北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (3): 537-542. doi: 10.19723/j.issn.1671-167X.2023.03.021
全内镜下突出腰椎间盘摘除术后功能状态的影响因素
- 1. 北京大学第三医院疼痛科, 北京 100191
2. 首都医科大学附属北京友谊医院骨科, 北京 100050
Influential factors related to functional status after full-endoscopic lumbar discectomy
Wei ZHU1,Bin ZHU1,2,*( ),Xiao-guang LIU1
),Xiao-guang LIU1
- 1. Department of Pain Medicine, Peking University Third Hospital, Beijing 100191, China
2. Department of Orthopedic, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China
摘要:
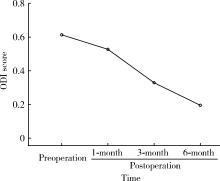
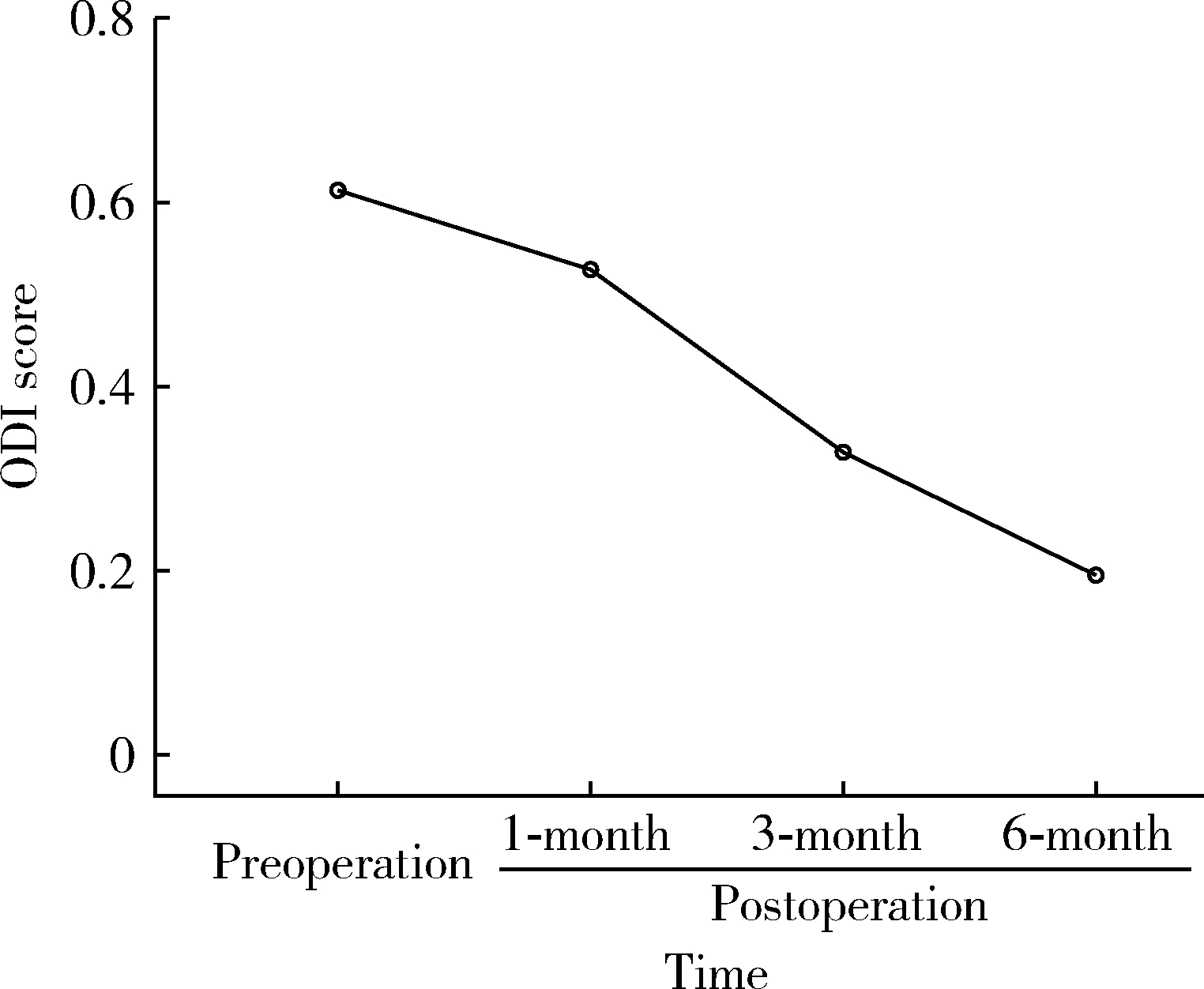
目的: 探索影响全内镜下突出腰椎间盘摘除术后患者功能状态的因素。方法: 采用前瞻性研究,收集符合入选标准并且完成全部随访的96例患者的一般资料、疼痛视觉模拟评分(visual analogue scale,VAS)、Oswestry功能障碍指数(Oswestry disability index,ODI)评分、广泛性焦虑障碍-7(generalised anxiety disorder-7,GAD-7)量表评分和患者健康问卷-9(patient health questionnaire-9,PHQ-9)量表评分。采用重复测量方差分析方法研究患者在术前及术后1、3、6个月的ODI评分变化,采用多元回归分析探索患者术后ODI评分的影响因素,采用Logistic回归分析探索患者术后6个月恢复正常工作状态的危险因素。结果: 患者整体术后功能状态有明显改善,其术后的功能状态与正在经历的疼痛强度呈高度正相关。影响术后功能状态的因素在不同康复时期有所不同,术后1个月和3个月时,影响术后功能状态的因素均为当前的平均疼痛强度;术后6个月时,影响术后功能状态的因素包括当前的平均疼痛强度、术前平均疼痛强度、性别和文化程度;影响患者术后6个月恢复正常工作状态的危险因素包括女性、低龄、术前抑郁状态、术后3个月平均疼痛强度高。结论: 全内镜下突出腰椎间盘摘除手术治疗慢性腰腿痛具有较好的可行性;患者术后功能状态恢复过程中,医务人员除需要采取镇痛措施降低患者经历的疼痛强度外,还需要关注心理社会因素对术后功能状态的影响;女性、低龄、术前抑郁状态、术后3个月平均疼痛强度高的患者可能会延迟术后恢复正常工作状态的时间。
中图分类号:
- R681.53
| 1 | 王琦, 倪家骧. 慢性疼痛的评估与治疗策略[J]. 中国医刊, 2005, 40 (4): 201- 203. |
| 2 |
Bair M , Wu J , Damush T , et al. Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients[J]. Psychosom Med, 2008, 70 (8): 890- 897.
doi: 10.1097/PSY.0b013e318185c510 |
| 3 | 刘丽丽, 王维宁. 疼痛日记对腰椎间盘突出症患者恐动症和恐惧回避信念的影响[J]. 护理学杂志, 2015, 30 (10): 25- 28. |
| 4 |
Shi R , Wang F , Hong X , et al. Comparison of percutaneous endoscopic lumbar discectomy versus microendoscopic discectomy for the treatment of lumbar disc herniation: A meta-analysis[J]. Int Orthop, 2019, 43 (4): 923- 937.
doi: 10.1007/s00264-018-4253-8 |
| 5 | 祝斌, 刘晓光, 李水清, 等. 内镜下无血管间隙减压技术治疗腰椎间盘突出症[J]. 中国疼痛医学杂志, 2017, 23 (2): 117- 121. |
| 6 | 符祖昶, 王清铿, 尤瑞金, 等. 经皮椎间孔镜治疗腰椎间盘突出症的临床效果[J]. 中国医药导报, 2017, 14 (18): 80- 83. |
| 7 | Watson J , Ryan C , Cooper L , et al. Pain neuroscience education for adults with chronic musculoskeletal pain: A mixed-methods systematic review and meta-analysis[J]. J Pain, 2019, 20 (10): 1140. e1- 1140. e22. |
| 8 | Louw A , Zimney K , Puentedura E , et al. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature[J]. Physiother Theory Pract, 2016, 32 (5): 332- 355. |
| 9 | Nijs J , Clark J , Malfliet A , et al. In the spine or in the brain? Recent advances in pain neuroscience applied in the intervention for low back pain[J]. Clin Exp Rheumatol, 2017, 107 (5): 108- 115. |
| 10 | Steenstra I , Munhall C , Irvin E , et al. Systematic review of prognostic factors for return to work in workers with sub-acute and chronic low back pain[J]. J Occup Rehabil, 2017, 27 (3): 369- 381. |
| [1] | 李志存, 吴天俣, 梁磊, 范宇, 孟一森, 张骞. 穿刺活检单针阳性前列腺癌术后病理升级的危险因素分析及列线图模型构建[J]. 北京大学学报(医学版), 2024, 56(5): 896-901. |
| [2] | 颜野,李小龙,夏海缀,朱学华,张羽婷,张帆,刘可,刘承,马潞林. 前列腺癌根治术后远期膀胱过度活动症的危险因素[J]. 北京大学学报(医学版), 2024, 56(4): 589-593. |
| [3] | 陈延,李况蒙,洪锴,张树栋,程建星,郑仲杰,唐文豪,赵连明,张海涛,姜辉,林浩成. 阴茎海绵体注射试验对阴茎血管功能影响的回顾性研究[J]. 北京大学学报(医学版), 2024, 56(4): 680-686. |
| [4] | 庞博,郭桐君,陈曦,郭华棋,石嘉章,陈娟,王欣梅,李耀妍,单安琪,余恒意,黄婧,汤乃军,王艳,郭新彪,李国星,吴少伟. 天津与上海35岁以上人群氮氧化物个体暴露水平及其影响因素[J]. 北京大学学报(医学版), 2024, 56(4): 700-707. |
| [5] | 和静,房中则,杨颖,刘静,马文瑶,霍勇,高炜,武阳丰,谢高强. 血浆中脂质代谢分子与颈动脉粥样硬化斑块、传统心血管危险因素及膳食因素的关系[J]. 北京大学学报(医学版), 2024, 56(4): 722-728. |
| [6] | 蔡珊,张依航,陈子玥,刘云飞,党佳佳,师嫡,李佳欣,黄天彧,马军,宋逸. 北京市中小学生身体活动时间现状及影响因素的路径[J]. 北京大学学报(医学版), 2024, 56(3): 403-410. |
| [7] | 张祖洪,陈天娇,马军. 中小学生青春发动时相与心血管代谢危险因素的相关性[J]. 北京大学学报(医学版), 2024, 56(3): 418-423. |
| [8] | 林郁婷,王华丽,田宇,巩俐彤,常春. 北京市老年人认知功能的影响因素[J]. 北京大学学报(医学版), 2024, 56(3): 456-461. |
| [9] | 朱金荣,赵亚娜,黄巍,赵微微,王悦,王松,苏春燕. 感染新型冠状病毒的血液透析患者的临床特征[J]. 北京大学学报(医学版), 2024, 56(2): 267-272. |
| [10] | 赖展鸿,李嘉辰,贠泽霖,张永刚,张昊,邢晓燕,邵苗,金月波,王乃迪,李依敏,李玉慧,栗占国. 特发性炎性肌病完全临床应答相关因素的单中心真实世界研究[J]. 北京大学学报(医学版), 2024, 56(2): 284-292. |
| [11] | 司筱芊,赵秀娟,朱凤雪,王天兵. 创伤出血性休克后急性呼吸窘迫综合征的危险因素[J]. 北京大学学报(医学版), 2024, 56(2): 307-312. |
| [12] | 李洋洋,侯林,马紫君,黄山雅美,刘捷,曾超美,秦炯. 孕期因素与婴儿牛奶蛋白过敏的关系[J]. 北京大学学报(医学版), 2024, 56(1): 144-149. |
| [13] | 刘晓强,周寅. 牙种植同期植骨术围术期高血压的相关危险因素[J]. 北京大学学报(医学版), 2024, 56(1): 93-98. |
| [14] | 罗靓,李云,王红彦,相晓红,赵静,孙峰,张晓盈,贾汝琳,李春. 抗内皮细胞抗体检测在早期流产中的预测价值[J]. 北京大学学报(医学版), 2023, 55(6): 1039-1044. |
| [15] | 游芳凝,罗靓,刘香君,张学武,李春. 未分化结缔组织病患者的妊娠结局、疾病演变及其影响因素[J]. 北京大学学报(医学版), 2023, 55(6): 1045-1052. |
|
||