北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (2): 328-333. doi: 10.19723/j.issn.1671-167X.2025.02.017
良性前列腺增生患者排尿中断症状与尿动力学指标的相关性
- 北京积水潭医院泌尿外科,北京 100035
Correlation between urination intermittences and urodynamic parameters in benign prostatic hyperplasia patients
Ning LIU*( ), Libo MAN, Feng HE, Guanglin HUANG, Jianpo ZHAI
), Libo MAN, Feng HE, Guanglin HUANG, Jianpo ZHAI
- Department of Urology, Beijing Jishuitan Hospital, Beijing 100035, China
摘要:
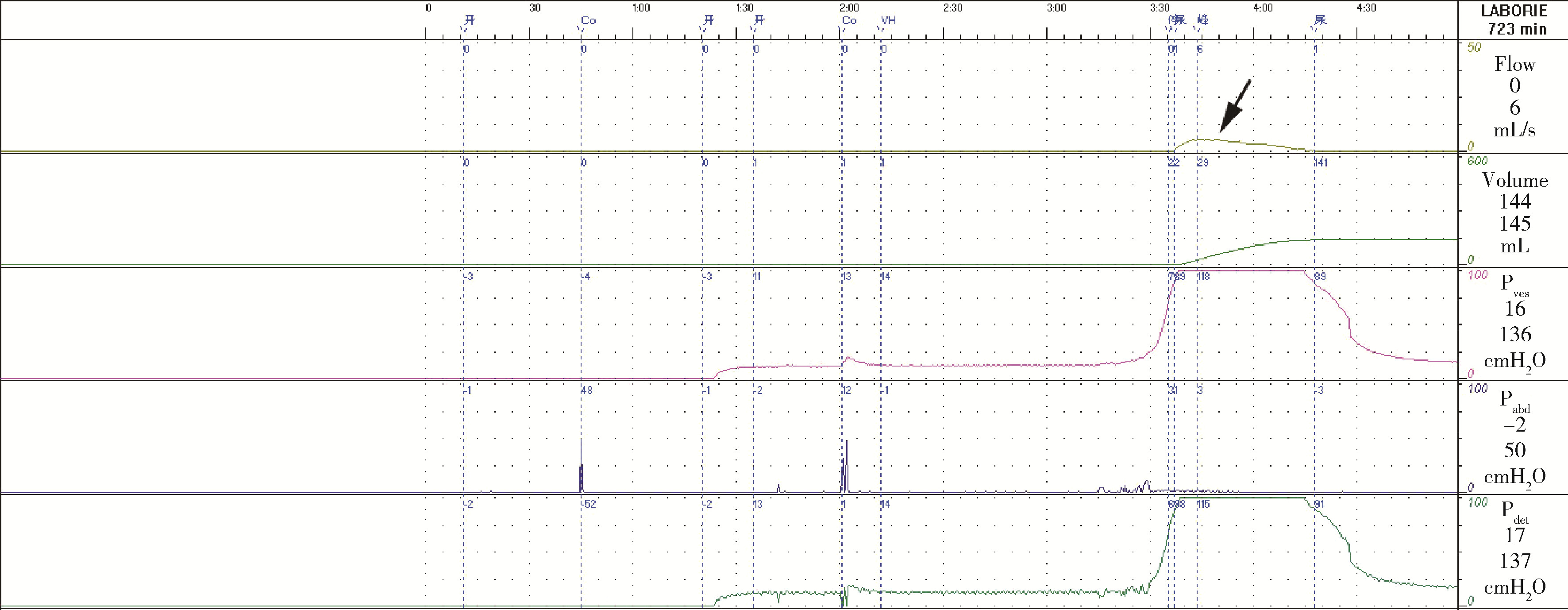
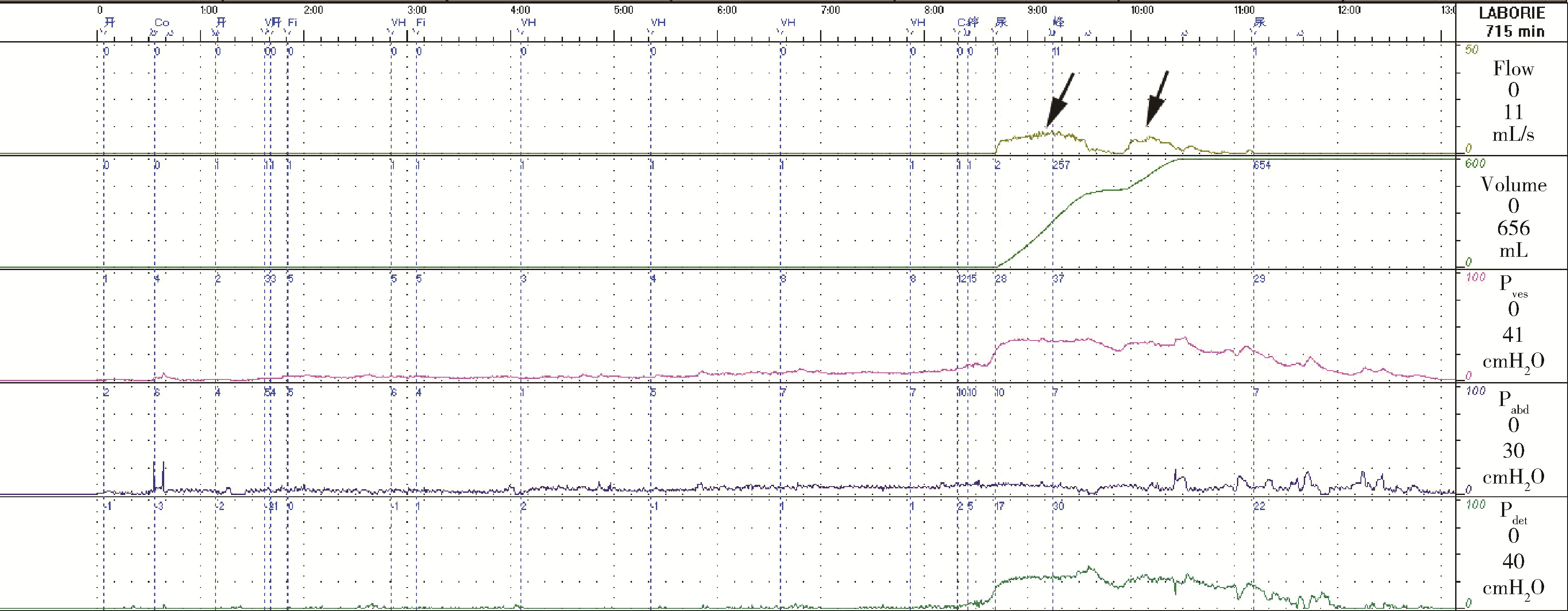
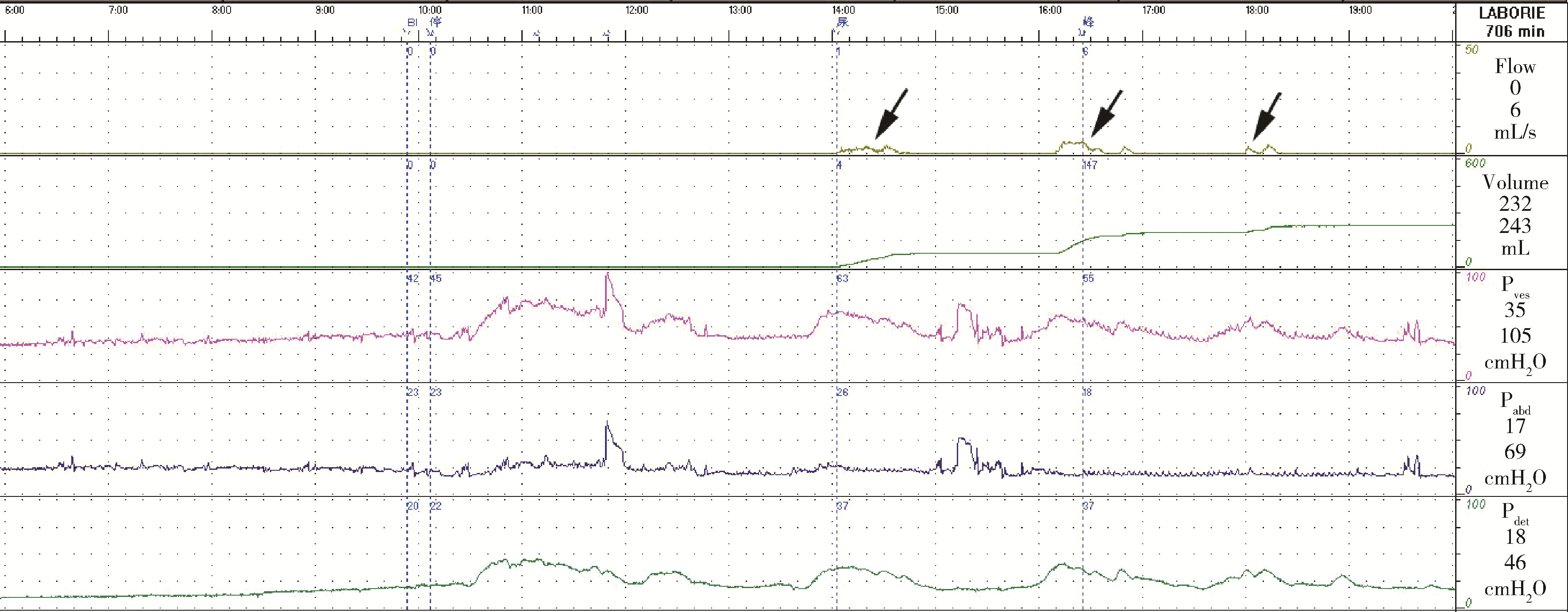
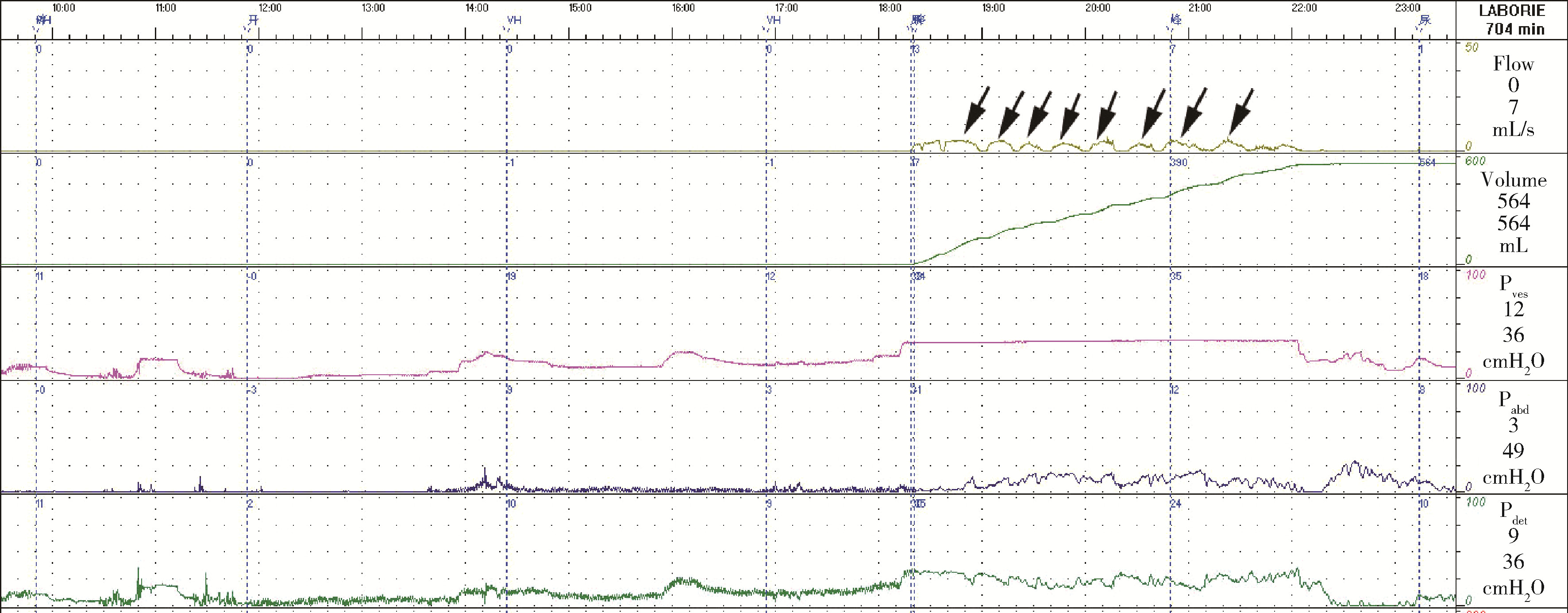
目的: 探讨良性前列腺增生(benign prostatic hyperplasia, BPH)患者排尿中断症状的影响因素和临床意义。方法: 对2016年1月至2021年6月期间272例男性BPH患者进行回顾性分析,患者均无神经系统病史及阳性体征,年龄45~84岁,平均63岁。全部患者先行自由尿流率检查,然后插管行尿动力学检查。应用逼尿肌功率曲线方法计算排尿做功、排尿功率和排尿能耗。根据自由尿流率的尿流中断频次进行分组,比较各组间的最大尿流时逼尿肌压(detrusor pressure at maximal flow rate,PdetQmax)、最大尿流率(maximal flow rate,Qmax)、膀胱收缩指数(bladder contractile index,BCI)、膀胱梗阻指数(bladder outlet obstruction index,BOOI)、排尿做功、排尿功率、排尿能耗等参数的差异。应用Logistic逐步回归方法分析发生排尿中断症状的影响因素。结果: 本组272例患者中,尿流无中断者179例(A组),尿流中断1次者46例(B组),尿流中断2次者22例(C组),尿流中断3次及以上者25例(D组)。各组的BCI为:A组113.4±28.2、B组101.0±30.2、C组83.3±30.2、D组81.0±30.5;排尿功率为:A组(29.2±14.8) mW、B组(16.4±9.6) mW、C组(14.5±7.1) mW、D组(8.5±5.0) mW,差异均有统计学意义(均P < 0.05)。各组的BOOI为:A组41.6±29.3、B组46.4±31.0、C组41.4±29.0、D组42.7±22.8;排尿能耗为:A组(5.41±2.21) J/L、B组(4.83±2.31) J/L、C组(5.02±2.54) J/L、D组(4.39±2.03) J/L,差异无统计学意义(均P>0.05)。Logistic逐步回归分析显示,膀胱功率(OR=0.814,95%CI:0.765~0.866,P < 0.001)、BCI (OR=1.023,95%CI:1.008~1.038,P=0.003)和膀胱做功(OR=2.232,95%CI:1.191~4.184,P=0.012)是发生排尿中断的独立危险因素。结论: BPH患者的排尿中断症状主要受到膀胱收缩功能的影响,与膀胱出口梗阻水平无明显关联,排尿中断频次增加可能是膀胱收缩功能下降的标志。
中图分类号:
- R697.32
| 1 |
Reynard JM , Yang Q , Donovan JL , et al. The ICS-"BPH" Study: Uroflowmetry, lower urinary tract symptoms and bladder outlet obstruction[J]. Br J Urol, 1998, 82 (5): 619- 623.
doi: 10.1046/j.1464-410x.1998.00813.x |
| 2 | Reddy SVK , Shaik AB . Non-invasive evaluation of bladder outlet obstruction in benign prostatic hyperplasia: A clinical correlation study[J]. J Urol, 2019, 17 (4): 259- 264. |
| 3 |
Hoag N , Gani J . Underactive bladder: Clinical features, urodynamic parameters, and treatment[J]. Int Neurourol J, 2015, 19 (3): 185- 189.
doi: 10.5213/inj.2015.19.3.185 |
| 4 |
Homma Y , Gotoh M , Kawauchi A , et al. Clinical guidelines for male lower urinary tract symptoms and benign prostatic hyperplasia[J]. Int J Urol, 2017, 24 (10): 716- 729.
doi: 10.1111/iju.13401 |
| 5 |
Parsons JK , Dahm P , Köhler TS , et al. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline amendment 2020[J]. J Urol, 2020, 204 (4): 799- 804.
doi: 10.1097/JU.0000000000001298 |
| 6 | Alexander LF , Oto A , Allen BC , et al. ACR Appropriateness Criteria® lower urinary tract symptoms: Suspicion of benign prostatic hyperplasia[J]. J Am Coll Radiol, 2019, 16 (11S): S378- S383. |
| 7 | Barry MJ , Fowler FJ Jr , O'Leary MP , et al. The American Urological Association symptom index for benign prostatic hyperplasia[J]. J Urol, 2017, 197 (2S): S189- S197. |
| 8 |
Li R , Zhu Q , Nibouche M , et al. Urine flow rate curve shapes and their descriptors[J]. Neurourol Urodyn, 2018, 37 (8): 2938- 2944.
doi: 10.1002/nau.23743 |
| 9 | Schäfer W . Analysis of bladder-outlet function with the linearized passive urethral resistance relation, linPURR, and a disease-specific approach for grading obstruction: From complex to simple[J]. World J Urol, 1995, 13 (1): 47- 58. |
| 10 | Drake MJ , Doumouchtsis SK , Hashim H , et al. Fundamentals of urodynamic practice, based on International Continence Society good urodynamic practices recommendations[J]. Neurourol Urodyn, 2018, 37 (S6): S50- S60. |
| 11 |
Rosier PFWM , Schaefer W , Lose G , et al. International Continence Society good urodynamic practices and terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study[J]. Neurourol Urodyn, 2017, 36 (5): 1243- 1260.
doi: 10.1002/nau.23124 |
| 12 |
Liu N , Man LB , He F , et al. Work capacity of the bladder during voiding: A novel method to evaluate bladder contractile function and bladder outlet obstruction[J]. Chin Med J (Engl), 2015, 128 (24): 3329- 3334.
doi: 10.4103/0366-6999.171426 |
| 13 | 刘宁, 满立波, 何峰, 等. 逼尿肌功率曲线分析在尿动力学研究中的应用[J]. 中华泌尿外科杂志, 2015, 36 (3): 224- 227. |
| 14 |
Smith PP , Birder LA , Abrams P , et al. Detrusor underactivity and the underactive bladder: Symptoms, function, cause-what do we mean? ICI-RS think tank 2014[J]. Neurourol Urodyn, 2016, 35 (2): 312- 317.
doi: 10.1002/nau.22807 |
| 15 |
Osman NI , Esperto F , Chapple CR . Detrusor underactivity and the underactive bladder: A systematic review of preclinical and clinical studies[J]. Eur Urol, 2018, 74 (5): 633- 643.
doi: 10.1016/j.eururo.2018.07.037 |
| 16 |
Chai TC , Kudze T . New therapeutic directions to treat underactive bladder[J]. Investig Clin Urol, 2017, 58 (Suppl 2): S99- S106.
doi: 10.4111/icu.2017.58.S2.S99 |
| 17 |
Gammie A , Kitney D , Drake M , et al. The calculation and comparison of the detrusor contractility parameter and Watts factor[J]. Neurourol Urodyn, 2018, 37 (8): 2745- 2752.
doi: 10.1002/nau.23745 |
| 18 |
Zhao Z , Azad R , Yang JH , et al. Progressive changes in detrusor function and micturition patterns with chronic bladder ischemia[J]. Investig Clin Urol, 2016, 57 (4): 249- 259.
doi: 10.4111/icu.2016.57.4.249 |
| 19 |
Namitome R , Takei M , Takahashi R , et al. A prediction model of detrusor underactivity based on symptoms and noninvasive test parameters in men with lower urinary tract symptoms: An analysis of a large group of patients undergoing pressure-flow studies[J]. Urol, 2020, 203 (4): 779- 785.
doi: 10.1097/JU.0000000000000616 |
| [1] | 柯涵炜, 王起, 许克新. 优化环磷酰胺剂量在间质性膀胱炎/膀胱疼痛综合征啮齿动物模型中的应用[J]. 北京大学学报(医学版), 2024, 56(5): 908-912. |
| [2] | 朱琳,张维宇,许克新. 环磷酰胺诱导SD大鼠膀胱疼痛综合征模型的有效性[J]. 北京大学学报(医学版), 2022, 54(4): 735-740. |
| [3] | 王起,张维宇,刘献辉,王明瑞,赖金惠,胡浩,徐涛,许克新. 骶神经调节术治疗膀胱逼尿肌无力的疗效分析[J]. 北京大学学报(医学版), 2021, 53(4): 671-674. |
| [4] | 王涛,许克新,张维宇,胡浩,张晓威,王焕瑞,刘献辉,陈京文,张晓鹏. 男性膀胱过度活动症的尿动力学分型及临床疗效随访[J]. 北京大学学报(医学版), 2019, 51(6): 1048-1051. |
| [5] | 刘可,张帆,肖春雷,夏海缀,郝一昌,毕海,赵磊,刘余庆,卢剑,马潞林. 低功率钬激光“七步两叶法”前列腺剜除术治疗良性前列腺增生[J]. 北京大学学报(医学版), 2019, 51(6): 1159-1164. |
| [6] | 张维宇,夏秋翔,胡浩,陈京文,孙屹然,许克新,张晓鹏. 门诊女性下尿路症状患者尿动力学检查结果分析及逼尿肌无力患者的随访[J]. 北京大学学报(医学版), 2019, 51(5): 856-862. |
| [7] | 张维宇,张晓鹏,陈京文,孙屹然,王佳,胡浩,许克新. 年龄因素对女性尿失禁患者尿动力学参数的影响[J]. 北京大学学报(医学版), 2016, 48(5): 825-829. |
| [8] | 张维宇,胡浩,王起,陈京文,许克新. 女性压力性尿失禁患者术前尿动力学检查的意义[J]. 北京大学学报(医学版), 2016, 48(4): 655-658. |
| [9] | 刘宁, 黄广林, 满立波, 何峰, 王海东, 王海, 李贵忠, 王建伟. 缩短钬激光前列腺剜除术学习曲线的方法[J]. 北京大学学报(医学版), 2015, 47(4): 720-723. |
| [10] | 刘宁, 何峰, 满立波, 黄广林, 王海东, 王海, 李贵忠, 王建伟. 尿动力学检查中伪像的曲线特征及影响因素分析[J]. 北京大学学报(医学版), 2014, 46(5): 817-820. |
| [11] | 靖华芳, 廖利民, 付光, 吴娟, 鞠彦合, 陈国庆. 脊髓损伤患者上尿路功能损害的相关因素分析[J]. 北京大学学报(医学版), 2014, 46(4): 544-547. |
| [12] | 胡浩, 许克新, 张晓鹏, 方志伟, 陈京文, 霍飞, 王栋, 王晓峰. 伴有膀胱过度活动症症状的良性前列腺增生患者尿液中脑源性神经营养因子的表达[J]. 北京大学学报(医学版), 2014, 46(4): 519-523. |
| [13] | 张峰波, 邵强, 田野. 二极管激光与铥激光经尿道前列腺剜除术治疗良性前列腺增生的应用比较[J]. 北京大学学报(医学版), 2013, 45(4): 592-. |
| [14] | 邓小林, 张虎, 史本涛, 关志忱. 家庭尿流率测定在下尿路症状患者评估中的研究进展[J]. 北京大学学报(医学版), 2012, 44(4): 655-658. |
| [15] | 金哲, 辛钟成 . 阴茎勃起功能障碍合并良性前列腺增生症相关下尿路症状的治疗[J]. 北京大学学报(医学版), 2011, 43(4): 632-635. |
|
||