北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (3): 498-505. doi: 10.19723/j.issn.1671-167X.2021.03.010
中国6~22岁学生群体甲乙丙类传染病流行趋势
董彦会1,陈曼曼1,王丽萍2,星一1,宋逸1,邹志勇1,董彬1,李中杰2,马军1,Δ( )
)
- 1.北京大学公共卫生学院,北京大学儿童青少年卫生研究所, 北京 100191
2.中国疾病预防控制中心,传染病预防控制处传染病监测预警重点实验室, 北京 102206
Epidemiological characteristics of infectious diseases of group A, B and C among Chinese students’ population
DONG Yan-hui1,CHEN Man-man1,WANG Li-ping2,XING Yi1,SONG Yi1,ZOU Zhi-yong1,DONG Bin1,LI Zhong-jie2,MA Jun1,Δ( )
)
- 1. Institute of Child and Adolescent Health, School of Public Health, Peking University, Beijing 100191, China
2. Division of Infectious Disease Control and Prevention, Key Laboratory of Surveillance and Early Warning on Infectious Disease, Chinese Centre for Disease Control and Prevention, Beijing 102206, China
摘要:
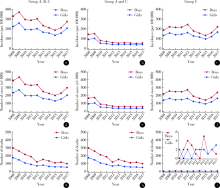
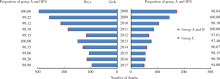
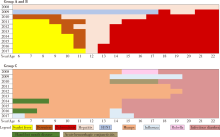
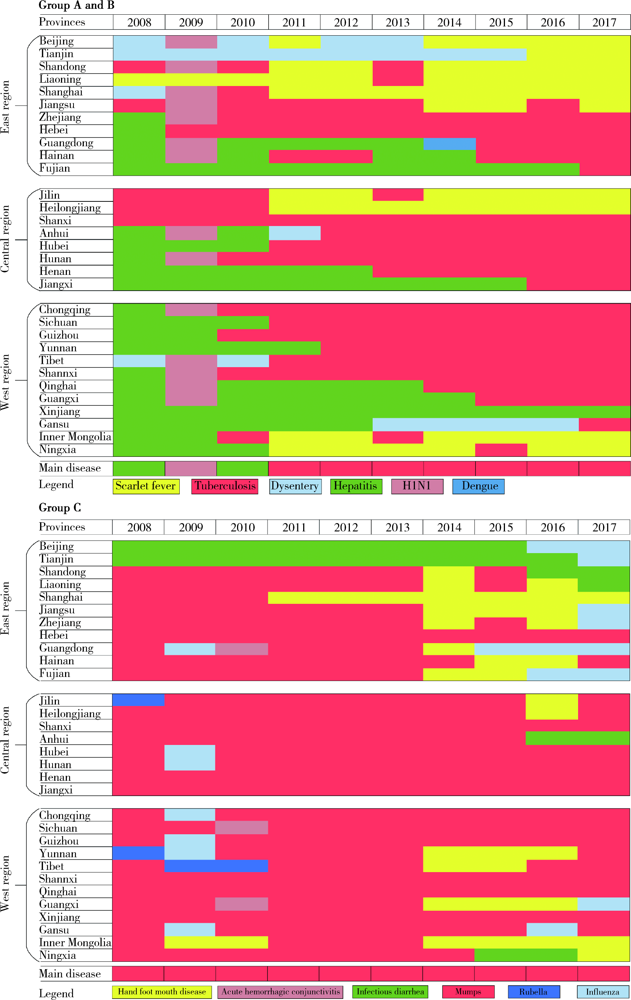
目的: 分析2008—2017年中国6~22岁学生群体甲乙丙类传染病的长期趋势、顺位变化以及主要传染病在不同年龄组和地区间的变化特征。方法: 选取2008—2017年全国传染病监测数据中诊断为法定报告传染病的学生病例作为研究对象,共涉及到甲乙丙类传染病40种,传染病的发病率和死亡率基于教育部公布年度学生人口数作为分母进行计算,选取各年龄组、各省份在每年度中的发病率最高的传染病作为主要传染病进行分析。结果: 2008—2015年中国6~22岁学生群体传染病发病率和死亡率整体呈波动下降趋势,男生发病率、发病数以及死亡数均高于女生,其中,2008—2015年男女生发病率下降幅度分别为43.4%和40.1%,但在2015—2017年出现反弹,增长幅度分别为47.1%和53.8%,反弹主要由丙类传染病增长导致。10年间,甲乙类传染病发病率的前3位疾病分别由2008年的病毒性肝炎、结核病和痢疾,转变为2017年的结核病、猩红热和病毒性肝炎。甲乙类传染病死亡率的前3位疾病分别由2008年的狂犬病、结核病和人类免疫缺陷病毒(human immunodeficiency virus,HIV)/获得性免疫缺陷综合征(acquired immune deficiency syndrome,AIDS),转变为2017年的HIV/AIDS、狂犬病和结核病。丙类传染病发病率和死亡顺位变化并不明显。在年龄组和地区分析中,甲乙类传染病主要以病毒性肝炎、猩红热和结核病为主,丙类传染病则以流行性腮腺炎和感染性腹泻病为主,但近年来,流感和手足口病在东部地区增长明显。结论: 2008—2017年间,我国在学生群体传染病防控方面成就显著,但传染病变化模式和特征显示出我国未来在防控呼吸道传染病、HIV/AIDS等性传播疾病以及新型突发传染病方面的迫切需求,本研究为全国学校卫生传染病防控机制的政策制定提供了重要基础。
中图分类号:
- R181.32
| [1] |
Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990-2013: A systematic subnational analysis for the Global Burden of Disease Study 2013[J]. Lancet, 2016,387(10015):251-272.
doi: 10.1016/S0140-6736(15)00551-6 |
| [2] |
Azzopardi PS, Hearps SJC, Francis KL, et al. Progress in adolescent health and wellbeing: Tracking 12 headline indicators for 195 countries and territories, 1990-2016[J]. Lancet, 2019,393(10176):1101-1118.
doi: S0140-6736(18)32427-9 pmid: 30876706 |
| [3] |
Hui DS, I Azhar E, Madani TA, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health: The latest 2019 novel coronavirus outbreak in Wuhan, China[J]. Int J Infect Dis, 2020,91:264-266.
doi: 10.1016/j.ijid.2020.01.009 |
| [4] |
Li Z, Gao GF. Infectious disease trends in China since the SARS outbreak[J]. Lancet Infect Dis, 2017,17(11):1113-1115.
doi: 10.1016/S1473-3099(17)30579-0 |
| [5] |
Wang L, Chu C, Yang G, et al. Transmission characteristics of different students during a school outbreak of (H1N1) pdm09 influenza in China, 2009[J]. Sci Rep, 2014,4:5982.
doi: 10.1038/srep05982 |
| [6] |
Zhang QL, He JF, Wu D, et al. Maiden outbreak of chikungunya in Dongguan city, Guangdong province, China: Epidemiological characteristics[J]. PLoS One, 2012,7(8):e42830.
doi: 10.1371/journal.pone.0042830 |
| [7] |
Lamagni T, Guy R, Chand M, et al. Resurgence of scarlet fever in England, 2014-16: A population-based surveillance study[J]. Lancet Infect Dis, 2018,18(2):180-187.
doi: 10.1016/S1473-3099(17)30693-X |
| [8] |
Park DW, Kim SH, Park JW, et al. Incidence and characteristics of scarlet fever, South Korea, 2008-2015[J]. Emerg Infect Dis, 2017,23(4):658-661.
doi: 10.3201/eid2304.160773 |
| [9] |
Liu Y, Chan TC, Yap LW, et al. Resurgence of scarlet fever in China: A 13-year population-based surveillance study[J]. Lancet Infect Dis, 2018,18(8):903-912.
doi: 10.1016/S1473-3099(18)30231-7 |
| [10] | Dong Y, Wang L, Burgner DP, et al. Infectious diseases in children and adolescents in China: Analysis of national surveillance data from 2008 to 2017[J]. BMJ, 2020,369:m1043. |
| [11] | 国务院联防联控机制新闻发布会文字实录[C]. (2020-04-21) [2020-09-16]. http://www.nhc.gov.cn/xcs/s3574/202004/3e16b2976000411da737c70523e05522.shtml. |
| [12] | 中华人民共和国国务院. 血吸虫病防治条例[S]. (2006-04-01)[2020-09-12]. http://www.gov.cn/flfg/2006-04/11/content_251237.htm. |
| [13] |
Wang L, Utzinger J, Zhou XN. Schistosomiasis control: Expe-riences and lessons from China[J]. Lancet, 2008,372(9652):1793-1795.
doi: 10.1016/S0140-6736(08)61358-6 |
| [14] | WHO. First WHO report on neglected tropical diseases[R]. (2020-01-01) [2020-08-20]. https://apps.who.int/iris/bitstream/handle/10665/44440/9789241564090_eng.pdf;jsessionid=590A 04986BB10FB0FE811B9A3DEFB5E3?sequence=1. |
| [15] | 卫生部. 关于印发《中国消除疟疾行动计划(2010—2020年)》的通知[EB]. (2010-05-19) [2020-09-15]. http://www.nhc.gov.cn/zwgk/wtwj/201304/15a4cc7a40b0452191fe409590ca99d8.shtml. |
| [16] |
Mehta NS, Mytton OT, Mullins EWS, et al. SARS-CoV-2 (COVID-19): What do we know about children? A systematic review[J]. Clin Infect Dis, 2020,71(9):2469-2479.
doi: 10.1093/cid/ciaa556 |
| [17] |
Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 among children in China[J]. Pediatrics, 2020,145(6):e20200702.
doi: 10.1542/peds.2020-0702 |
| [18] | 潘松, 王宏伟, 李威, 等. 学校症状监测系统预警传染病爆发的实例研究[J]. 中国学校卫生, 2008,29(12):1107-1108. |
| [19] | 吴尊友. 我国艾滋病经性传播新特征与防治面临的挑战[J]. 中华流行病学杂志, 2018,39(6):707-709. |
| [20] | 中国疾病预防控制中心性病艾滋病预防控制中心. 艾滋病防治宣传教育核心信息[R]. (2019-11) [2020-09-20]. http://ncaids.chinacdc.cn/sjb/2019azbsjb/201910/t20191024_206453.htm. |
| [21] | 国家卫生和计划生育委员会. 建立疫情通报制度进一步加强学校艾滋病防控工作[EB]. (2015-08-10)[2020-10-06] http://www.gov.cn/zhengce/2015-08/10/content_2910626.htm. |
| [1] | 李成跃, 王浩, 阿力木江·依米提·塔尔肯. 1985——2019年新疆维吾尔族中小学生生长发育的长期趋势[J]. 北京大学学报(医学版), 2024, 56(5): 802-808. |
| [2] | 蔡珊,张依航,陈子玥,刘云飞,党佳佳,师嫡,李佳欣,黄天彧,马军,宋逸. 北京市中小学生身体活动时间现状及影响因素的路径[J]. 北京大学学报(医学版), 2024, 56(3): 403-410. |
| [3] | 李卫民,祖菲娅·吐尔地. 维吾尔族、哈萨克族和汉族大学生体重指数与体能指数的关系[J]. 北京大学学报(医学版), 2024, 56(3): 411-417. |
| [4] | 张祖洪,陈天娇,马军. 中小学生青春发动时相与心血管代谢危险因素的相关性[J]. 北京大学学报(医学版), 2024, 56(3): 418-423. |
| [5] | 闫晓晋,刘云飞,马宁,党佳佳,张京舒,钟盼亮,胡佩瑾,宋逸,马军. 《中国儿童发展纲要(2011-2020年)》实施期间中小学生营养不良率变化及其政策效应分析[J]. 北京大学学报(医学版), 2023, 55(4): 593-599. |
| [6] | 姚晓莹,刘志科,李宁,马瑞,赵薛飞,张良,许国章,詹思延,方挺. 2015—2019年宁波市0~36月龄婴幼儿癫痫发病的流行病学研究[J]. 北京大学学报(医学版), 2021, 53(3): 485-490. |
| [7] | 李远骋, 崔闻心, 郭雪儿, 朱璠, 刘思辰, 贾碧波, 汪培, 马迎华. 青年学生男男性行为人群中人类免疫缺陷病毒阳性与阴性者获得性免疫缺陷综合征(艾滋病)相关知识与行为比较[J]. 北京大学学报(医学版), 2021, 53(3): 511-517. |
| [8] | 宋逸,罗冬梅,胡佩瑾,闫晓晋,张京舒,雷园婷,张冰,马军. 1985--2014年中国汉族13~18岁中学生体质健康达标优秀率趋势分析[J]. 北京大学学报(医学版), 2020, 52(2): 317-322. |
| [9] | 吴双胜,杨鹏,李海月,马春娜,王全意. 传染病健康素养水平与传染病症状发生之间的相关性研究[J]. 北京大学学报(医学版), 2018, 50(5): 937-940. |
| [10] | 宋逸,雷园婷,胡佩瑾,张冰,马军. 2014年全国汉族中小学生身体素质现况分析[J]. 北京大学学报(医学版), 2018, 50(3): 436-442. |
| [11] | 刘园,栾庆先. 北京石景山社区中老年人群慢性牙周炎和颈动脉内膜中层厚度的相关性[J]. 北京大学学报(医学版), 2018, 50(2): 264-270. |
| [12] | 程吟楚,潘勇平,张洋,潘昱廷,丁呈怡,曹宇,卓琳,方任飞,高爱钰,郭晶,李爱军,付强,马军,詹思延. 北京市中学生药品安全认知与行为调查[J]. 北京大学学报(医学版), 2017, 49(6): 1038-1043. |
| [13] | 宋逸,胡佩瑾,董彦会,张冰,马军. 2014年全国各省、自治区、直辖市汉族学生视力不良现况分析[J]. 北京大学学报(医学版), 2017, 49(3): 433-438. |
| [14] | 张欣,娜荷芽,叶墨,王梦楠,魏少明,孙亚慧,张复兵,孙昕霙,常春,史宇晖. 北京大学生艾滋病相关知识、态度、行为的变化特点及影响因素[J]. 北京大学学报(医学版), 2017, 49(3): 462-468. |
| [15] | 王怡欣,马迎华,李恬静,胡翼飞,彭华参. 同性交友平台上青年学生的艾滋病知识和艾滋病相关行为现状[J]. 北京大学学报(医学版), 2017, 49(3): 469-475. |
|
||