北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (3): 511-519. doi: 10.19723/j.issn.1671-167X.2022.03.017
2011—2020年宁波市鄞州区炎症性肠病发病的流行病学研究
贺冰洁1,刘志科1,沈鹏2,孙烨祥2,陈彬3,詹思延1,4,*( ),林鸿波2,*(
),林鸿波2,*( )
)
- 1. 北京大学公共卫生学院流行病与卫生统计学系,北京 100191
2. 鄞州区疾病预防控制中心,浙江宁波 315199
3. 宁波市肛肠医院,浙江宁波 315048
4. 北京大学人工智能研究院,北京 100191
Epidemiological study on the incidence of inflammatory bowel disease in Yinzhou District, Ningbo City from 2011 to 2020
Bing-jie HE1,Zhi-ke LIU1,Peng SHEN2,Ye-xiang SUN2,Bin CHEN3,Si-yan ZHAN1,4,*( ),Hong-bo LIN2,*(
),Hong-bo LIN2,*( )
)
- 1. Department of Epidemiology and Biostatistics, Peking University School of Public Health, Beijing 100191, China
2. Yinzhou District Center for Disease Control and Prevention, Ningbo 315199, Zhejiang, China
3. Ningbo Anorectal Hospital, Ningbo 315048, Zhejiang, China
4. Institute for Artificial Intelligence, Peking University, Beijing 100191, China
摘要:
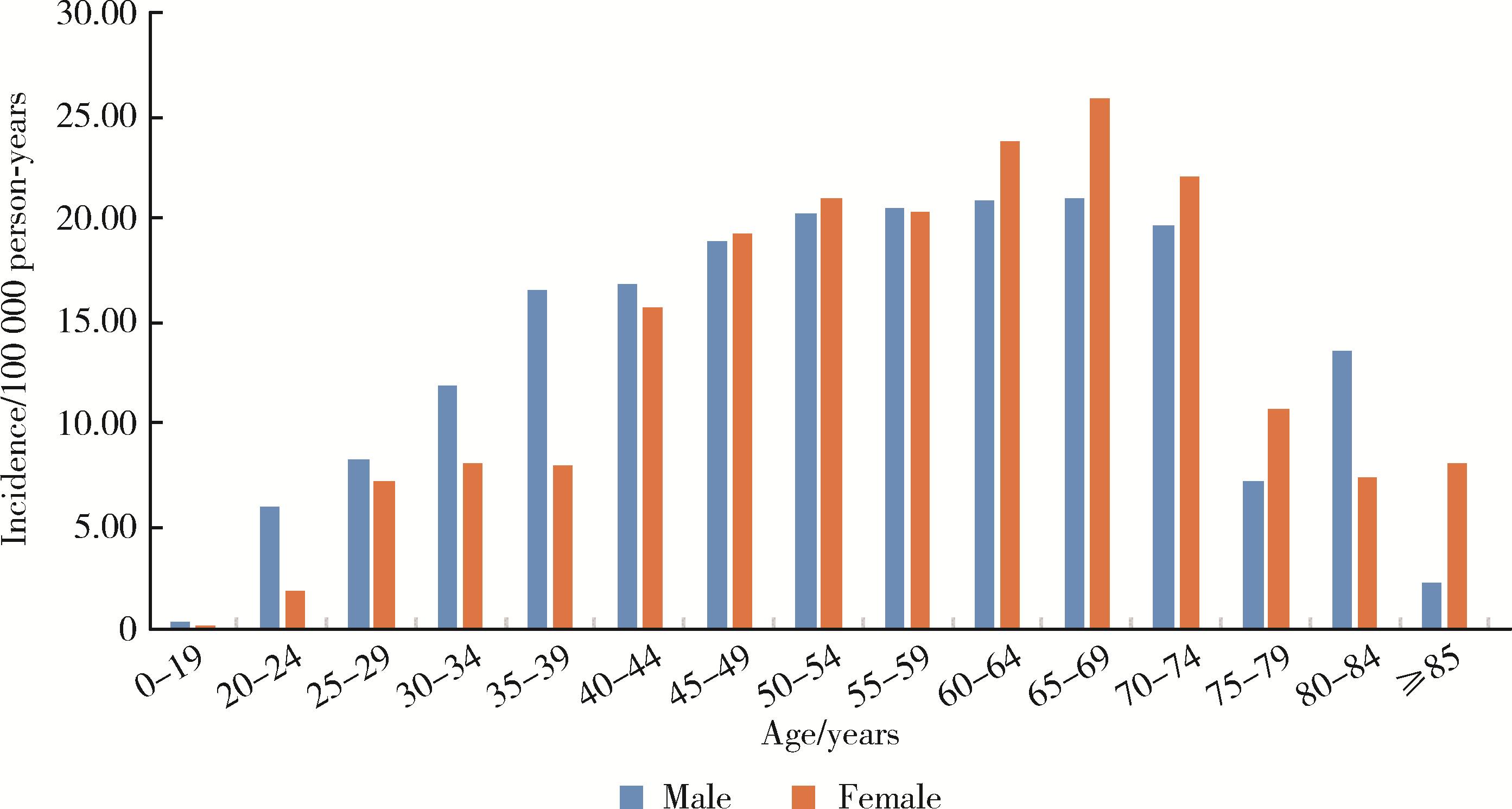
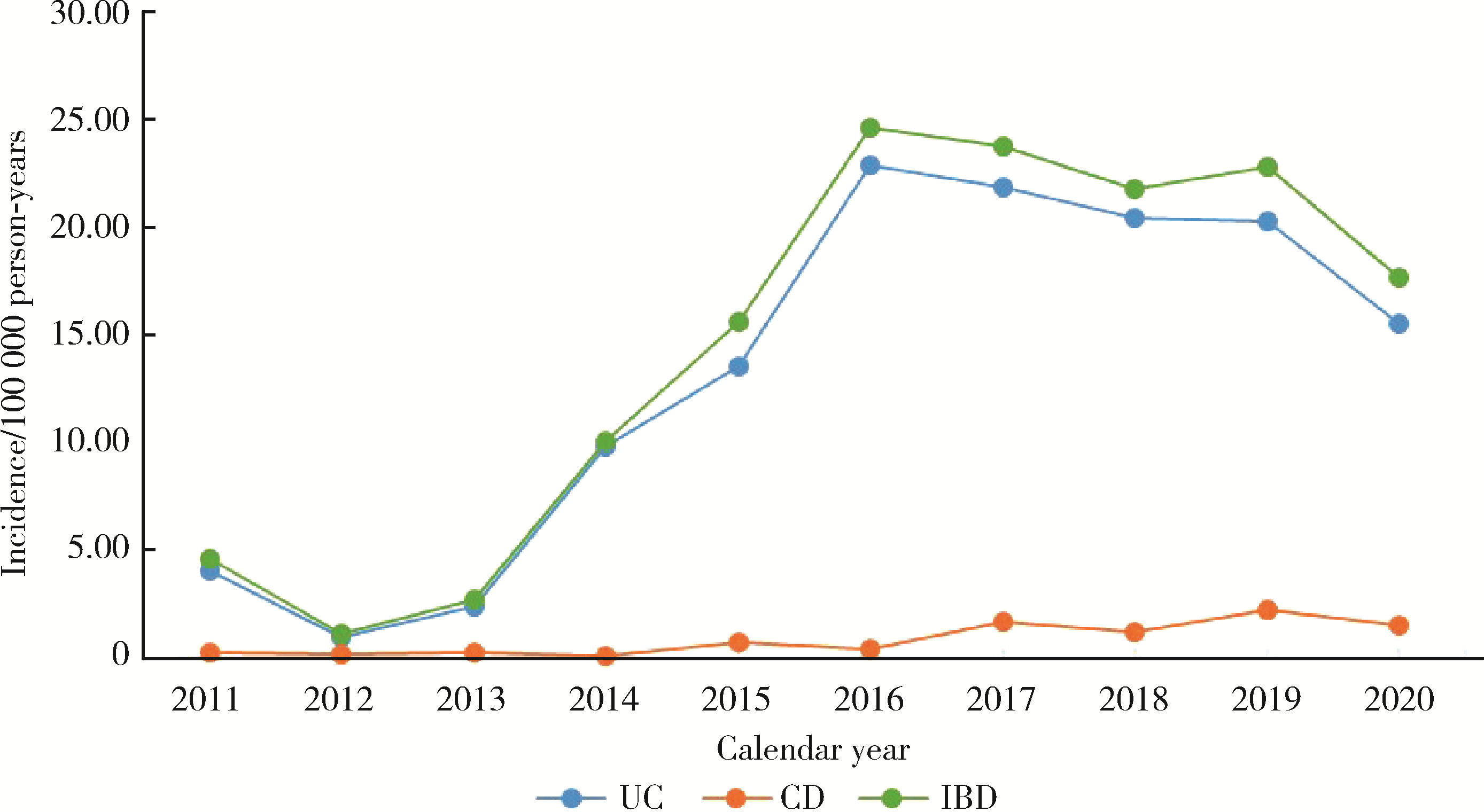
目的: 描述宁波市鄞州区常住居民炎症性肠病发病的分布特征,了解该地区炎症性肠病的疾病负担和发展趋势。方法: 采用回顾性队列设计,收集2010—2020年鄞州区全民健康信息平台的居民健康档案中所有常住居民的登记信息,利用电子病历随访其炎症性肠病就诊情况,设置1年洗脱期,以登记1年后首次诊断且以炎症性肠病为首要诊断的患者为新发病例。采用泊松分布估算炎症性肠病的发病密度及其95%置信区间(confidence interval, CI)。结果: 2011—2020年累计纳入鄞州区常住居民1 496 427人,其中男性729 996人(48.78%),总随访人年8 081 030.82,中位随访人年5.41 [四分位距(interquartile range, IQR): 5.29]。研究期间共有1 217例炎症性肠病新发病例,男性(624例,51.27%)多于女性(593例,48.73%),总发病密度为15.06/10万人年(95%CI: 14.23, 15.93),其中溃疡性结肠炎1 106例(90.88%),发病密度为13.69/10万人年(95%CI: 12.89, 14.52);克罗恩病70例(5.75%),发病密度为0.87/10万人年(95%CI: 0.68, 1.09);未定型结肠炎41例(3.37%),发病密度为0.51/10万人年(95%CI: 0.36, 0.69)。溃疡性结肠炎的中位发病年龄为50.82岁(IQR: 18.77),发病年龄在45~49岁组占比最高(15.01%);发病密度随年龄增长逐渐上升,45~49岁年龄组达到较高水平,随后略有上升,65~69岁年龄组发病密度最高,为25.44/10万人年(95%CI: 20.85, 30.75),至75~79岁组发病密度迅速下降;克罗恩病的中位发病年龄为44.34岁(IQR: 33.41),发病年龄在25~29岁组占比最高(12.86%),由于克罗恩病新发病例数较少,年龄分布波动较大,青年和老年各有峰值。2011—2020年间,鄞州区炎症性肠病的发病密度在2011—2013年处于较低水平,2014—2016年呈迅速上升趋势,2016年达到峰值[24.62/10万人年(95%CI: 21.31, 28.30)],2017—2020年略有下降。结论: 2011—2020年鄞州区炎症性肠病发病密度呈较高水平,医疗机构和卫生部门需重视其所带来的疾病负担。
中图分类号:
- R181.2
| 1 | 葛均波, 徐永健. 内科学[M]. 8版 北京: 人民卫生出版社, 2013: 385- 393. |
| 2 |
中华医学会消化病学分会炎症性肠病学组. 炎症性肠病诊断与治疗的共识意见(2012年·广州)[J]. 胃肠病学, 2012, 17 (12): 763- 781.
doi: 10.3969/j.issn.1008-7125.2012.12.013 |
| 3 |
张玉洁, 梁洁, 吴开春. 炎症性肠病诊断与治疗的共识意见(2018年, 北京)溃疡性结肠炎部分解读[J]. 中华消化杂志, 2018, 38 (5): 312- 314.
doi: 10.3760/cma.j.issn.0254-1432.2018.05.003 |
| 4 |
Ungaro R , Mehandru S , Allen PB , et al. Ulcerative colitis[J]. Lancet, 2017, 389 (10080): 1756- 1770.
doi: 10.1016/S0140-6736(16)32126-2 |
| 5 |
冉志华, 童锦禄. 炎症性肠病诊断与治疗的共识意见(2018年, 北京)克罗恩病部分解读[J]. 中华消化杂志, 2018, 38 (5): 315- 317.
doi: 10.3760/cma.j.issn.0254-1432.2018.05.004 |
| 6 |
Torres J , Mehandru S , Colombel JF , et al. Crohn's disease[J]. Lancet, 2017, 389 (10080): 1741- 1755.
doi: 10.1016/S0140-6736(16)31711-1 |
| 7 |
Alatab S , Sepanlou SG , Ikuta K , et al. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990—2017: a systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet Gastroenterol Hepatol, 2020, 5 (1): 17- 30.
doi: 10.1016/S2468-1253(19)30333-4 |
| 8 |
李学锋, 彭霞, 周明欢. 我国炎症性肠病流行病学研究进展[J]. 现代消化及介入诊疗, 2020, 25 (9): 1265- 1267.
doi: 10.3969/j.issn.1672-2159.2020.09.032 |
| 9 | Qiu Y , Ren W , Liu Y , et al. Disease burden of inflammatory bowel disease in China from 1990 to 2017: findings from the Glo-bal Burden of Diseases 2017[J]. E Clin Med, 2020, 27, 100544. |
| 10 |
中华医学会消化病学分会炎症性肠病学组. 炎症性肠病诊断与治疗的共识意见(2018年·北京)[J]. 中华炎性肠病杂志, 2018, 2 (3): 173- 190.
doi: 10.3760/cma.j.issn.2096-367X.2018.03.005 |
| 11 |
Cui G , Yuan A . A systematic review of epidemiology and risk factors associated with Chinese inflammatory bowel disease[J]. Front Med, 2018, 5, 183.
doi: 10.3389/fmed.2018.00183 |
| 12 |
Li X , Song P , Li J , et al. The disease burden and clinical characteristics of inflammatory bowel disease in the Chinese population: a systematic review and meta-analysis[J]. Int J Environ Res Public Health, 2017, 14 (3): 238.
doi: 10.3390/ijerph14030238 |
| 13 | Qiao Y , Ran Z . Potential influential factors on incidence and pre-valence of inflammatory bowel disease in mainland China[J]. JGH Open, 2019, 4 (1): 11- 15. |
| 14 |
Huang K , Tao S , Zhou X , et al. Incidence rates of health outcomes of interest among Chinese children exposed to selected vaccines in Yinzhou Electronic Health Records: a population-based retrospective cohort study[J]. Vaccine, 2020, 38 (18): 3422- 3428.
doi: 10.1016/j.vaccine.2020.03.013 |
| 15 | 鄞州区普查中心. 鄞州区人口普查公报数据解读[EB/OL]. (2021-05-19)[2021-11-22]. http://www.nbyz.gov.cn/art/2021/5/19/art_1229108054_59071135.html. |
| 16 |
林鸿波, 刘翠丽, 沈鹏, 等. 基于鄞州区域医疗数据的利巴韦林临床使用的分析[J]. 中国药物警戒, 2018, 15 (2): 73- 77.
doi: 10.3969/j.issn.1672-8629.2018.02.003 |
| 17 |
Yang Y , Zhou X , Gao S , et al. Evaluation of electronic healthcare databases for post-marketing drug safety surveillance and pharmacoepidemiology in China[J]. Drug Saf, 2018, 41 (1): 125- 137.
doi: 10.1007/s40264-017-0589-z |
| 18 | 浙江省人民政府. 浙江省人民政府关于调整宁波市部分行政区划的通知[EB/OL]. (2016-09-30)[2021-11-22]. http://www.zj.gov.cn/art/2016/9/30/art_1229017138_64597.html. |
| 19 |
Keyashian K , Dehghan M , Sceats L , et al. Comparative incidence of inflammatory bowel disease in different age groups in the United States[J]. Inflamm Bowel Dis, 2019, 25 (12): 1983- 1989.
doi: 10.1093/ibd/izz092 |
| 20 |
Jung YS , Han M , Kim WH , et al. Incidence and clinical outcomes of inflammatory bowel disease in South Korea, 2011—2014: a nationwide population-based study[J]. Dig Dis Sci, 2017, 62 (8): 2102- 2112.
doi: 10.1007/s10620-017-4640-9 |
| 21 |
Kaplan GG , Windsor JW . The four epidemiological stages in the global evolution of inflammatory bowel disease[J]. Nat Rev Gastroenterol Hepatol, 2021, 18 (1): 56- 66.
doi: 10.1038/s41575-020-00360-x |
| 22 |
Zeng Z , Zhu Z , Yang Y , et al. Incidence and clinical characteristics of inflammatory bowel disease in a developed region of Guangdong Province, China: a prospective population-based study[J]. J Gastroenterol Hepatol, 2013, 28 (7): 1148- 1153.
doi: 10.1111/jgh.12164 |
| 23 |
Yang H , Li Y , Wu W , et al. The incidence of inflammatory bowel disease in Northern China: a prospective population-based study[J]. PLoS One, 2014, 9 (7): e101296.
doi: 10.1371/journal.pone.0101296 |
| 24 | Zhao J , Ng SC , Lei Y , et al. First prospective, population-based inflammatory bowel disease incidence study in mainland of China: the emergence of "Western" disease[J]. Inflamm Bowel Dis, 2013, 19 (9): 1839- 1845. |
| 25 |
Ng SC , Tang W , Ching JY , et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn' s and colitis epidemiology study[J]. Gastroenterology, 2013, 145 (1): 158- 165.
doi: 10.1053/j.gastro.2013.04.007 |
| 26 | 缪佳蓉. 云南省炎症性肠病流行病学特征、环境及复发因素的研究[D]. 云南: 昆明医科大学, 2015. |
| 27 |
Shivashankar R , Tremaine WJ , Harmsen WS , et al. Incidence and prevalence of Crohn's disease and ulcerative colitis in Olms-ted County, Minnesota from 1970 through 2010[J]. Clin Gastroenterol Hepatol, 2017, 15 (6): 857- 863.
doi: 10.1016/j.cgh.2016.10.039 |
| 28 |
Kotze PG , Underwood FE , Damião A , et al. Progression of inflammatory bowel diseases throughout Latin America and the Caribbean: a systematic review[J]. Clin Gastroenterol Hepatol, 2020, 18 (2): 304- 312.
doi: 10.1016/j.cgh.2019.06.030 |
| 29 |
Burisch J , Munkholm P . The epidemiology of inflammatory bowel disease[J]. Scand J Gastroenterol, 2015, 50 (8): 942- 951.
doi: 10.3109/00365521.2015.1014407 |
| 30 |
Mak WY , Zhao M , Ng SC , et al. The epidemiology of inflammatory bowel disease: east meets west[J]. J Gastroenterol Hepatol, 2020, 35 (3): 380- 389.
doi: 10.1111/jgh.14872 |
| 31 |
Loftus EV Jr. , Silverstein MD , Sandborn WJ , et al. Ulcerative colitis in Olmsted County, Minnesota, 1940—1993: incidence, prevalence, and survival[J]. Gut, 2000, 46 (3): 336- 343.
doi: 10.1136/gut.46.3.336 |
| 32 | 浙江统计数据库. 鄞州区地区生产总值统计[EB/OL]. (2021-02-22)[2021-10-22]. http://data.tjj.zj.gov.cn/page/dataquery.simpleMacro/newQuery/newQuery.jsp?getData=nianduData&ddiUrn=urn:ddi:ZJJCKSTAT:a463a4d9-806b-4fcc-8fc9-b43a8ee4298c:1&dataClassific=yandu&sjztId=urn:ddi:ZJJCKSTAT:8c1a842d-cf0b-40b5-b355-ec4c8d90c506:1&sjztB-gq=N&orgCode=330212&proDemo=zj. |
| 33 | 浙江统计数据库. 鄞州区人均生产总值统计[EB/OL]. (2021-02-22)[2021-10-22]. http://data.tjj.zj.gov.cn/page/dataquery.simpleMacro/newQuery/newQuery.jsp?getData=nianduData&ddiUrn=urn:ddi:ZJJCKSTAT:a463a4d9-806b-4fcc-8fc9-b43a8ee4298c:1&dataClassific=yandu&sjztId=urn:ddi:ZJJCKSTAT:8c1a842d-cf0b-40b5-b355-ec4c8d90c506:1&sjztB-gq=N&orgCode=330212&proDemo=zj. |
| 34 |
Chen Y . Perspectives of IBD China: is Crohn's and colitis foundation model a solution to health care issues for the country?[J]. Inflamm Bowel Dis, 2018, 24 (5): 925- 929.
doi: 10.1093/ibd/izy056 |
| 35 |
Ng SC , Shi HY , Hamidi N , et al. Worldwide incidence and pre-valence of inflammatory bowel disease in the 21st century: a syste-matic review of population-based studies[J]. Lancet, 2017, 390 (10114): 2769- 2778.
doi: 10.1016/S0140-6736(17)32448-0 |
| [1] | 岳芷涵,韩娜,鲍筝,吕瑾莨,周天一,计岳龙,王辉,刘珏,王海俊. 儿童早期体重指数轨迹与超重风险关联的前瞻性队列研究[J]. 北京大学学报(医学版), 2024, 56(3): 390-396. |
| [2] | 吴芸,徐亚兰,张国艳,张媛媛,王峻瑶,尤鹏,彭涛,刘玉兰,陈宁. 乌司奴单抗对克罗恩病临床缓解及透壁愈合的疗效[J]. 北京大学学报(医学版), 2024, 56(2): 253-259. |
| [3] | 马会超,李军,王永清. 妊娠合并炎症性肠病的临床特点[J]. 北京大学学报(医学版), 2024, 56(2): 260-266. |
| [4] | 刘晓强,周寅. 牙种植同期植骨术围术期高血压的相关危险因素[J]. 北京大学学报(医学版), 2024, 56(1): 93-98. |
| [5] | 于欢,杨若彤,王斯悦,吴俊慧,王梦莹,秦雪英,吴涛,陈大方,武轶群,胡永华. 2型糖尿病患者使用二甲双胍与缺血性脑卒中发病风险的队列研究[J]. 北京大学学报(医学版), 2023, 55(3): 456-464. |
| [6] | 马涛,李艳辉,陈曼曼,马莹,高迪,陈力,马奇,张奕,刘婕妤,王鑫鑫,董彦会,马军. 青春期启动提前与儿童肥胖类型的关联研究: 基于横断面调查和队列调查[J]. 北京大学学报(医学版), 2022, 54(5): 961-970. |
| [7] | 刘杰,郭超. 正/负性情绪对中国老年人死亡风险影响的前瞻性队列研究[J]. 北京大学学报(医学版), 2022, 54(2): 255-260. |
| [8] | 周吴平,穆楠,简伟研,王化虹. 克罗恩病患者疾病经济负担现状与相关因素[J]. 北京大学学报(医学版), 2021, 53(3): 555-559. |
| [9] | 姚晓莹,刘志科,李宁,马瑞,赵薛飞,张良,许国章,詹思延,方挺. 2015—2019年宁波市0~36月龄婴幼儿癫痫发病的流行病学研究[J]. 北京大学学报(医学版), 2021, 53(3): 485-490. |
| [10] | 刘晓强,杨洋,周建锋,刘建彰,谭建国. 640例单牙种植术对血压和心率影响的队列研究[J]. 北京大学学报(医学版), 2021, 53(2): 390-395. |
| [11] | 刘欢,何映东,刘金波,黄薇,赵娜,赵红薇,周晓华,王宏宇. 血管健康指标对新发心脑血管事件的预测价值:北京血管健康分级标准的初步验证[J]. 北京大学学报(医学版), 2020, 52(3): 514-520. |
| [12] | 孟文颖,黄琬桐,张杰,焦明远,金蕾,靳蕾. 孕早期血清维生素E水平与妊娠期高血压疾病发病风险的关系[J]. 北京大学学报(医学版), 2020, 52(3): 470-478. |
| [13] | 唐迅,张杜丹,刘晓非,刘秋萍,曹洋,李娜,黄少平,窦会东,高培,胡永华. China-PAR脑卒中模型在北方农村人群中预测脑卒中发病风险的应用[J]. 北京大学学报(医学版), 2020, 52(3): 444-450. |
| [14] | 李军,牛占岳,薛艳,石雪迎,张波,王媛. 重度溃疡性结肠炎合并卡波西肉瘤1例并文献综述[J]. 北京大学学报(医学版), 2020, 52(2): 373-377. |
| [15] | 王婷婷,韩影,高芳芳,叶磊,张育军. 环状RNA circ-SOD2对肠上皮屏障和溃疡性结肠炎的作用[J]. 北京大学学报(医学版), 2019, 51(5): 805-812. |
|
||