| [1] |
Soares CJ, Soares PV, de Freitas Santos-Filho PC, et al. The influence of cavity design and glass fiber posts on biomechanical behavior of endodontically treated premolars[J]. J Endod, 2008,34(8):1015-1019.
|
| [2] |
Savychuk A, Manda M, Galanis C , et al. Stress generation in mandibular anterior teeth restored with different types of post-and-core at various levels of ferrule[J]. J Prosthet Dent, 2018,119(6):965-974.
|
| [3] |
Strefezza C, Amaral MM, Quinto J Jr , et al. Effect of 830 nm diode laser irradiation of root canal on bond strength of metal and fiber post[J]. Photomed Laser Surq, 2018,36(8):439-444.
|
| [4] |
Goracci C, Tavares AU, Fabianelli A , et al. The adhesion between fiber posts and root canal walls: comparison between microtensile and push-out bond strength measurements[J]. Eur J Oral Sci, 2004,112(4):353-361.
|
| [5] |
Par M, Tarle Z, Hickel R , et al. Dentin bond strength of experimental composites containing bioactive glass: changes during aging for up to 1 year[J]. J Adhes Dent, 2018,20(4):325-334.
|
| [6] |
Garcia C, Ruales-Carrera E, Prates LH , et al. Effect of different irrigations on the bond strength of self-adhesive resin cement to root dentin[J]. J Clin Exp Dent, 2018,10(2):e139-e145.
|
| [7] |
Roydhouse RH . Punch-shear test for dental purposes[J]. J Dent Res, 1970,49:131-136.
|
| [8] |
Garcia PP, da Costa RG, Garcia AV , et al. Effect of surface treatments on the bond strength of CAD/CAM fiber glass posts[J]. J Clin Exp Dent, 2018,10(6):e591-e597.
|
| [9] |
Bohrer TC, Fontana PE, Wandscher VF , et al. Endodontic sealers affect the bong strength of fiber posts and the degree of conversion of two resin cements[J]. J Adhes Dent, 2018,20(2):165-172.
|
| [10] |
Tuncdemir AR, Buyukerkmen EB, Celebi H , et al. Effects of postsurface treatments including femtosecond laser and aluminum-oxide airborne-partical abrasion on the bond strength of the fiber posts[J]. Niqer J Clin Pract, 2018,21(3):350-355.
|
| [11] |
Shafiei F, Saadat M, Jowkar Z . Effect of laser heat treatment on Pull-out bond strength of fiber posts treated with different silanes[J]. J Clin Exp Dent, 2018,10(5):e413-e418.
|
| [12] |
Feilzer AJ, De Gee AJ, Davidson CL . Setting stress in composite resin in relation to configuration of the restoration[J]. J Dent Res, 1987,66(11):1636-1639.
|
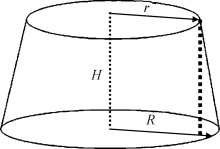
| [13] |
Tay FR, Loushine RJ, Lambrechts P , et al. Geometric factors affecting dentin bonding in root canals: a theoretical modeling approach[J]. J Endod, 2005,31(8):584-589.
|
| [14] |
Patierno JM, Rueggeberg FA, Anderson RW , et al. Push-out and SEM evaluation of resin composite bonded to internal cervical dentin[J]. J Endod Dent Traumatol, 1996,12(5):227-236.
|
| [15] |
Bolhuis P, De Gee A, Feilzer A . The influence of fatigue loading on the quality of the cement layer and retention strength of carbon fiber post resin composite core restorations[J]. Oper Dent, 2005,30(2):220-227.
|
| [16] |
Lin G, Geubelle PH, Sottos NR . Simulation of fiber debonding with friction in a model composite pushout test[J]. Int J Solids Struct, 2001,38(2):8547-8562.
|
| [17] |
Soares CJ, Santana FR, Castro CG , et al. Finite element analysis and bond strength of a glass post to intraradicular dentin: comparison between microtensile and push-out tests[J]. Dent Mater, 2008,24(10):1405-1411.
|
| [18] |
Belwalkar VR, Gade J, Mankar NP . Comparison of the effect of shear bond strength with silane and other three chemical presurface treatments of a glass fiber-reinforced post on adhesion with a resin-based luting agent: an in vitro study[J]. Contemp Clin Dent, 2016,7(2):193-197.
|
| [19] |
Pyun JH, Shin TB, Lee JH , et al. Effects of hydrogen peroxide pretreatment and heat activation of silane on the shear bond strength of fiber-reinforced composite posts to resin cement[J]. J Adv Prosthodont, 2016,8(2):94-100.
|
| [20] |
Cecchin D, Farina AP, Vitti RP , et al. Acid etching and surface coating of glass-fiber posts: bond strength and interface analysis[J]. Braz Dent J, 2016,27(2):228-233.
|
| [21] |
Mosharraf R, Baghaei Yazdi N . Comparative evaluation of effects of different surface treatment methods on bond strength between fiber post and composite core[J]. J Adv Prosthodont, 2012,4(2):103-108.
|
| [22] |
Aksornmuang J, Foxton RM, Nakajima M , et al. Microtensilebond strength of a dual cure resin core material to glass and quartz fibreposts[J]. J Dent, 2004,32(6):433-450.
|