Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (1): 133-138. doi: 10.19723/j.issn.1671-167X.2021.01.020
Previous Articles Next Articles
Chinese morphological stages of midpalatal suture and its correlation with Demirjian dental age
- Department of Orthodontics, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R783.5
| [1] |
Bjork A. Sutural growth of the upper face studied by the implant method[J]. Acta Odontol Scand, 1966,24(2):109-127.
doi: 10.3109/00016356609026122 pmid: 5225742 |
| [2] |
Melsen B. Palatal growth studied on human autopsy material[J]. Am J Orthod, 1975,68(1):42-54.
doi: 10.1016/0002-9416(75)90158-x pmid: 1056143 |
| [3] |
Persson M, Thilander B. Palatal suture closure in man from 15 to 35 years of age[J]. Am J Orthod, 1977,72(1):42-52.
doi: 10.1016/0002-9416(77)90123-3 pmid: 267435 |
| [4] |
Haas AJ. The treatment of maxillary deficiency by opening the midpalatal suture[J]. Angle Orthod, 1965,35:200-217.
doi: 10.1043/0003-3219(1965)035<0200:TTOMDB>2.0.CO;2 pmid: 14331020 |
| [5] |
McNamara JA Jr, Baccetti T, Franchi L, et al. Rapid maxillary expansion followed by fixed appliances: a long-term evaluation of changes in arch dimensions[J]. Angle Orthod, 2003,73(4):344-353.
doi: 10.1043/0003-3219(2003)073<0344:RMEFBF>2.0.CO;2 pmid: 12940553 |
| [6] |
Baccetti T, Franchi L, Cameron CG, et al. Treatment timing for rapid maxillary expansion[J]. Angle Orthod, 2001,71(5):343-350.
doi: 10.1043/0003-3219(2001)071<0343:TTFRME>2.0.CO;2 pmid: 11605867 |
| [7] |
Rungcharassaeng K, Caruso JM, Kan JY, et al. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion[J]. Am J Orthod Dentofacial Orthop, 2007,132(4):428.
doi: 10.1016/j.ajodo.2007.02.052 pmid: 17920493 |
| [8] |
Barber AF, Sims MR. Rapid maxillary expansion and external root resorption in man: A scanning electron microscope study[J]. Am J Orthod, 1981,79(6):630-652.
doi: 10.1016/0002-9416(81)90356-0 pmid: 7015868 |
| [9] |
Rinaldi MRL, Azeredo F, de Lima EM, et al. Cone-beam computed tomography evaluation of bone plate and root length after maxillary expansion using tooth-borne and tooth-tissue-borne banded expanders[J]. Am J Orthod Dentofacial Orthop, 2018,154(4):504-516.
doi: 10.1016/j.ajodo.2017.12.018 pmid: 30268261 |
| [10] |
Garib DG, Henriques JF, Janson G, et al. Rapid maxillary expansion: Tooth tissue-borne versus tooth-borne expanders. A computed tomography evaluation of dentoskeletal effects[J]. Angle Orthod, 2005,75(4):548-557.
doi: 10.1043/0003-3219(2005)75[548:RMETVT]2.0.CO;2 pmid: 16097223 |
| [11] | 高璐, 谷岩. 中国人群腭中缝生长发育形态特点分期与其相应生理年龄分布的初步研究[J]. 中华口腔正畸学杂志, 2020,27(2):61-66. |
| [12] |
Demirjian A, Goldstein H, Tanner JM. A new system of dental age assessment[J]. Hum Biol, 1973,45(2):211-227.
pmid: 4714564 |
| [13] |
Demirjian A, Goldstein H. New systems for dental maturity based on seven and four teeth[J]. Ann Hum Biol, 1976,3(5):411-421.
doi: 10.1080/03014467600001671 pmid: 984727 |
| [14] |
Macha M, Lamba B, Avula JSS, et al. Estimation of correlation between chronological age, skeletal age and dental age in children: a cross-sectional study [J]. J Clin Diagn Res, 2017, 11 (9): ZC01-ZC04.
doi: 10.7860/JCDR/2017/25175.10537 pmid: 29207822 |
| [15] |
李萌, 李果, 王虎. Demirjian牙龄推断法及其应用与更新[J]. 国际口腔医学杂志, 2014,41(6):725-729.
doi: 10.7518/gjkq.2014.06.026 |
| [16] |
Perinetti G, Contardo L, Gabrieli P, et al. Diagnostic performance of dental maturity for identification of skeletal maturation phase[J]. Eur J Orthod, 2011,34(4):487-492.
doi: 10.1093/ejo/cjr027 pmid: 21345927 |
| [17] | Proffit WR. Contemporary orthodontics[M]. 6th ed. Philadelphia: Elsevier, 2018. |
| [18] |
Ró$\dot{z}$yło-Kalinowska I, Kolasa-Rᶏczka A, Kalinowski P. Relationship between dental age according to Demirjian and cervical vertebrae maturity in Polish children[J]. Eur J Orthod, 2010,33(1):75-83.
doi: 10.1093/ejo/cjq031 pmid: 20558591 |
| [19] |
Ladewig VM, Capelozza-Filho L, Almeida-Pedrin RR, et al. Tomographic evaluation of the maturation stage of the midpalatal suture in post-adolescents[J]. Am J Orthod Dentofacial Orthop, 2018,153(6):818-824.
doi: 10.1016/j.ajodo.2017.09.019 pmid: 29853239 |
| [20] |
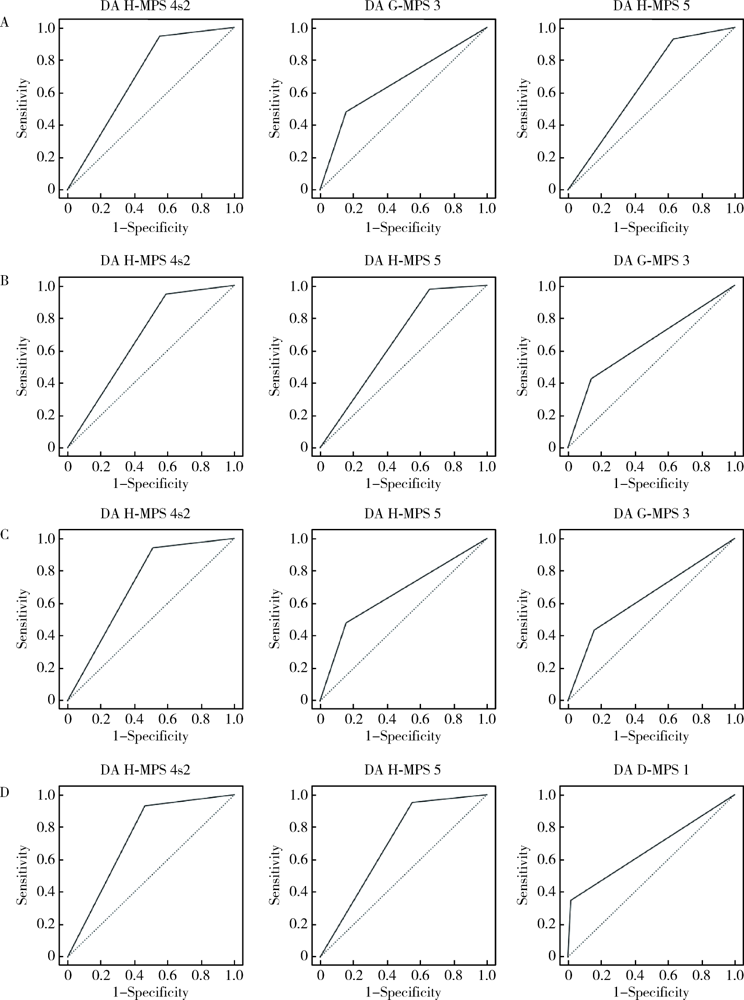
Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation[J]. Caspian J Intern Med, 2013,4(2):627-635.
pmid: 24009950 |
| [21] |
Korbmacher H, Schilling A, Puschel K, et al. Age-dependent three-dimensional micro-computed tomography analysis of the human midpalatal suture[J]. J Orofac Orthop, 2007,68(5):364-376.
doi: 10.1007/s00056-007-0729-7 |
| [22] |
Knaup B, Yildizhan F, Wehrbein H. Age-related changes in the midpalatal suture[J]. J Orofac Orthop, 2004,65(6):467-474.
doi: 10.1007/s00056-004-0415-y |
| [23] | 黄悦勤. 临床流行病学[M]. 4版. 北京: 人民卫生出版社, 2014. |
| [24] | 葛立宏. 儿童口腔医学[M]. 2版. 北京: 北京大学医学出版社, 2013. |
|
||