Journal of Peking University (Health Sciences) ›› 2025, Vol. 57 ›› Issue (2): 272-276. doi: 10.19723/j.issn.1671-167X.2025.02.008
Previous Articles Next Articles
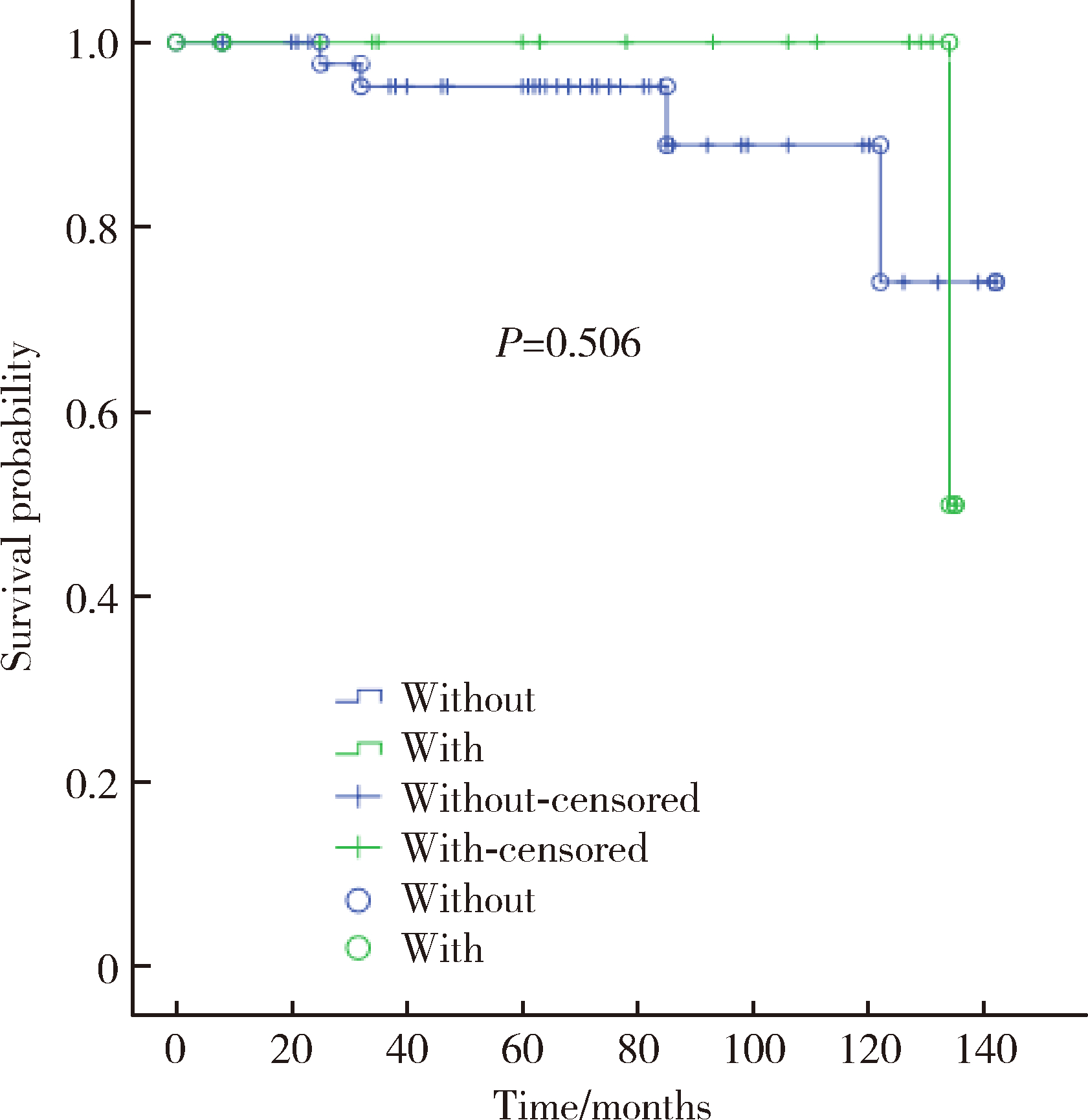
Effect of intraoperative blood salvage autotransfusion on the prognosis of patients after carotid body tumor resection
Weihao LI, Jing LI, Xuemin ZHANG, Wei LI, Qingle LI, Xiaoming ZHANG*( )
)
- Department of Vascular Surgery, Peking University People's Hospital, Beijing 100044, China
CLC Number:
- R457.1
| 1 |
郭红磊, 贾彦焘. 颈动脉体瘤临床诊疗研究进展[J]. 临床误诊误治, 2021, 34 (3): 108- 112.
doi: 10.3969/j.issn.1002-3429.2021.03.021 |
| 2 |
Moore MG , Netterville JL , Mendenhall WM , et al. Head and neck paragangliomas: An update on evaluation and management[J]. Otolaryngol Head Neck Surg, 2016, 154 (4): 597- 605.
doi: 10.1177/0194599815627667 |
| 3 | 顾光超, 郑月宏. 颈动脉体瘤的影像学检查及外科治疗进展[J]. 血管与腔内血管外科杂志, 2020, 6 (5): 439- 441. |
| 4 |
Butt N , Baek WK , Lachkar S , et al. The carotid body and associated tumors: Updated review with clinical/surgical significance[J]. Br J Neurosurg, 2019, 33 (5): 500- 503.
doi: 10.1080/02688697.2019.1617404 |
| 5 | 马赫, 黄燕娟. 术中回收式自体输血技术适应症的应用[J]. 中南医学科学杂志, 2017, 45 (2): 186- 188. |
| 6 |
李红霞, 韩志强, 钟海燕. 回收式自体输血对肿瘤手术患者预后的影响[J]. 临床输血与检验, 2018, 20 (1): 106- 108.
doi: 10.3969/j.issn.1671-2587.2018.01.036 |
| 7 |
李晶, 蒋京军, 张小明, 等. 颈动脉转流管在复杂颈动脉体瘤手术切除中的应用[J]. 中国普通外科杂志, 2018, 27 (12): 1556- 1562.
doi: 10.7659/j.issn.1005-6947.2018.12.010 |
| 8 | 孔祥国, 李楠, 杨建勇, 等. 术前经导管动脉栓塞对ShamblinⅡ/Ⅲ型颈动脉体瘤切除术的影响[J]. 中山大学学报(医学科学版), 2021, 42 (2): 287- 293. |
| 9 | 吴朋, 吕国士. 64排CT增强扫描结合血管成像对恶性颈动脉体瘤的诊断价值分析[J]. 中国全科医学, 2013, 16 (3): 354- 356. |
| 10 | Mascia D , Esposito G , Ferrante A , et al. Carotid body tumor contemporary management in a high-volume center[J]. J Cardiovasc Surg (Torino), 2020, 61 (4): 459- 466. |
| 11 |
Gu G , Wu X , Ji L , et al. Proposed modification to the Shamblin's classification of carotid body tumors: A single-center retrospective experience of 116 tumors[J]. Eur J Surg Oncol, 2021, 47 (8): 1953- 1960.
doi: 10.1016/j.ejso.2021.03.244 |
| 12 |
Chen Y , Li Y , Liu J , et al. The clinical characteristics and outcomes of carotid body tumors in Chinese patients: A STROBE-compliant observational study[J]. Medicine (Baltimore), 2020, 99 (3): e18824.
doi: 10.1097/MD.0000000000018824 |
| 13 |
Illuminati G , Pasqua R , Nardi P , et al. Results of resection of carotid body tumors with and without lymphnodes' dissection[J]. Surg Oncol, 2021, 37, 101555.
doi: 10.1016/j.suronc.2021.101555 |
| 14 |
王凤明, 章文成, 张仑. 15例恶性颈动脉体瘤的诊断与治疗[J]. 中国肿瘤临床, 2007, 34 (20): 1185- 1187.
doi: 10.3969/j.issn.1000-8179.2007.20.013 |
| 15 |
陶英杰, 刘经祖, 金锐. 10例恶性颈动脉体瘤之生物学行为分析[J]. 中国肿瘤临床, 2001, 28 (4): 288- 289.
doi: 10.3969/j.issn.1000-8179.2001.04.015 |
| 16 | 廖蓉仙, 徐雪梅, 吕豪. 2010—2018年衢州市回收式自体输血发展与思考[J]. 浙江临床医学, 2020, 22 (3): 461- 462. |
| 17 |
汪晓晓, 郭建荣. 自体输血在老年患者手术中的应用价值及风险分析[J]. 临床输血与检验, 2021, 23 (2): 259- 262.
doi: 10.3969/j.issn.1671-2587.2021.02.027 |
| 18 |
Kumar N , Ravikumar N , Tan JYH , et al. Current status of the use of salvaged blood in metastatic spine tumour surgery[J]. Neurospine, 2018, 15 (3): 206- 215.
doi: 10.14245/ns.1836140.070 |
| 19 | 聂晓红, 闫瑞琪, 胡强夫, 等. 术中自体血回输对原发性良性脑膜瘤全切术后肿瘤复发的影响[J]. 广东医学, 2020, 41 (9): 956- 958. |
| 20 |
Bower MR , Ellis SF , Scoggins CR , et al. Phase Ⅱ comparison study of intraoperative autotransfusion for major oncologic procedures[J]. Ann Surg Oncol, 2011, 18 (1): 166- 173.
doi: 10.1245/s10434-010-1228-4 |
| 21 | Elmalky M , Yasin N , Rodrigues-Pinto R , et al. The safety, efficacy, and cost-effectiveness of intraoperative cell salvage in metastatic spine tumor surgery[J]. Spine J, 2017, 17 (7): 977- 982. |
| 22 |
Kinnear N , O'Callaghan M , Hennessey D , et al. Intra-operative cell salvage in urological surgery: A systematic review and meta-analysis of comparative studies[J]. BJU Int, 2019, 123 (2): 210- 219.
doi: 10.1111/bju.14373 |
| 23 |
胡晓云, 陈愉, 赵斌江. 等容血液稀释在颈动脉体瘤手术中的应用[J]. 中国输血杂志, 2000, 13 (4): 251- 252.
doi: 10.3969/j.issn.1004-549X.2000.04.014 |
| 24 | 陈述, 潘静. 稀释法自体输血在颈动脉体瘤手术中的应用(附2例报告)[J]. 齐鲁医学杂志, 2003, 18 (1): 84. |
| [1] | Yaqing MAO, Zhen CHEN, Yao YU, Wenbo ZHANG, Yang LIU, Xin PENG. Impact of type 2 diabetes mellitus on the prognosis of patients with oral squamous cell carcinoma [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 1089-1096. |
| [2] | Junyong OU,Kunming NI,Lulin MA,Guoliang WANG,Ye YAN,Bin YANG,Gengwu LI,Haodong SONG,Min LU,Jianfei YE,Shudong ZHANG. Prognostic factors of patients with muscle invasive bladder cancer with intermediate-to-high risk prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 582-588. |
| [3] | Shuai LIU,Lei LIU,Zhuo LIU,Fan ZHANG,Lulin MA,Xiaojun TIAN,Xiaofei HOU,Guoliang WANG,Lei ZHAO,Shudong ZHANG. Clinical treatment and prognosis of adrenocortical carcinoma with venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 624-630. |
| [4] | Le YU,Shaohui DENG,Fan ZHANG,Ye YAN,Jianfei YE,Shudong ZHANG. Clinicopathological characteristics and prognosis of multilocular cystic renal neoplasm of low malignant potential [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 661-666. |
| [5] | Zezhen ZHOU,Shaohui DENG,Ye YAN,Fan ZHANG,Yichang HAO,Liyuan GE,Hongxian ZHANG,Guoliang WANG,Shudong ZHANG. Predicting the 3-year tumor-specific survival in patients with T3a non-metastatic renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 673-679. |
| [6] | Yangyi FANG,Qiang LI,Zhigao HUANG,Min LU,Kai HONG,Shudong ZHANG. Well-differentiated papillary mesothelial tumour of the tunica vaginalis: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 741-744. |
| [7] | Yuanyuan ZENG,Yun XIE,Daonan CHEN,Ruilan WANG. Related factors of euthyroid sick syndrome in patients with sepsis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 526-532. |
| [8] | Jian-bin LI,Meng-na LYU,Qiang CHI,Yi-lin PENG,Peng-cheng LIU,Rui WU. Early prediction of severe COVID-19 in patients with Sjögren’s syndrome [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1007-1012. |
| [9] | Huan-rui LIU,Xiang PENG,Sen-lin LI,Xin GOU. Risk modeling based on HER-2 related genes for bladder cancer survival prognosis assessment [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 793-801. |
| [10] | Zi-xuan XUE,Shi-ying TANG,Min QIU,Cheng LIU,Xiao-jun TIAN,Min LU,Jing-han DONG,Lu-lin MA,Shu-dong ZHANG. Clinicopathologic features and prognosis of young renal tumors with tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 802-811. |
| [11] | Han LU,Jian-yun ZHANG,Rong YANG,Le XU,Qing-xiang LI,Yu-xing GUO,Chuan-bin GUO. Clinical factors affecting the prognosis of lower gingival squamous cell carcinoma [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 702-707. |
| [12] | Yun-fei SHI,Hao-jie WANG,Wei-ping LIU,Lan MI,Meng-ping LONG,Yan-fei LIU,Yu-mei LAI,Li-xin ZHOU,Xin-ting DIAO,Xiang-hong LI. Analysis of clinicopathological and molecular abnormalities of angioimmunoblastic T-cell lymphoma [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 521-529. |
| [13] | Xiao-juan ZHU,Hong ZHANG,Shuang ZHANG,Dong LI,Xin LI,Ling XU,Ting LI. Clinicopathological features and prognosis of breast cancer with human epidermal growth factor receptor 2 low expression [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 243-253. |
| [14] | Yu-mei LAI,Zhong-wu LI,Huan LI,Yan WU,Yun-fei SHI,Li-xin ZHOU,Yu-tong LOU,Chuan-liang CUI. Clinicopathological features and prognosis of anorectal melanoma: A report of 68 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 262-269. |
| [15] | Qi SHEN,Yi-xiao LIU,Qun HE. Mucinous tubular and spindle cell carcinoma of kidney: Clinicopathology and prognosis [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 276-282. |
|
||