北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (2): 303-308. doi: 10.19723/j.issn.1671-167X.2025.02.013
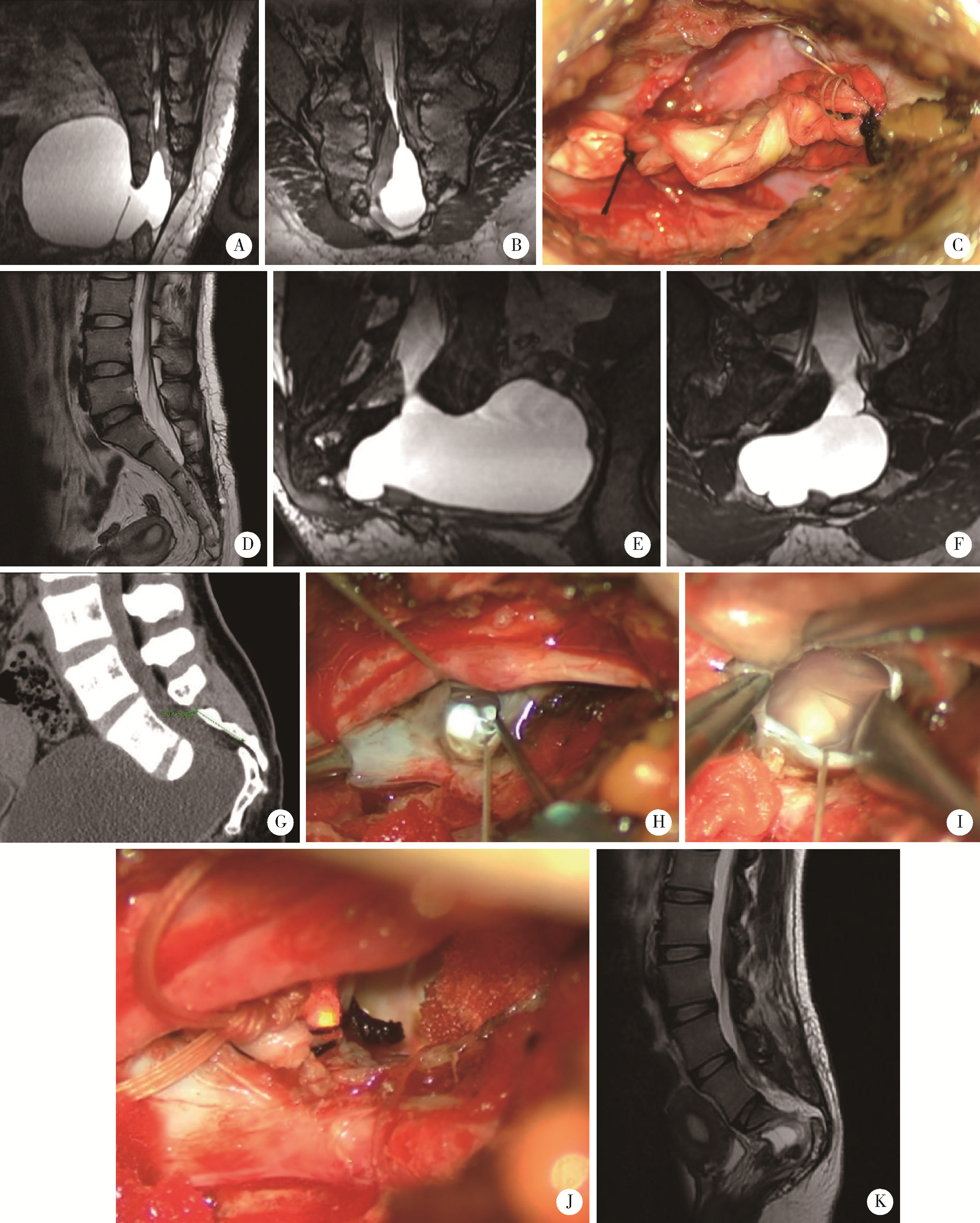
任意维度重建磁共振对骶管囊肿进行精准分型对于指导微创手术和康复的意义
孙建军1,2,*( ), 马千权1, 尹晓亮1, 杨辰龙1, 张嘉1, 陈素华1, 吴超1, 谢京城1, 韩芸峰1, 林国中1, 司雨1, 杨军1, 邬海博3, 赵强3
), 马千权1, 尹晓亮1, 杨辰龙1, 张嘉1, 陈素华1, 吴超1, 谢京城1, 韩芸峰1, 林国中1, 司雨1, 杨军1, 邬海博3, 赵强3
- 1. 北京大学第三医院神经外科,北京 100191
2. 首都医科大学附属北京友谊医院神经外科,北京 100050
3. 北京大学第三医院放射科,北京 100191
Significance of precise classification of sacral meningeal cysts by multiple dimensions radiographic reconstruction MRI in guiding operative strategy and rehabilitation
Jianjun SUN1,2,*( ), Qianquan MA1, Xiaoliang YIN1, Chenlong YANG1, Jia ZHANG1, Suhua CHEN1, Chao WU1, Jingcheng XIE1, Yunfeng HAN1, Guozhong LIN1, Yu SI1, Jun YANG1, Haibo WU3, Qiang ZHAO3
), Qianquan MA1, Xiaoliang YIN1, Chenlong YANG1, Jia ZHANG1, Suhua CHEN1, Chao WU1, Jingcheng XIE1, Yunfeng HAN1, Guozhong LIN1, Yu SI1, Jun YANG1, Haibo WU3, Qiang ZHAO3
- 1. Department of Neurosurgery, Peking University Third Hospital, Beijing 100191, China
2. Department of Neurosurgery, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China
3. Department of Radiology, Peking University Third Hospital, Beijing 100191, China
摘要:
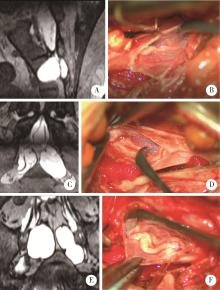
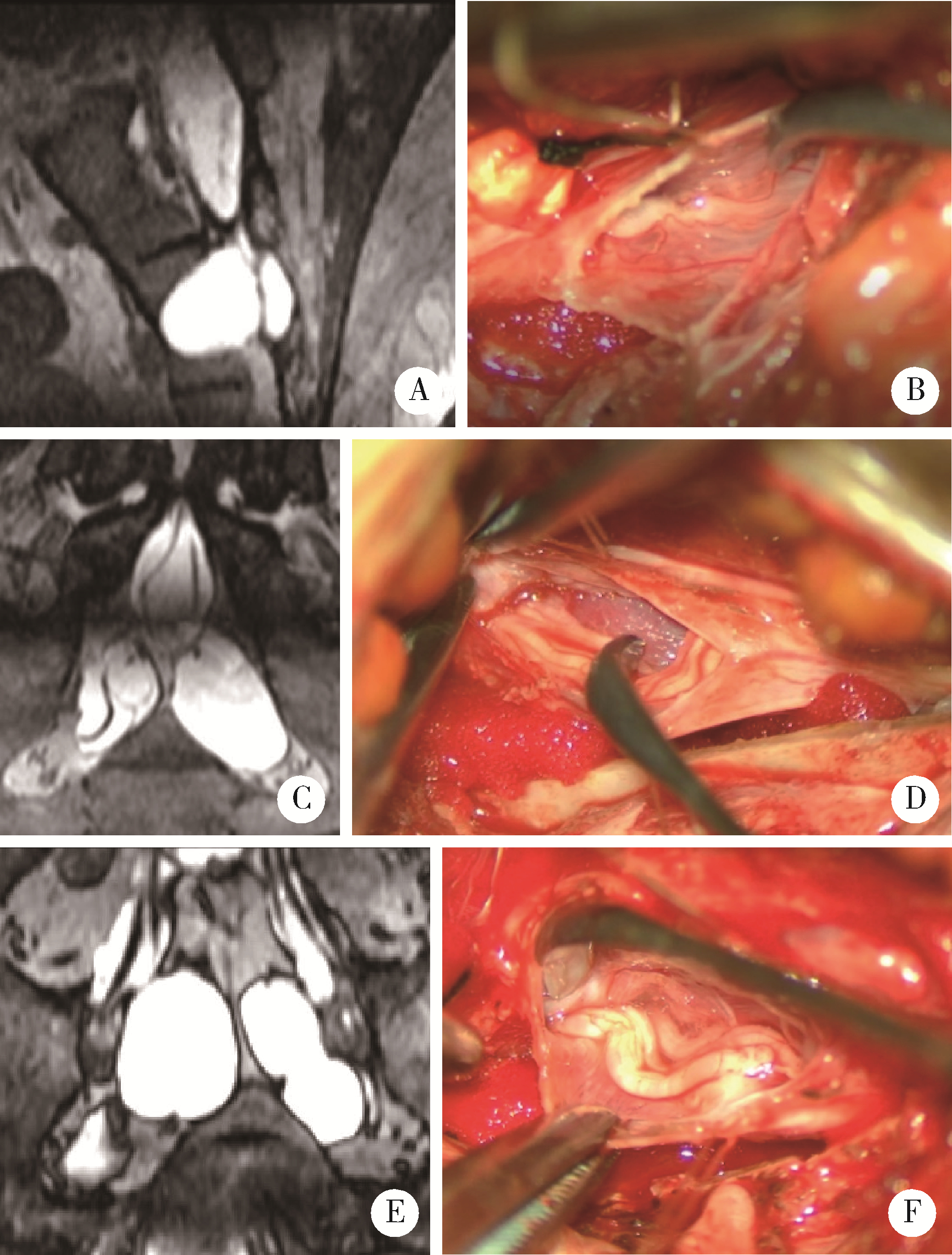
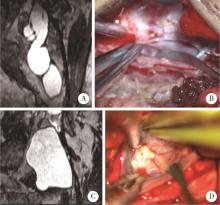
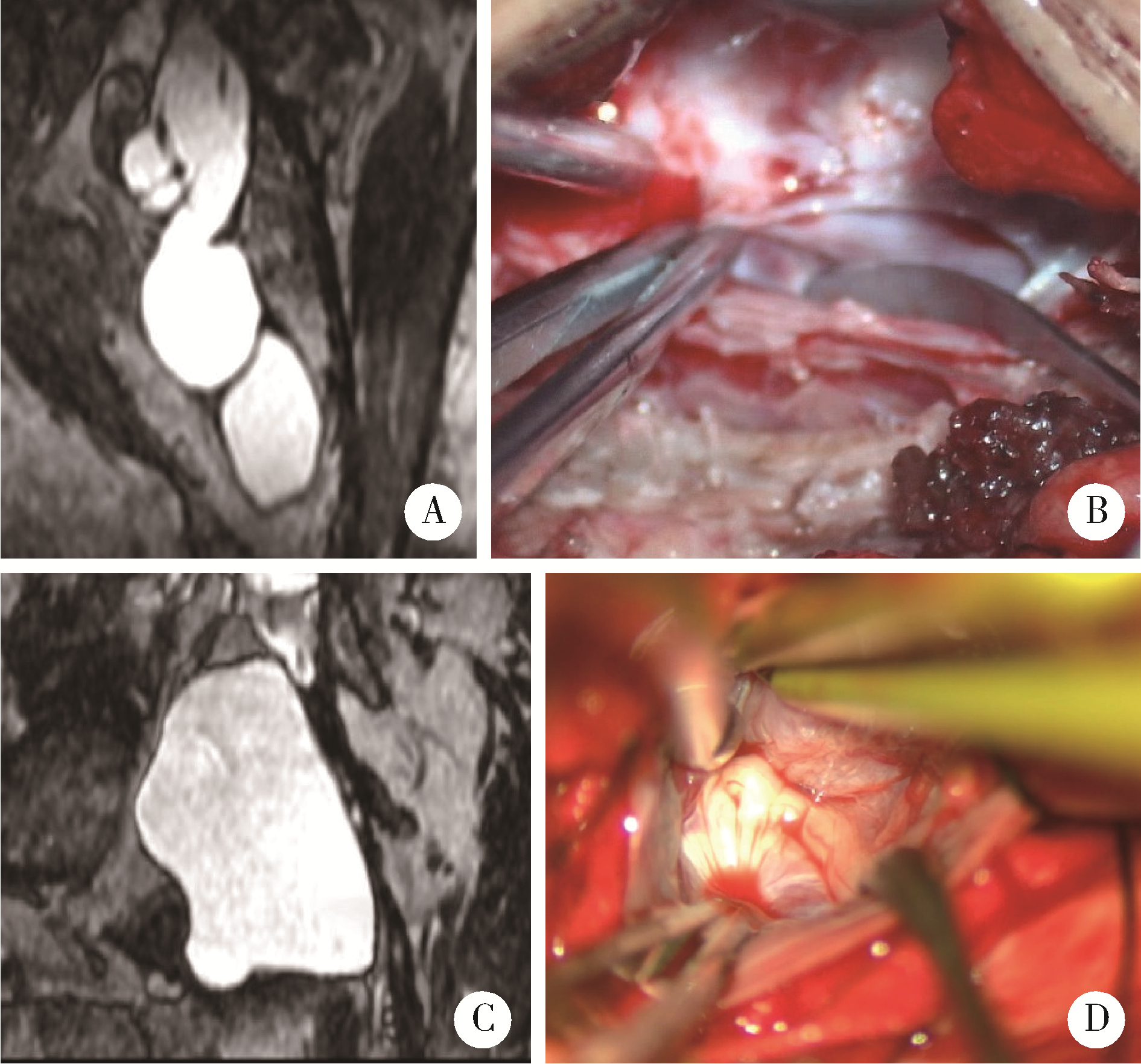
目的: 运用任意维度重建磁共振对骶管囊肿进行精准分型, 有效指导患者的微创手术和术后个性化康复。方法: 2021年3—12月, 应用任意维度重建磁共振评估骶管囊肿患者的围手术期状况, 根据神经根或漏口轨迹重建出囊肿内神经根走行和囊肿漏口情况, 对骶管囊肿进行精准分型并精准设计手术切口和骶管后壁骨窗范围。于显微镜下验证术前分型的准确性, 指导对应术式治疗不同类型的骶管囊肿。术后复查神经根水肿情况、术腔是否有积液等, 制定患者个性化的康复方案, 便于患者顺利康复。结果: 92例骶管囊肿患者中, 58例(63.0%)为内含神经根囊肿, 29例(31.5%)为内无神经根囊肿, 5例(5.4%)为混合型骶管囊肿。58例内含神经根囊肿的患者中, 手术显微镜下复核影像临床分型的准确度可达96.6% (56/58), 只有2例较大的单发囊肿、神经根在囊肿上极闪现被误认为内无神经根型。29例内无神经根的骶管囊肿患者中, 显微镜下复核影像的准确度达100%。对12例复发骶管囊肿内部的神经根和漏口情况的判断准确度达到100%。术后1个月发现迟发性术腔积液2例, 予以艾灸、泡澡等康复治疗, 患者术后4~6个月积液消失。结论: 任意维度重建磁共振在术前可准确判断骶管囊肿的临床分型, 指导手术精准执行, 并个性化改善患者的康复效果。
中图分类号:
- R739.42
| 1 |
Sun JJ , Wang ZY , Li ZD , et al. Reconstruction of nerve root sheaths for sacral extradural spinal meningeal cysts with spinal nerve root fibers[J]. Sci China Life Sci, 2013, 56 (11): 1007- 1013.
doi: 10.1007/s11427-013-4536-7 |
| 2 |
Sun JJ , Wang ZY , Teo M , et al. Comparative outcomes of the two types of sacral extradural spinal meningeal cysts using different operation methods: A prospective clinical study[J]. PLoS One, 2013, 8 (12): e83964.
doi: 10.1371/journal.pone.0083964 |
| 3 |
Sun JJ , Wang ZY , Liu B , et al. Neck transfixion for sacral extradural spinal meningeal cysts without spinal nerve root fibers[J]. Eur Spine J, 2016, 25 (6): 1945- 1952.
doi: 10.1007/s00586-014-3471-z |
| 4 | 谢京城, 王振宇, 陈晓东. 骶管终丝脊膜囊肿合并脊髓拴系综合征的诊断和治疗[J]. 中国临床神经外科杂志, 2015, 20 (11): 651- 653. |
| 5 |
Weigel R , Polemikos M , Uksul N , et al. Tarlov cysts: Long-term follow-up after microsurgical inverted plication and sacroplasty[J]. Eur Spine J, 2016, 25 (11): 3403- 3410.
doi: 10.1007/s00586-016-4744-5 |
| 6 | Hulens M , Bruyninckx F , Dankaerts W , et al. Electromyographic abnormalities associated with symptomatic sacral Tarlov cysts[J]. Pain Pract, 2016, 16 (5): E81- E88. |
| 7 |
Hulens M , Rasschaert R , Bruyninckx F , et al. Symptomatic Tarlov cysts are often overlooked: Ten reasons why: A narrative review[J]. Eur Spine J, 2019, 28 (10): 2237- 2248.
doi: 10.1007/s00586-019-05996-1 |
| 8 |
Fletcher SA , Mirza S , Burström G , et al. Management of perineural (Tarlov) cysts: A population-based cohort study and algorithm for the selection of surgical candidates[J]. Acta Neurochir (Wien), 2019, 161 (9): 1909- 1915.
doi: 10.1007/s00701-019-04000-5 |
| 9 |
Yang AI , Rinehart CD , McShane BJ , et al. Growth of lumbosacral perineural (Tarlov) cysts: A natural history analysis[J]. Neurosurgery, 2020, 86 (1): 88- 92.
doi: 10.1093/neuros/nyy586 |
| 10 |
Hulens M , Bruyninckx F , Dankaerts W , et al. High prevalence of perineural cysts in patients with fibromyalgia and chronic fatigue syndrome[J]. Pain Med, 2021, 22 (4): 883- 890.
doi: 10.1093/pm/pnaa410 |
| 11 |
Dowsett LE , Clement F , Coward S , et al. Effectiveness of surgical treatment for Tarlov cysts: A systematic review of published literature[J]. Clin Spine Surg, 2018, 31 (9): 377- 384.
doi: 10.1097/BSD.0000000000000582 |
| 12 | Telfeian AE , Doberstein C , Oyelese AA , et al. Transforaminal endoscopic approach for treatment of a lumbar perineural cyst: Technical note[J]. World Neurosurg, 2019, 127 (7): 85- 91. |
| 13 |
Wang Z , Jian F , Chen Z , et al. Percutaneous spinal endoscopic treatment of symptomatic sacral Tarlov cysts[J]. World Neurosurg, 2022, 158, e598- e604.
doi: 10.1016/j.wneu.2021.11.019 |
| 14 |
Ma QQ , Zhang J , Yang CL , et al. Arachnoidal diverticula of sacral extradural meningeal cyst: A novel definition and case series[J]. World Neurosurg, 2022, 163, e106- e112.
doi: 10.1016/j.wneu.2022.03.052 |
| 15 |
Tsuchimochi K , Morioka T , Murakami N , et al. Huge multiple spinal extradural meningeal cysts in infancy[J]. Childs Nerv Syst, 2019, 35 (3): 535- 540.
doi: 10.1007/s00381-018-4009-1 |
| 16 | 王奥楠, 邬海博, 孙建军. 三维快速稳态采集成像序列术前评估神经根型骶管囊肿的价值[J]. 实用放射学杂志, 2021, 37 (10): 15- 17. |
| [1] | 邢念增,王明帅,杨飞亚,尹路,韩苏军. 前列腺免活检创新理念的临床实践及其应用前景[J]. 北京大学学报(医学版), 2024, 56(4): 565-566. |
| [2] | 田宇轩,阮明健,刘毅,李德润,吴静云,沈棋,范宇,金杰. 双参数MRI改良PI-RADS评分4分和5分病灶的最大径对临床有意义前列腺癌的预测效果[J]. 北京大学学报(医学版), 2024, 56(4): 567-574. |
| [3] | 刘毅,袁昌巍,吴静云,沈棋,肖江喜,赵峥,王霄英,李学松,何志嵩,周利群. 靶向穿刺+6针系统穿刺对PI-RADS 5分患者的前列腺癌诊断效能[J]. 北京大学学报(医学版), 2023, 55(5): 812-817. |
| [4] | 袁昌巍,李德润,李志华,刘毅,山刚志,李学松,周利群. 多参数磁共振成像中动态对比增强状态在诊断PI-RADS 4分前列腺癌中的应用[J]. 北京大学学报(医学版), 2023, 55(5): 838-842. |
| [5] | 刘颖,霍然,徐慧敏,王筝,王涛,袁慧书. 磁共振血管壁成像评估颈动脉中重度狭窄患者斑块特征与脑血流灌注的相关性[J]. 北京大学学报(医学版), 2023, 55(4): 646-651. |
| [6] | 傅强,高冠英,徐雁,林卓华,孙由静,崔立刚. 无症状髋关节前上盂唇撕裂超声与磁共振检查的对比研究[J]. 北京大学学报(医学版), 2023, 55(4): 665-669. |
| [7] | 叶珊,金萍萍,张楠,邬海博,石林,赵强,杨坤,袁慧书,樊东升. 肌萎缩侧索硬化患者认知功能改变与脑皮层厚度分析[J]. 北京大学学报(医学版), 2022, 54(6): 1158-1162. |
| [8] | 蔡颖,万巧琴,蔡宪杰,高亚娟,韩鸿宾. 光生物调节加速脑组织间液引流及其机制[J]. 北京大学学报(医学版), 2022, 54(5): 1000-1005. |
| [9] | 王书磊,高阳旭,张宏武,杨海波,李辉,李宇,沈笠雪,姚红新. 儿童基底节区生殖细胞瘤30例临床分析[J]. 北京大学学报(医学版), 2022, 54(2): 222-226. |
| [10] | 张帆,陈曲,郝一昌,颜野,刘承,黄毅,马潞林. 术前及术后膜性尿道长度与腹腔镜根治性前列腺切除术后控尿功能恢复的相关性[J]. 北京大学学报(医学版), 2022, 54(2): 299-303. |
| [11] | 吴一凡,张晓圆,任爽,玉应香,常翠青. 基于磁共振的青年男性股四头肌的测量和评估[J]. 北京大学学报(医学版), 2021, 53(5): 843-849. |
| [12] | 盛荟,梁磊,周童亮,贾彦兴,王彤,袁兰,韩鸿宾. 光磁双模态探针钆-[4,7-双-羧甲基-10-(2-荧光素硫脲乙基)-1,4,7,10-四氮杂环十二烷-1-基]-乙酸络合物合成方法的改进[J]. 北京大学学报(医学版), 2020, 52(5): 959-963. |
| [13] | 赵世明,杨铁军,许春苗,郭孝峰,马永康,陈学军,李祥,何朝宏. 3.0T磁共振成像在接受过经尿道膀胱肿瘤切除术膀胱癌中诊断肌层浸润的应用[J]. 北京大学学报(医学版), 2020, 52(4): 701-704. |
| [14] | 林国中,王振宇,谢京城,刘彬,马长城,陈晓东. 内含终丝的骶管囊肿21例临床研究[J]. 北京大学学报(医学版), 2020, 52(3): 582-585. |
| [15] | 宋宇,韩鸿宾,杨军,王艾博,和清源,李媛媛,赵国梅,高亚娟,王睿,韩易兴,刘爱连,宋清伟. 脑对流增强给药对老年大鼠脑细胞外间隙微观结构的影响[J]. 北京大学学报(医学版), 2020, 52(2): 362-367. |
|
||