北京大学学报(医学版) ›› 2018, Vol. 50 ›› Issue (6): 1078-1082. doi: 10.19723/j.issn.1671-167X.2018.06.024
鼻喷右美托咪定在儿童口腔门诊全身麻醉前的镇静效果
- 北京大学口腔医学院·口腔医院,麻醉科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室, 北京 100081
Effects of intranasal dexmedetomidine for children undergoing dental rehabilitation under general anesthesia: a double-blinded randomized controlled trial
Ling GAO( ),Yun LIU,Xu-dong YANG
),Yun LIU,Xu-dong YANG
- Department of Anesthesiology, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
摘要:
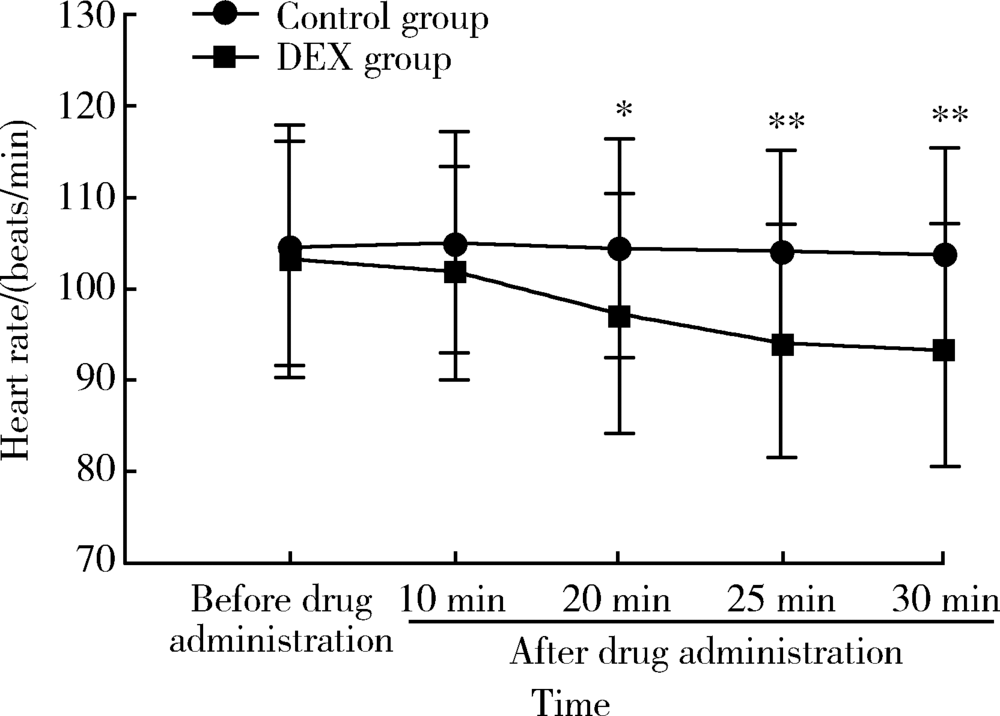
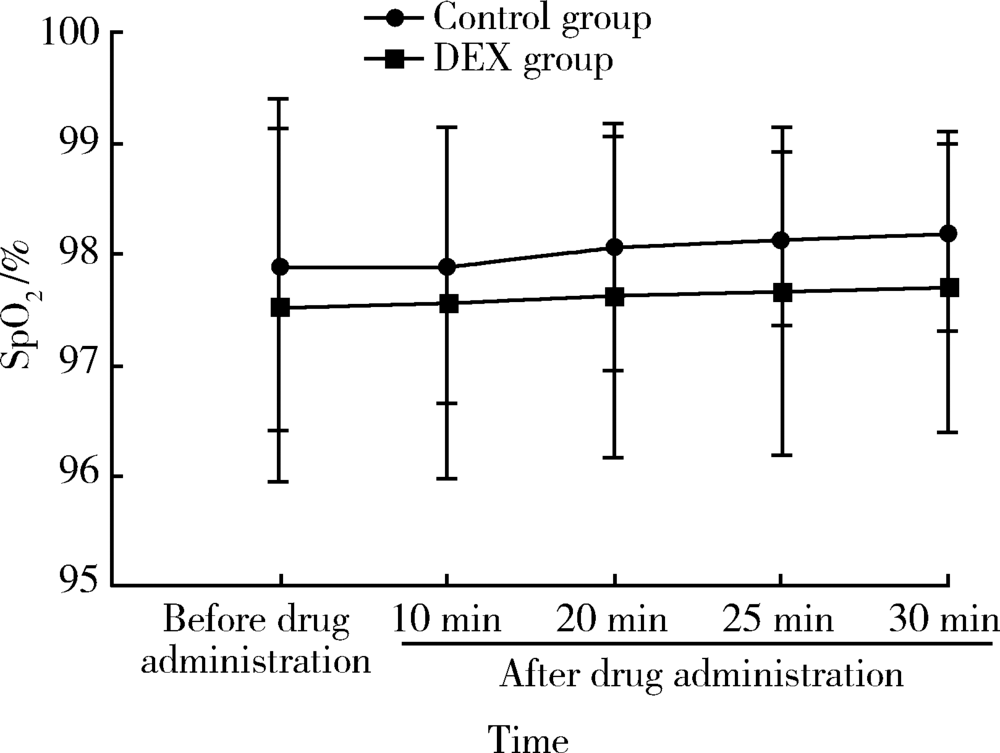
目的: 观察全身麻醉下牙病治疗患儿鼻喷右美托咪定(dexmedetomidine,DEX)对术前紧张情绪、父母分离焦虑、面罩接受程度和术后躁动的影响。方法: 选择北京大学口腔医院儿童口腔门诊全身麻醉下牙病治疗的患儿60例,年龄2~9岁,随机分为2组:对照组术前30 min经鼻喷入生理盐水0.02 mL/kg,DEX组喷入DEX 2 μg/kg(药物使用原液)。观察和记录患儿给药前及给药后10、20、25、30 min的心率(heart rate,HR)、脉搏血氧饱和度(oxygen saturation,SpO2)以及给药30 min后的Ramsay镇静评分、分离焦虑评分、面罩吸入诱导接受度评分和术后躁动评分及并发症的情况。结果: 两组患儿的年龄、体重、性别构成、手术时间、拔管时间和苏醒时间相似,差异无统计学意义。DEX组患儿与父母的分离焦虑、面罩接受程度明显优于对照组(56.7% vs. 26.7%,73.3% vs. 40%,P均<0.05),术后躁动评分在两组间差异无统计学意义(P>0.05)。与对照组相比,DEX组患儿给药20 min后HR有所下降,差异有统计学意义[(97.13±12.93)次/min vs. (104.53±11.97)次/min, P<0.05]。两组患儿的SpO2未见明显差异,且均未见心动过缓、低氧血症的发生。结论: 全身麻醉前经鼻喷入DEX可以产生良好的术前镇静作用,改善与父母的分离焦虑,提高面罩接受度。两组患儿苏醒质量高,无明显的苏醒期躁动、呼吸抑制等并发症。鼻喷DEX 2 μg/kg是一种安全有效的儿童术前给药方式。
中图分类号:
- R782.05
| [1] |
夏斌, 秦满, 马文利 , 等. 693例儿童全身麻醉下牙齿治疗的特征分析[J]. 北京大学学报(医学版), 2013,45(6):984-988.
doi: 10.3969/j.issn.1671-167X.2013.06.032 |
| [2] |
Kain ZN, Mayes LC , O’Connor TZ, et al. Preoperative anxiety in children. Predictors and outcomes[J]. Arch Pediatr Adolesc Med, 1996,150(12):1238-1245.
doi: 10.1001/archpedi.1996.02170370016002 |
| [3] |
Wstson AT, Visram A . Children’s preoperative anxiety and postoperative behavior[J]. Paediatr Anaesth, 2003,13(3):188-204.
doi: 10.1046/j.1460-9592.2003.00848.x pmid: 12641680 |
| [4] |
Wolfe TR, Braude DA . Intranasl medication delivery for children: A brief review and update[J]. Pediatrics, 2010,126(3):532-537.
doi: 10.1542/peds.2010-0616 pmid: 20696726 |
| [5] |
Peng K, Wu SR, Ji FH , et al. Premedication with dexmedetomidine in pediatric patients: a systematic review and meta-analysis[J]. Clinics, 2014,69(11):777-786.
doi: 10.6061/clinics/2014(11)12 pmid: 4255070 |
| [6] |
Piao G, Wu J . Systematic assessment of dexmedetomidine as an anesthetic agent: a meta-analysis of randomized controlled trials[J]. Arch Med Sci, 2014,10(1):19-24.
doi: 10.5114/aoms.2014.40730 pmid: 3953974 |
| [7] |
Kuang H, Johnson JA, Mulqueen JM , et al. The efficacy of benzodiazepines as acute anxiolytics in children: A meta-analysis[J]. Depress Anxiety, 2017,34(10):888-896.
doi: 10.1002/da.22643 pmid: 28504861 |
| [8] |
Deshmukh PV, Kulkami SS, Parchandekar MK , et al. Comparison of preanesthetic sedation in pediatric patients with oral and intranasal midazolam[J]. J Anaesthesiol Clin Pharmacol, 2016,32(3):353-358.
doi: 10.4103/0970-9185.168205 pmid: 5009843 |
| [9] |
Iirola T, Vilo S, Manner T , et al. Bioavailability of dexmedetomidine after intranasal administration[J]. Eur J Clin Pharmacol, 2011,67(8):825-831.
doi: 10.1007/s00228-011-1002-y |
| [10] |
Lee Y, Kim J, Kim S , et al. Intranasal administration of dexmedetomidine (DEX) as a premedication for pediatric patients undergoing general anesthesia for dental treatment[J]. J Dent Anesth Pain Med, 2016,16(1):25-29.
doi: 10.17245/jdapm.2016.16.1.25 pmid: 5564115 |
| [11] |
Sheta SA, Al-Sarheed MA, Abdelhalim AA . Intranasal dexmedetomidine vs. midazolam for premedication in children undergoing complete dental rehabilitation: a double-blinded randomized controlled trial[J]. Pediatric Anesth, 2014,24(2):181-189.
doi: 10.1111/pan.12287 pmid: 24237879 |
| [12] |
Yuen VM, Irwin MG, Hui TW , et al. A double-blind, crossover assessment of the sedative and analgesic effects of intranasal dexmedetomidine[J]. Anesth Analg, 2007,105(2):374-380.
doi: 10.1213/01.ane.0000269488.06546.7c pmid: 17646493 |
| [13] |
Yuen VM, Hui TW, Irwin MG , et al. Optimal timing for the administration of intranasal dexmedetomidine for premedication in children[J]. Anaesthesia, 2010,65(9):922-929.
doi: 10.1111/j.1365-2044.2010.06453.x |
| [14] |
Yuen VM, Hui TW, Irwin MG , et al. A randomised comparison of two intranasal dexmedetomidine doses for premedication in children[J]. Anaesthesia, 2012,67(11):1210-1216.
doi: 10.1111/j.1365-2044.2012.07309.x pmid: 22950484 |
| [15] |
Yuen VM, Hui TW, Irwin MG , et al. A comparison of intranasal dexmedetomidine and oral midazolam for premedication in pediatric anesthesia: a double-blinded randomized controlled trial[J]. Anesth Analg, 2008,106(6):1715-1721.
doi: 10.1213/ane.0b013e31816c8929 pmid: 18499600 |
| [16] |
Wolfe TR, Bemstone T . Intranasal drug delivery: An alternative to intravenous administration in selected emergency cases[J]. J Emerg Nurs, 2004,30(2):141-147.
doi: 10.1016/j.jen.2004.01.006 |
| [17] |
Talon MD, Woodson LC, Sherwood ER , et al. Intranasal dexmedetomidine premedication is comparable with midazolam in burn children undergoing reconstructive surgery[J]. J Burn Care Res, 2009,30(4):599-605.
doi: 10.1097/BCR.0b013e3181abff90 pmid: 19506498 |
| [18] |
Jun JH, Kim KN, Kim JY , et al. The effects of intranasal dexmedetomidine premedication in children: a systematic review and meta-analysis[J]. Can J Anaesth, 2017,64(9):947-961.
doi: 10.1007/s12630-017-0917-x pmid: 28639236 |
| [19] |
Kain ZN, Caldwell-Andrews AA, Maranets I , et al. Predicting which child-parent pair will benefit from parental presence during induction of anesthesia: A decision-making approach[J]. Anesth Analg, 2006,102(1):81-84.
doi: 10.1213/01.ANE.0000181100.27931.A1 pmid: 16368808 |
| [1] | 赵双云, 邹思雨, 李雪莹, 沈丽娟, 周虹. 中文版口腔健康素养量表简版(HeLD-14)在学龄前儿童家长中应用的信度和效度评价[J]. 北京大学学报(医学版), 2024, 56(5): 828-832. |
| [2] | 陈心心, 唐哲, 乔艳春, 荣文笙. 北京市密云区4岁儿童患龋状况及其与龋活跃性检测的相关性[J]. 北京大学学报(医学版), 2024, 56(5): 833-838. |
| [3] | 岳芷涵,韩娜,鲍筝,吕瑾莨,周天一,计岳龙,王辉,刘珏,王海俊. 儿童早期体重指数轨迹与超重风险关联的前瞻性队列研究[J]. 北京大学学报(医学版), 2024, 56(3): 390-396. |
| [4] | 费秀文,刘斯,汪波,董爱梅. 成人及儿童组织坏死性淋巴结炎临床特征及治疗[J]. 北京大学学报(医学版), 2024, 56(3): 533-540. |
| [5] | 俞光岩. 儿童唾液腺疾病[J]. 北京大学学报(医学版), 2024, 56(1): 1-3. |
| [6] | 闫晓晋,刘云飞,马宁,党佳佳,张京舒,钟盼亮,胡佩瑾,宋逸,马军. 《中国儿童发展纲要(2011-2020年)》实施期间中小学生营养不良率变化及其政策效应分析[J]. 北京大学学报(医学版), 2023, 55(4): 593-599. |
| [7] | 弭小艺,侯杉杉,付子苑,周末,李昕璇,孟召学,蒋华芳,周虹. 中文版童年不良经历问卷在学龄前儿童父母中应用的信效度评价[J]. 北京大学学报(医学版), 2023, 55(3): 408-414. |
| [8] | 崔孟杰,马奇,陈曼曼,马涛,王鑫鑫,刘婕妤,张奕,陈力,蒋家诺,袁雯,郭桐君,董彦会,马军,星一. 不同生长模式与7~17岁儿童青少年代谢综合征的关系[J]. 北京大学学报(医学版), 2023, 55(3): 415-420. |
| [9] | 党佳佳,蔡珊,钟盼亮,王雅琪,刘云飞,师嫡,陈子玥,张依航,胡佩瑾,李晶,马军,宋逸. 室外夜间人工光暴露与中国9~18岁儿童青少年超重肥胖的关联[J]. 北京大学学报(医学版), 2023, 55(3): 421-428. |
| [10] | 陈敬,肖伍才,单蕊,宋洁云,刘峥. DRD2基因rs2587552多态性对儿童肥胖干预效果的影响:一项前瞻性、平行对照试验[J]. 北京大学学报(医学版), 2023, 55(3): 436-441. |
| [11] | 李辉,高阳旭,王书磊,姚红新. 恶性肿瘤患儿完全植入式静脉输液港手术并发症[J]. 北京大学学报(医学版), 2022, 54(6): 1167-1171. |
| [12] | 刘京,陆爱东,左英熹,吴珺,黄志卓,贾月萍,丁明明,张乐萍,秦炯. 儿童急性淋巴细胞白血病合并癫痫发作75例临床特征和预后分析[J]. 北京大学学报(医学版), 2022, 54(5): 948-953. |
| [13] | 崔雅茜,杜军保,张清友,廖莹,刘平,王瑜丽,齐建光,闫辉,徐文瑞,刘雪芹,孙燕,孙楚凡,张春雨,陈永红,金红芳. 儿童直立不耐受和坐位不耐受的疾病谱及治疗方式十年回顾[J]. 北京大学学报(医学版), 2022, 54(5): 954-960. |
| [14] | 马涛,李艳辉,陈曼曼,马莹,高迪,陈力,马奇,张奕,刘婕妤,王鑫鑫,董彦会,马军. 青春期启动提前与儿童肥胖类型的关联研究: 基于横断面调查和队列调查[J]. 北京大学学报(医学版), 2022, 54(5): 961-970. |
| [15] | 杜燕燕,王健,贺兰,季丽娜,徐樨巍. 儿童川崎病合并轻微脑炎/脑病伴可逆性胼胝体压部病变综合征1例并文献复习[J]. 北京大学学报(医学版), 2022, 54(4): 756-761. |
|
||