北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (3): 492-499. doi: 10.19723/j.issn.1671-167X.2020.03.015
大气臭氧短期监测指标与健康年轻人肺功能和气道炎症的关联
- 北京大学公共卫生学院劳动卫生与环境卫生学系,北京 100191
Monitoring metrics for short-term exposure to ambient ozone and pulmonary function and airway inflammation in healthy young adults
Jia-hui CHEN,Da-yu HU,Xu JIA,Wei NIU,Fu-rong DENG,Xin-biao GUO( )
)
- Department of Occupational and Environmental Health Sciences, Peking University School of Public Health, Beijing 100191, China
摘要:
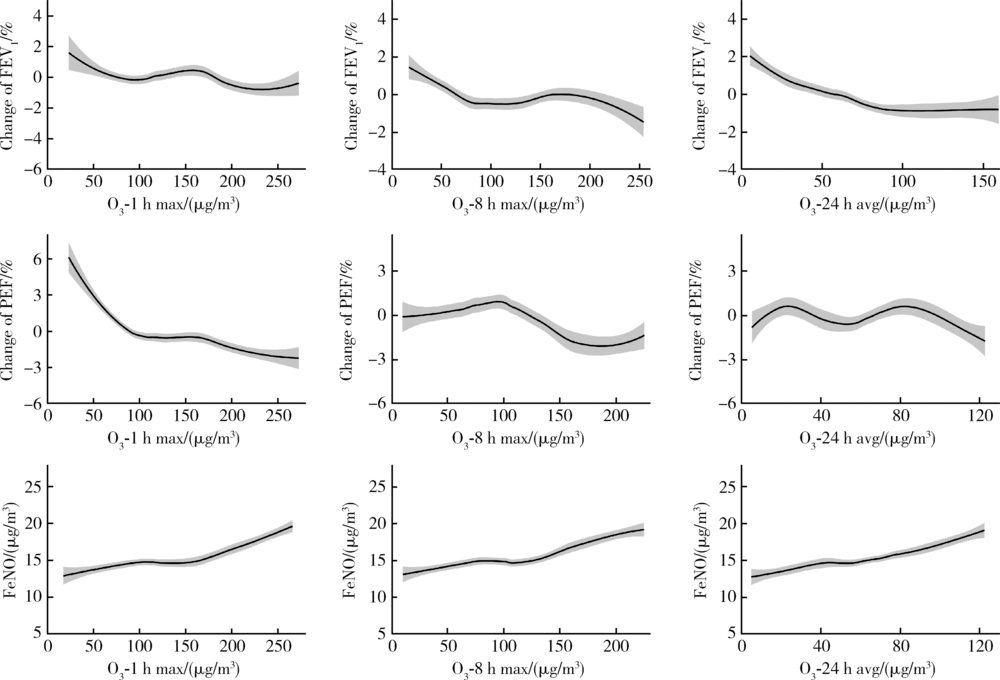
目的 探讨不同监测指标下,大气臭氧(ozone,O3)短期暴露与健康年轻人肺功能和气道炎症的关联。方法 采用定组研究设计,招募97名健康年轻大学生为研究对象,于2017年12月至2018年6月对每位研究对象进行3次随访调查,每次随访期间对研究对象的肺功能和呼出气一氧化氮(fractional exhaled nitric oxide,FeNO)进行测量;空气污染物浓度数据由距研究对象居住区最近的北京市环境监测站获得,气象数据来自中国气象数据网。采用线性混合效应模型分析不同监测指标下,大气O3短期暴露与健康年轻人肺功能和气道炎症的关联。结果 研究期间大气O3日1 h最大浓度(daily 1-h maximum concentration of O3,O3-1 h max)、日最大8 h平均浓度(daily maximum 8-h average concentration of O3,O3-8 h max)和24 h平均浓度(24-h average concentration of O3,O3-24 h avg)的P50(P25,P75)分别为102.5(76.8,163.0) μg/m3、91.1(68.3,154.3) μg/m3和61.6(36.9,81.7) μg/m3。效应估计结果显示,不同监测指标下,大气O3与第1秒用力呼气容积(forced expiratory volume in the first second,FEV1)呈显著负相关,与FeNO呈显著正相关。O3-1 h max的6 d滑动平均值每增加一个四分位数间距(interquartile range,IQR=71.5 μg/m3)与FEV1降低 6.2%(95%CI: -11.8%,-0.5%)和FeNO升高63.3%(95%CI: 13.8%,134.3%)有关。O3-8 h max的7 d滑动平均值每增加一个四分位数间距(IQR=62.0 μg/m3)与FEV1降低6.2%(95%CI: -11.6%,-0.7%)和FeNO升高75.5%(95%CI: 19.3,158.0%)有关。O3-24 h avg的5 d滑动平均值每增加一个四分位数间距(IQR=32.9 μg/m3)与FEV1降低3.7%(95%CI: -7.1%,-0.2%)和FeNO升高25.3%(95%CI: 3.6%,51.6%)有关。没有观察到不同监测指标下O3与最大呼气流量(peak expiratory flow,PEF)变化的显著关联。 结论 大气O3的短期暴露与健康年轻人的肺功能降低和气道炎症增加有关,且日1 h最大浓度指标更能灵敏反映O3的呼吸效应。
中图分类号:
- X5
| [1] |
Dales R, Chen L, Frescura AM, et al. Acute effects of outdoor air pollution on forced expiratory volume in 1 s: a panel study of schoolchildren with asthma[J]. Eur Respir J, 2009,34(2):316-323.
doi: 10.1183/09031936.00138908 |
| [2] | 邸沂遥. 空气污染对哮喘患者肺功能、FeNO和血清IgE水平的影响[D]. 石家庄: 河北医科大学, 2016. |
| [3] |
Sinharay R, Gong J, Barratt B, et al. Respiratory and cardiovascular responses to walking down a traffic-polluted road compared with walking in a traffic-free area in participants aged 60 years and older with chronic lung or heart disease and age-matched healthy controls: a randomised, crossover study[J]. Lancet, 2018,391(10118):339-349.
doi: 10.1016/S0140-6736(17)32643-0 pmid: 29221643 |
| [4] |
Yoda Y, Otani N, Sakurai S, et al. Acute effects of summer air pollution on pulmonary function and airway inflammation in healthy young women[J]. J Epidemiol, 2014,24(4):312-320.
pmid: 24857953 |
| [5] |
Bai L, Su X, Zhao D, et al. Exposure to traffic-related air pollution and acute bronchitis in children: season and age as modifiers[J]. J Epidemiol Community Health, 2018,72(5):426-433.
pmid: 29440305 |
| [6] |
Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015[J]. Lancet, 2017,389(10082):1907-1918.
doi: 10.1016/S0140-6736(17)30505-6 pmid: 28408086 |
| [7] | 崔娟, 王黎君. 1990年与2013年中国大气臭氧污染导致慢性阻塞性肺疾病的疾病负担分析[J]. 中华预防医学杂志, 2016,50(5):391-396. |
| [8] |
Guo Y, Zeng H, Zheng R, et al. The association between lung cancer incidence and ambient air pollution in China: a spatiotemporal analysis[J]. Environ Res, 2016,144(Pt A):60-65.
pmid: 26562043 |
| [9] |
Yang C, Yang H, Guo S, et al. Alternative ozone metrics and daily mortality in Suzhou: the China air pollution and health effects study (CAPES)[J]. Sci Total Environ, 2012,426:83-89.
doi: 10.1016/j.scitotenv.2012.03.036 pmid: 22521098 |
| [10] | Tolbert PE, Klein M, Metzger KB, et al. Interim results of the study of particulates and health in Atlanta (SOPHIA)[J]. J Expo Anal Environ Epidemiol, 2000,10(5):446-460. |
| [11] |
Li H, Wu S, Pan L, et al. Short-term effects of various ozone metrics on cardiopulmonary function in chronic obstructive pulmonary disease patients: results from a panel study in Beijing, China[J]. Environ Pollut, 2018,232:358-366.
doi: 10.1016/j.envpol.2017.09.030 pmid: 28987568 |
| [12] |
Bell ML, Dominici F, Samet JM. A meta-analysis of time-series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study[J]. Epidemiology, 2005,16(4):436-445.
doi: 10.1097/01.ede.0000165817.40152.85 pmid: 15951661 |
| [13] |
Thurston GD, Ito K. Epidemiological studies of acute ozone exposures and mortality[J]. J Expo Anal Environ Epidemiol, 2001,11(4):286-294.
pmid: 11571608 |
| [14] |
Anderson GB, Bell ML. Does one size fit all? The suitability of standard ozone exposure metric conversion ratios and implications for epidemiology[J]. J Expo Sci Environ Epidemiol, 2010,20(1):2-11.
doi: 10.1038/jes.2008.69 pmid: 18985076 |
| [15] |
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry[J]. Eur Respir J, 2005,26(2):319-338.
doi: 10.1183/09031936.05.00034805 pmid: 16055882 |
| [16] |
ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005[J]. Am J Respir Crit Care Med, 2005,171(8):912-930.
doi: 10.1164/rccm.200406-710ST pmid: 15817806 |
| [17] | 王亭槐. 生理学[M]. 9版. 北京: 人民卫生出版社, 2018: 156. |
| [18] |
Adman MA, Hashim JH, Manaf MRA, et al. Associations between air pollutants and peak expiratory flow and fractional exhaled nitric oxide in students[J]. Int J Tuberc Lung Dis, 2020,24(2):189-195.
doi: 10.5588/ijtld.19.0096 pmid: 32127103 |
| [19] | 杨克敌. 环境卫生学[M]. 8版. 北京: 人民卫生出版社, 2017: 95. |
| [20] |
Huang J, Song Y, Chu M, et al. Cardiorespiratory responses to low-level ozone exposure: the in door ozone study in children (DOSE)[J]. Environ Int, 2019,131:105021.
pmid: 31349208 |
| [21] |
Altug H, Gaga EO, Dogeroglu T, et al. Effects of ambient air pollution on respiratory tract complaints and airway inflammation in primary school children[J]. Sci Total Environ, 2014,479/480:201-209.
doi: 10.1016/j.scitotenv.2014.01.127 |
| [22] | 张嘉尧. 臭氧对人群的急性健康影响研究[D]. 南京: 南京医科大学, 2019. |
| [23] |
Zhang J, Sun H, Chen Q, et al. Effects of individual ozone exposure on lung function in the elderly: a cross-sectional study in China[J]. Environ Sci Pollut Res Int, 2019,26(12):11690-11695.
doi: 10.1007/s11356-019-04324-w pmid: 30806931 |
| [24] |
Devlin RB, Duncan KE, Jardim M, et al. Controlled exposure of healthy young volunteers to ozone causes cardiovascular effects[J]. Circulation, 2012,126(1):104-111.
doi: 10.1161/CIRCULATIONAHA.112.094359 pmid: 22732313 |
| [25] |
Kariisa M, Foraker R, Pennell M, et al. Short- and long-term effects of ambient ozone and fine particulate matter on the respiratory health of chronic obstructive pulmonary disease subjects[J]. Arch Environ Occup Health, 2015,70(1):56-62.
doi: 10.1080/19338244.2014.932753 pmid: 25136856 |
| [26] | 赵丽敏, 马利军. 呼出气一氧化氮检测及临床意义[J]. 中华实用诊断与治疗杂志, 2011,25(5):422-423. |
| [27] |
Nickmilder M, de Burbure C, Carbonnelle S, et al. Increase of exhaled nitric oxide in children exposed to low levels of ambient ozone[J]. J Toxicol Environ Health A, 2007,70(3-4):270-274.
doi: 10.1080/15287390600884834 pmid: 17365589 |
| [28] |
Berhane K, Zhang Y, Linn WS, et al. The effect of ambient air pollution on exhaled nitric oxide in the children’s health study[J]. Eur Respir J, 2011,37(5):1029-1036.
doi: 10.1183/09031936.00081410 pmid: 20947676 |
| [29] |
Day DB, Xiang J, Mo J, et al. Association of ozone exposure with cardiorespiratory pathophysiologic mechanisms in healthy adults[J]. JAMA Intern Med, 2017,177(9):1344-1353.
doi: 10.1001/jamainternmed.2017.2842 pmid: 28715576 |
| [30] |
Bell ML, Hobbs BF, Ellis H. Metrics matter: conflicting air quality rankings from different indices of air pollution[J]. J Air Waste Manag Assoc, 2005,55(1):97-106.
doi: 10.1080/10473289.2005.10464596 pmid: 15704544 |
| [1] | 阎腾龙,胥嘉钰,陈田,杨鑫,王伟伟,周淑佩,牛丕业,贾光,夏交. 亚慢性PM2.5和O3共同暴露对大鼠鼻黏膜ATP总量及ATP酶活性的影响[J]. 北京大学学报(医学版), 2024, 56(4): 687-692. |
| [2] | 张宏,董继元,王建军,范临夏,曲强,刘洋. 兰州市臭氧对儿童哮喘的短期影响及其季节性差异[J]. 北京大学学报(医学版), 2022, 54(2): 227-235. |
| [3] | 刘佳兴,胡贵平,赵琳,张永明,王丽,贾光,刘瑞祥,冯慧敏,徐华东. 铬酸盐低水平长期职业接触与劳动者早期健康效应[J]. 北京大学学报(医学版), 2019, 51(2): 307-314. |
| [4] | 郜鑫, 尚静, 杨敬林, 李前, 陈田, 庞元捷, 张文晓, 栾先国, 朱彤, 贾光. 黑碳和臭氧处理的黑碳对小鼠遗传损伤的比较研究[J]. 北京大学学报(医学版), 2014, 46(3): 400-404. |
|
||