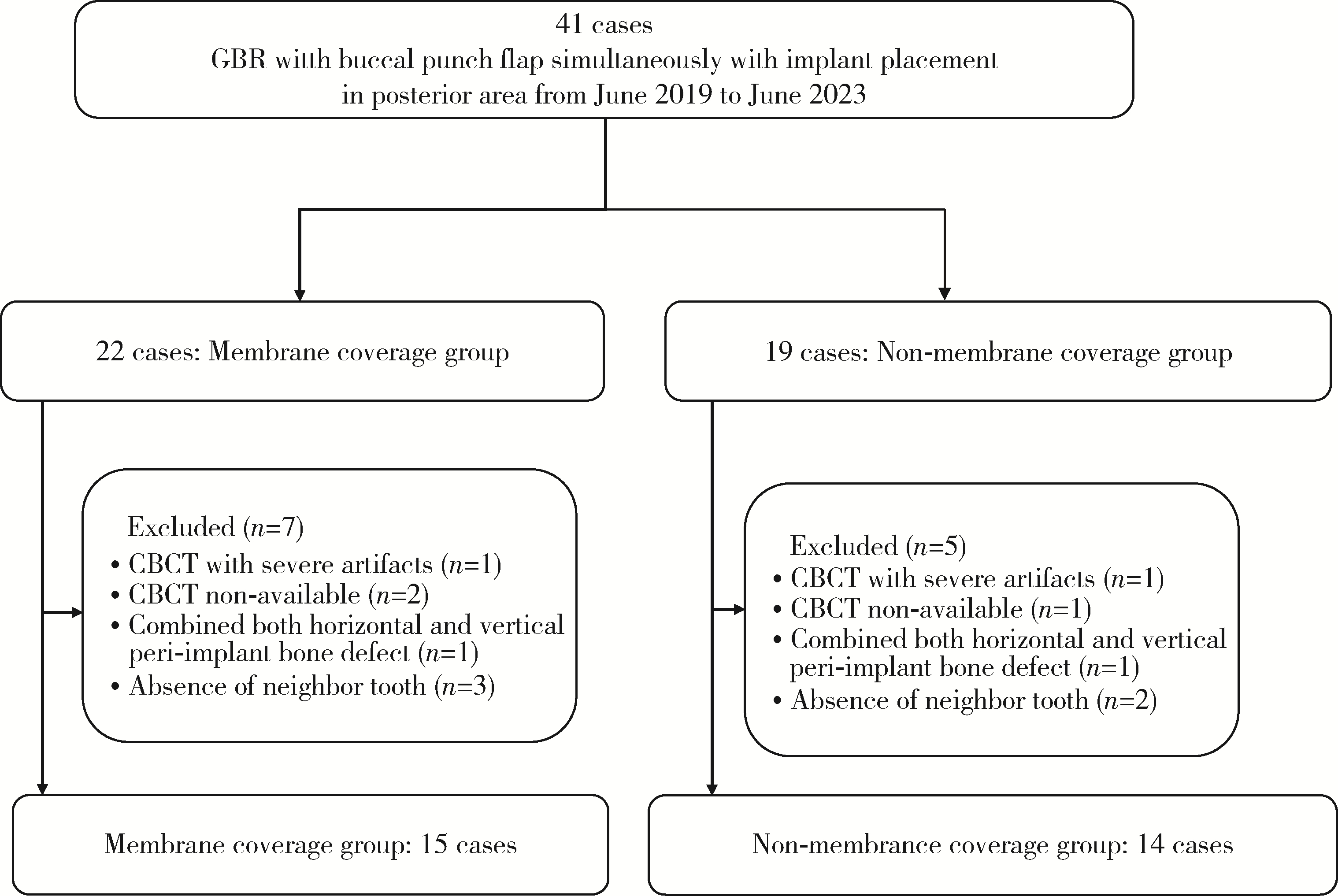
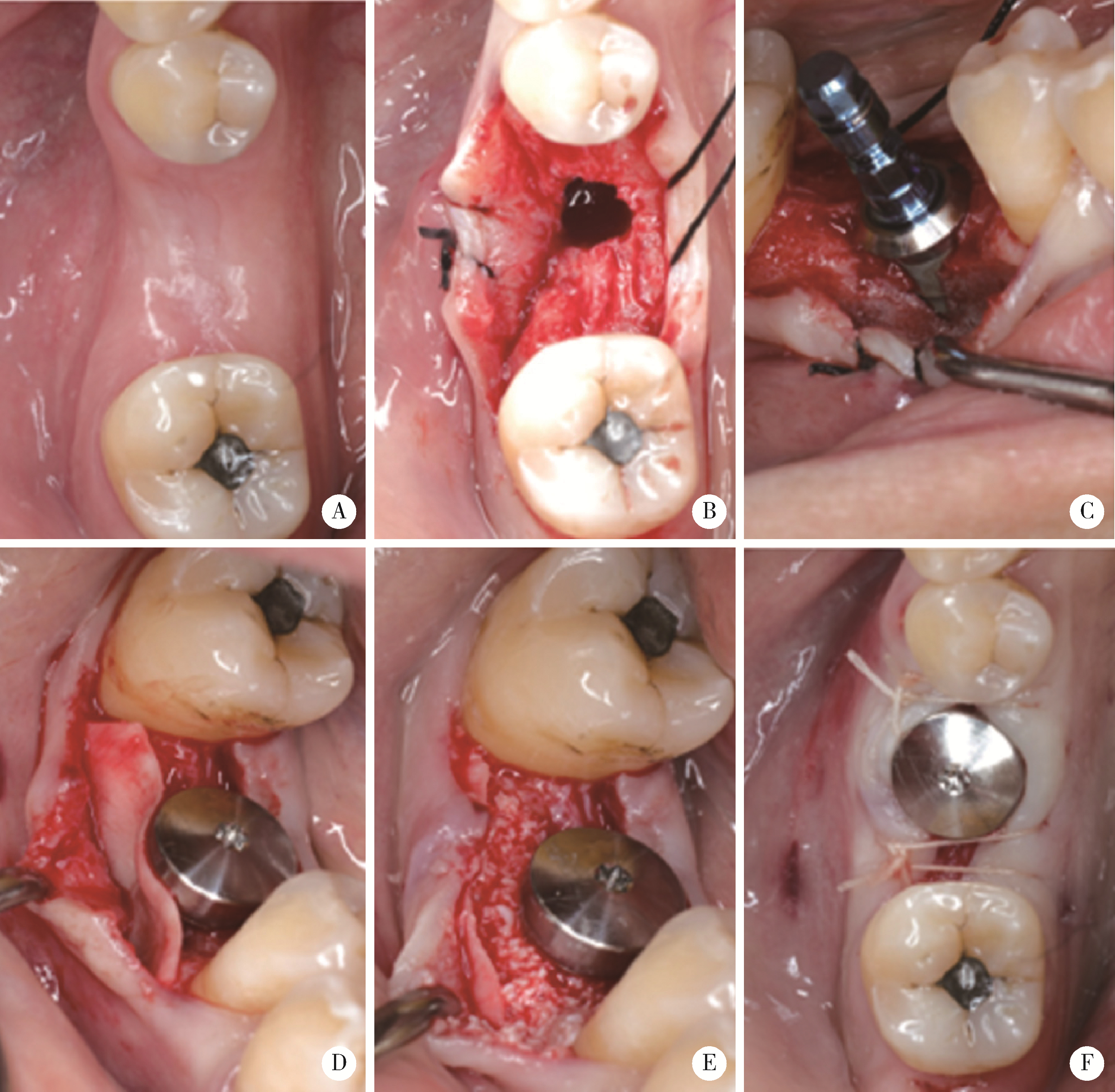
Role of collagen membrane in modified guided bone regeneration surgery using buccal punch flap approach: A retrospective and radiographical cohort study
Deng-hui DUAN1,Hom-Lay WANG2,En-bo WANG1,*( )
)
- 1. Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center for Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
2. Department of Periodontics and Oral Medicine, School of Dentistry, University of Michigan, Ann Arbor, MI, 48109, USA
CLC Number:
- R782.13
| 1 | Hammerle CH , Jung RE , Feloutzis A . A systematic review of the survival of implants in bone sites augmented with barrier membranes (guided bone regeneration) in partially edentulous patients[J]. J Clin Periodontol, 2002, 29 (Suppl 3): 226- 231. |
| 2 | Thoma DS , Bienz SP , Figuero E , et al. Efficacy of lateral bone augmentation performed simultaneously with dental implant placement: A systematic review and meta-analysis[J]. J Clin Perio-dontol, 2019, 46 (Suppl 21): 257- 276. |
| 3 |
Jung RE , Fenner N , Hämmerle CH , et al. Long-term outcome of implants placed with guided bone regeneration (GBR) using resorbable and non-resorbable membranes after 12-14 years[J]. Clin Oral Implants Res, 2013, 24 (10): 1065- 1073.
doi: 10.1111/j.1600-0501.2012.02522.x |
| 4 | Benic GI , Thoma DS , Jung RE , et al. Guided bone regeneration with particulate vs. block xenogenic bone substitutes: A pilot cone beam computed tomographic investigation[J]. Clin Oral Implants Res, 2017, 28 (11): e262- e270. |
| 5 |
Fu JH , Oh TJ , Benavides E , et al. A randomized clinical trial evaluating the efficacy of the sandwich bone augmentation technique in increasing buccal bone thickness during implant placement surgery: Ⅰ. Clinical and radiographic parameters[J]. Clin Oral Implants Res, 2014, 25 (4): 458- 467.
doi: 10.1111/clr.12171 |
| 6 | Ye GH , Duan DH , Wang EB . Ridge volume stability of maxillary anterior implants placed with simultaneous lateral guided bone regeneration during healing: A radiographic analysis[J]. Chin J Dent Res, 2021, 24 (4): 251- 256. |
| 7 |
Wang HL , Boyapati L . "PASS" principles for predictable bone regeneration[J]. Implant Dent, 2006, 15 (1): 8- 17.
doi: 10.1097/01.id.0000204762.39826.0f |
| 8 |
César Neto JB , Cavalcanti MC , Sapata VM , et al. The positive effect of tenting screws for primary horizontal guided bone regeneration: A retrospective study based on cone-beam computed tomography data[J]. Clin Oral Implants Res, 2020, 31 (9): 846- 855.
doi: 10.1111/clr.13630 |
| 9 |
Farias D , Caceres F , Sanz A , et al. Horizontal bone augmentation in the posterior atrophic mandible and dental implant stability using the tenting screw technique[J]. Int J Periodontics Restorative Dent, 2021, 41 (4): e147- e155.
doi: 10.11607/prd.5137 |
| 10 |
Duan DH , Wang HL , Xiao WC , et al. Bone regeneration using titanium plate stabilization for the treatment of peri-implant bone defects: A retrospective radiologic pilot study[J]. Clin Implant Dent Relat Res, 2022, 24 (6): 792- 800.
doi: 10.1111/cid.13139 |
| 11 |
Ciocca L , Lizio G , Baldissara P , et al. Prosthetically CAD-CAM-guided bone augmentation of atrophic jaws using customized tita-nium mesh: Preliminary results of an open prospective study[J]. J Oral Implantol, 2018, 44 (2): 131- 137.
doi: 10.1563/aaid-joi-D-17-00125 |
| 12 |
Her S , Kang T , Fien MJ . Titanium mesh as an alternative to a membrane for ridge augmentation[J]. J Oral Maxillofac Surg, 2012, 70 (4): 803- 810.
doi: 10.1016/j.joms.2011.11.017 |
| 13 |
Lee SR , Jang TS , Seo CS , et al. Hard tissue volume stability effect beyond the bony envelope of a three-dimensional preformed titanium mesh with two different collagen barrier membranes on peri-implant dehiscence defects in the anterior maxilla: A rando-mized clinical trial[J]. Materials (Basel), 2021, 14 (19): 5618.
doi: 10.3390/ma14195618 |
| 14 |
Sumida T , Otawa N , Kamata YU , et al. Custom-made titanium devices as membranes for bone augmentation in implant treatment: Clinical application and the comparison with conventional titanium mesh[J]. J Craniomaxillofac Surg, 2015, 43 (10): 2183- 2188.
doi: 10.1016/j.jcms.2015.10.020 |
| 15 |
Lin Z , Fateh A , Salem DM , et al. Periosteum: Biology and applications in craniofacial bone regeneration[J]. J Dent Res, 2014, 93 (2): 109- 116.
doi: 10.1177/0022034513506445 |
| 16 | Duan DH , Wang HL , Wang EB . Effect of intact periosteum on alveolar ridge contour stability after horizontal guided bone regene-ration in posterior region: A retrospective and radiographical cohort study[J]. Chin J Dent Res, 2023, 26 (4): 229- 236. |
| 17 |
Deng C , Yi Z , Xiong C , et al. Using the intact periosteum for horizontal bone augmentation of peri-implant defects: A retrospective cohort study[J]. Br J Oral Maxillofac Surg, 2022, 60 (10): 1325- 1331.
doi: 10.1016/j.bjoms.2022.09.012 |
| 18 |
Dahlin C , Linde A , Gottlow J , et al. Healing of bone defects by guided tissue regeneration[J]. Plast Reconstr Surg, 1988, 81 (5): 672- 676.
doi: 10.1097/00006534-198805000-00004 |
| 19 | Dahlin C , Sennerby L , Lekholm U , et al. Generation of new bone around titanium implants using a membrane technique: An experimental study in rabbits[J]. Int J Oral Maxillofac Implants, 1989, 4 (1): 19- 25. |
| 20 | Becker W , Becker BE , Handlesman M , et al. Bone formation at dehisced dental implant sites treated with implant augmentation material: A pilot study in dogs[J]. Int J Periodontics Restorative Dent, 1990, 10 (2): 92- 101. |
| 21 |
Louis PJ , Gutta R , Said-Al-Naief N , et al. Reconstruction of the maxilla and mandible with particulate bone graft and titanium mesh for implant placement[J]. J Oral Maxillofac Surg, 2008, 66 (2): 235- 245.
doi: 10.1016/j.joms.2007.08.022 |
| 22 |
Atef M , Tarek A , Shaheen M , et al. Horizontal ridge augmentation using native collagen membrane vs titanium mesh in atrophic maxillary ridges: Randomized clinical trial[J]. Clin Implant Dent Relat Res, 2020, 22 (2): 156- 166.
doi: 10.1111/cid.12892 |
| 23 |
Urban IA , Saleh MHA , Ravidà A , et al. Vertical bone augmentation utilizing a titanium-reinforced PTFE mesh: A multi-variate analysis of influencing factors[J]. Clin Oral Implants Res, 2021, 32 (7): 828- 839.
doi: 10.1111/clr.13755 |
| 24 |
Benic GI , Bienz SP , Song YW , et al. Randomized controlled clinical trial comparing guided bone regeneration of peri-implant defects with soft-type block versus particulate bone substitutes: Six-month results of hard-tissue changes[J]. J Clin Periodontol, 2022, 49 (5): 480- 495.
doi: 10.1111/jcpe.13606 |
| 25 |
Park SH , Lee KW , Oh TJ , et al. Effect of absorbable membranes on sandwich bone augmentation[J]. Clin Oral Implants Res, 2008, 19 (1): 32- 41.
doi: 10.1111/j.1600-0501.2007.01408.x |
| 26 |
Spray JR , Black CG , Morris HF , et al. The influence of bone thickness on facial marginal bone response: Stage 1 placement through stage 2 uncovering[J]. Ann Periodontol, 2000, 5 (1): 119- 128.
doi: 10.1902/annals.2000.5.1.119 |
| 27 |
Botticelli D , Berglundh T , Lindhe J . Hard-tissue alterations following immediate implant placement in extraction sites[J]. J Clin Periodontol, 2004, 31 (10): 820- 828.
doi: 10.1111/j.1600-051X.2004.00565.x |
| 28 |
Severi M , Simonelli A , Farina R , et al. Effect of lateral bone augmentation procedures in correcting peri-implant bone dehiscence and fenestration defects: A systematic review and network meta-analysis[J]. Clin Implant Dent Relat Res, 2022, 24 (2): 251- 264.
doi: 10.1111/cid.13078 |
| 29 |
Park JC , Kim CS , Choi SH , et al. Flap extension attained by vertical and periosteal-releasing incisions: A prospective cohort study[J]. Clin Oral Implants Res, 2012, 23 (8): 993- 998.
doi: 10.1111/j.1600-0501.2011.02244.x |
| 30 |
Monje A , Pons R , Vilarrasa J , et al. Significance of barrier membrane on the reconstructive therapy of peri-implantitis: A rando-mized controlled trial[J]. J Periodontol, 2023, 94 (3): 323- 335.
doi: 10.1002/JPER.22-0511 |
| [1] | Shishi BO,Chengzhi GAO. Tooth segmentation and identification on cone-beam computed tomography with convolutional neural network based on spatial embedding information [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 735-740. |
| [2] | Xiaotong LING,Liuyang QU,Danni ZHENG,Jing YANG,Xuebing YAN,Denggao LIU,Yan GAO. Three-dimensional radiographic features of calcifying odontogenic cyst and calcifying epithelial odontogenic tumor [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 131-137. |
| [3] | Han ZHAO,Yan WEI,Xuehui ZHANG,Xiaoping YANG,Qing CAI,Chengyun NING,Mingming XU,Wenwen LIU,Ying HUANG,Ying HE,Yaru GUO,Shengjie JIANG,Yunyang BAI,Yujia WU,Yusi GUO,Xiaona ZHENG,Wenjing LI,Xuliang DENG. Bionic design, preparation and clinical translation of oral hard tissue restorative materials [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 4-8. |
| [4] | Xiaoqiang LIU,Yin ZHOU. Risk factors of perioperative hypertension in dental implant surgeries with bone augmentation [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 93-98. |
| [5] | Jin-hua ZHANG,Jie PAN,Zhi-peng SUN,Xiao WANG. Effect of various intracanal materials on the diagnostic accuracy of cone-beam computed tomography in vertical root fractures [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 333-338. |
| [6] | Jia-xue YE,Yu-hong LIANG. A prevalence survey of cone-beam computed tomography use among endodontic practitioners [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 114-119. |
| [7] | Meng-qiao PAN,Jian LIU,Li XU,Xiao XU,Jian-xia HOU,Xiao-tong LI,Xiao-xia WANG. A long-term evaluation of periodontal phenotypes before and after the periodontal-orthodontic-orthognathic combined treatment of lower anterior teeth in patients with skeletal Angle class Ⅲ malocclusion [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 52-61. |
| [8] | Yu FU,Xin-nong HU,Sheng-jie CUI,Jie SHI. Decompensation effectiveness and alveolar bone remodeling analysis of mandibular anterior teeth after preoperative orthodontic treatment in high-angle patients with skeletal class Ⅱ malocclusion [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 62-69. |
| [9] | Juan GAO,Hang-miao LV,Hui-min MA,Yi-jiao ZHAO,Xiao-tong LI. Evaluation of root resorption after surgical orthodontic treatment of skeletal Class Ⅲ malocclusion by three-dimensional volumetric measurement with cone-beam CT [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 719-726. |
| [10] | LIU Wei-tao,WANG Yi-ran,WANG Xue-dong,ZHOU Yan-heng. A cone-beam computed tomography evaluation of three-dimensional changes of circummaxillary sutures following maxillary protraction with alternate rapid palatal expansions and constrictions [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 346-355. |
| [11] | Gang YANG,Wen-jie HU,Jie CAO,Deng-gao LIU. Three-dimensional morphology analysis of the supraosseous gingival profile of periodontally healthy maxillary anterior teeth [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 990-994. |
| [12] | YOU Peng-yue,LIU Yu-hua,WANG Xin-zhi,WANG Si-wen,TANG Lin. Biocompatibility and effect on bone formation of a native acellular porcine pericardium: Results of in vitro and in vivo [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 776-784. |
| [13] | WANG Si-wen,YOU Peng-yue,LIU Yu-hua,WANG Xin-zhi,TANG Lin,WANG Mei. Efficacy of two barrier membranes and deproteinized bovine bone mineral on bone regeneration in extraction sockets: A microcomputed tomographic study in dogs [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 364-370. |
| [14] | MENG Yuan,ZHANG Li-qi,ZHAO Ya-ning,LIU Deng-gao,ZHANG Zu-yan,GAO Yan. Three-dimentional radiographic features of 67 maxillary radicular cysts [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 396-401. |
| [15] | ZHOU Jing,LIU Yi. Cone-beam CT evaluation of temporomandibular joint in skeletal class Ⅱ female adolescents with different vertical patterns [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 109-119. |
|
||