北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (1): 66-73. doi: 10.19723/j.issn.1671-167X.2024.01.011
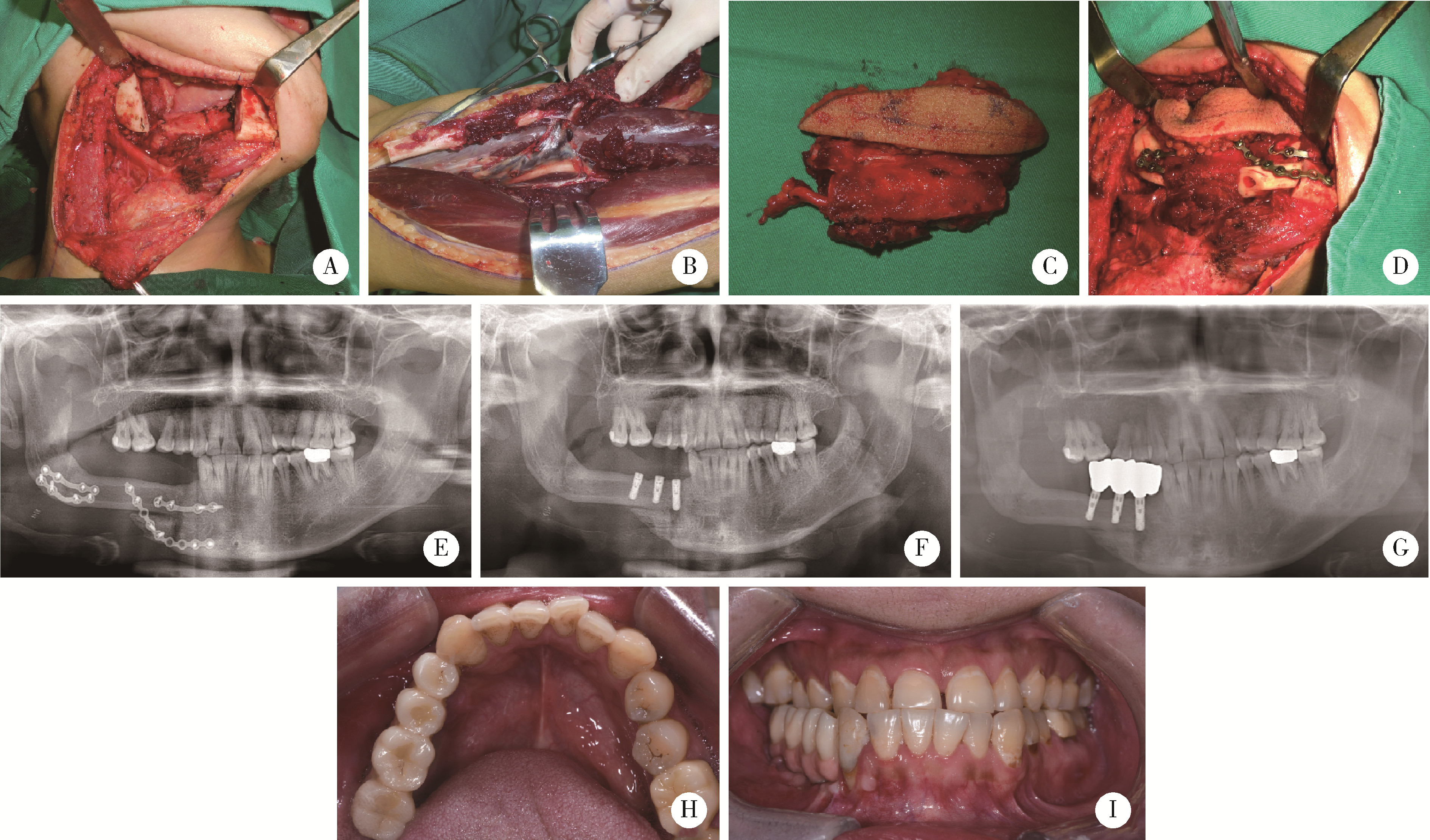
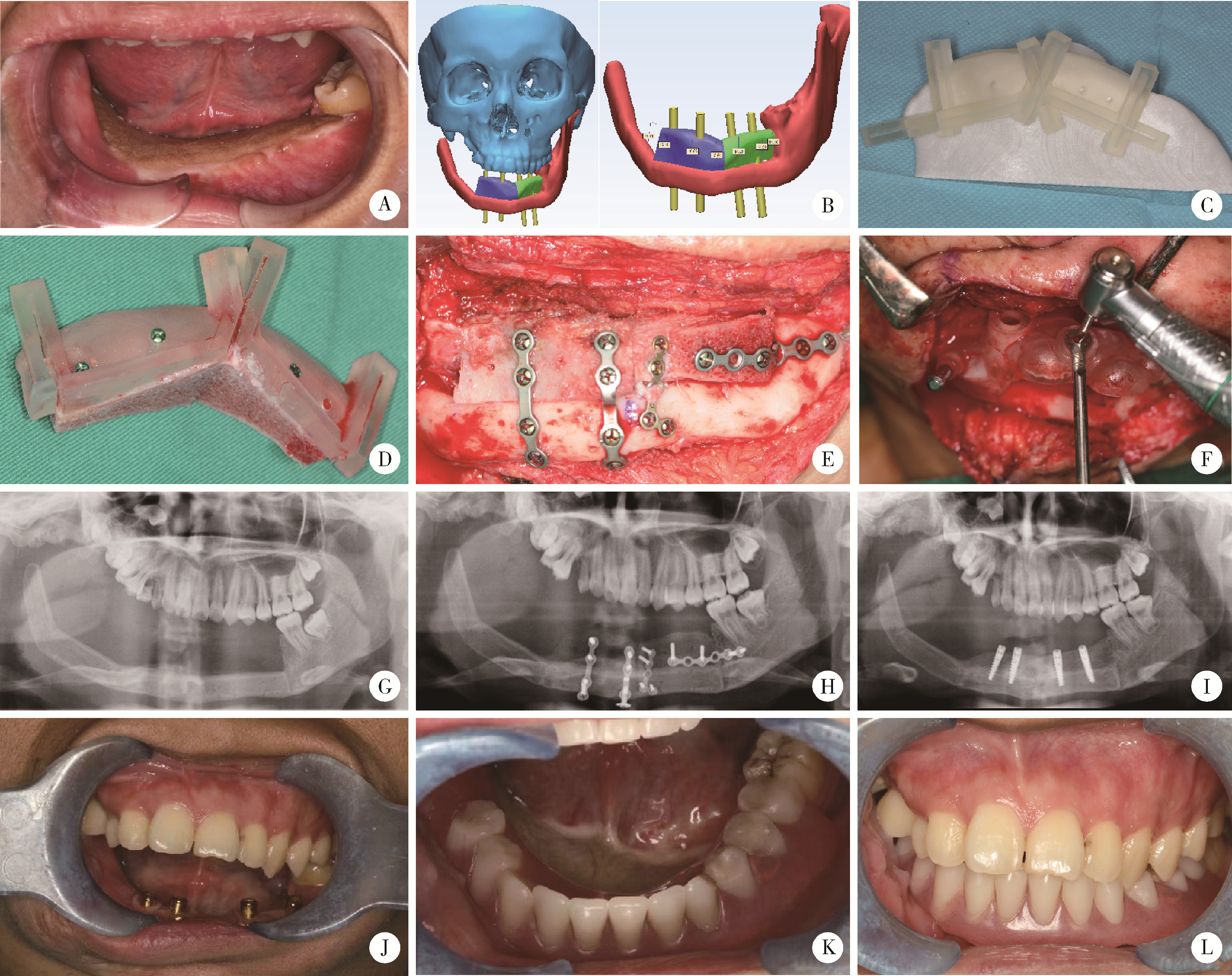
游离腓骨瓣修复下颌骨缺损术后义齿修复的临床分析
- 北京大学口腔医学院·口腔医院口腔颌面外科,国家口腔医学中心,国家口腔疾病临床医学研究中心,口腔生物材料和数字诊疗装备国家工程研究中心,口腔数字医学北京市重点实验室,国家卫生健康委员会口腔医学计算机应用工程技术研究中心,北京 100081
Clinical analysis of denture rehabilitation after mandibular fibula free-flap reconstruction
Congwei WANG,Min GAO,Yao YU,Wenbo ZHANG,Xin PENG*( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry, Beijing 100081, China
摘要:
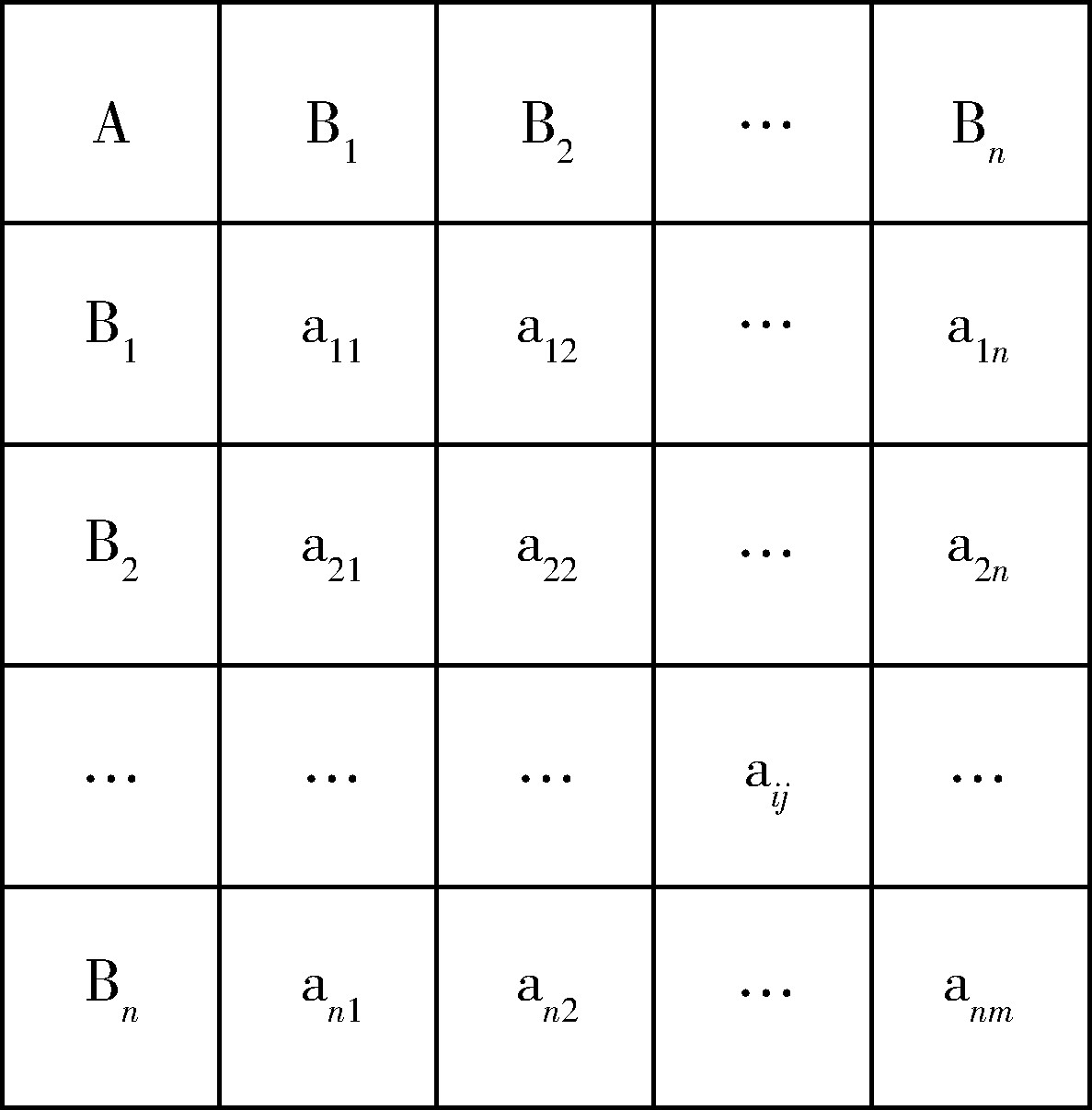
目的: 分析游离腓骨瓣重建下颌骨缺损患者术后义齿修复情况,并对义齿功能进行评价。方法: 收集2015年1月至2020年12月期间154例因炎症、外伤、肿瘤等原因实施下颌骨节段切除,并采用血管化游离腓骨瓣修复下颌骨缺损的患者,回顾相关资料并随访调查患者义齿修复的相关情况,同时对义齿修复功能评价的各指标进行专家权威赋值,获得义齿功能评分。采用SPSS 18.0软件对纳入研究患者的基本信息和患者义齿修复情况进行统计分析。结果: 游离腓骨瓣修复下颌骨缺损患者术后义齿修复率为17.5%,其中,下颌骨良性肿瘤患者采用腓骨瓣修复的术后义齿修复率为25.0%(18/72例),明显高于恶性肿瘤患者的术后义齿修复率11.0%(9/82例,P < 0.05)。缺损累及髁突和不累及髁突的患者在义齿修复率和义齿功能评分上差异均无统计学意义(P>0.05)。种植义齿修复患者的义齿功能评分显著高于活动义齿修复的患者(P < 0.05)。根据Brown分类,缺损累及下颌骨前牙区患者的义齿功能评分显著高于未累及下颌骨前牙区的患者(P < 0.05)。因口内条件差而未行义齿修复的患者约占未行义齿修复患者总数的37.9%,是未行义齿修复的最主要原因。结论: 游离腓骨瓣重建下颌骨缺损的义齿修复情况与肿瘤性质、口内条件等关系密切,种植义齿的临床修复效果更佳,是未来颌骨重建后义齿修复的更优选择。
中图分类号:
- R782.2
| 1 |
Wallace CG , Chang YM , Tsai CY , et al. Harnessing the potential of the free fibula osteoseptocutaneous flap in mandible reconstruction[J]. Plast Reconstr Surg, 2010, 125 (1): 305- 314.
doi: 10.1097/PRS.0b013e3181c2bb9d |
| 2 |
Iizuka T , Häfliger J , Seto I , et al. Oral rehabilitation after mandibular reconstruction using an osteocutaneous fibula free flap with endosseous implants. Factors affecting the functional outcome in patients with oral cancer[J]. Clin Oral Implants Res, 2005, 16 (1): 69- 79.
doi: 10.1111/j.1600-0501.2004.01076.x |
| 3 |
Parbo N , Murra NT , Andersen K , et al. Outcome of partial mandibular reconstruction with fibula grafts and implant-supported prostheses[J]. Int J Oral Maxillofac Surg, 2013, 42 (11): 1403- 1408.
doi: 10.1016/j.ijom.2013.05.007 |
| 4 |
Lilly GL , Petrisor D , Wax MK . Mandibular rehabilitation: From the Andy Gump deformity to jaw-in-a-day[J]. Laryngoscope Investig Otolaryngol, 2021, 6 (4): 708- 720.
doi: 10.1002/lio2.595 |
| 5 |
Petrovic I , Ahmed ZU , Huryn JM , et al. Oral rehabilitation for patients with marginal and segmental mandibulectomy: A retrospective review of 111 mandibular resection prostheses[J]. J Prosthet Dent, 2019, 122 (1): 82- 87.
doi: 10.1016/j.prosdent.2018.09.020 |
| 6 |
Brown JS , Barry C , Ho M , et al. A new classification for mandi-bular defects after oncological resection[J]. Lancet Oncol, 2016, 17 (1): e23- e30.
doi: 10.1016/S1470-2045(15)00310-1 |
| 7 |
Jacobsen HC , Wahnschaff F , Trenkle T , et al. Oral rehabilitation with dental implants and quality of life following mandibular reconstruction with free fibular flap[J]. Clin Oral Investig, 2016, 20 (1): 187- 192.
doi: 10.1007/s00784-015-1487-3 |
| 8 |
Bodard AG , Salino S , Desoutter A , et al. Assessment of functio-nal improvement with implant-supported prosthetic rehabilitation after mandibular reconstruction with a microvascular free fibula flap: A study of 25 patients[J]. J Prosthet Dent, 2015, 113 (2): 140- 145.
doi: 10.1016/j.prosdent.2014.08.005 |
| 9 |
Patel SY , Kim DD , Ghali GE . Maxillofacial reconstruction using vascularized fibula free flaps and endosseous implants[J]. Oral Maxillofac Surg Clin North Am, 2019, 31 (2): 259- 284.
doi: 10.1016/j.coms.2018.12.005 |
| 10 |
Li R , Meng Z , Zhang Y , et al. Soft tissue management: A critical part of implant rehabilitation after vascularized free-flap reconstruction[J]. J Oral Maxillofac Surg, 2021, 79 (3): 560- 574.
doi: 10.1016/j.joms.2020.11.006 |
| 11 |
Smith Nobrega A , Santiago JF Jr , de Faria Almeida DA , et al. Irradiated patients and survival rate of dental implants: A systematic review and meta-analysis[J]. J Prosthet Dent, 2016, 116 (6): 858- 866.
doi: 10.1016/j.prosdent.2016.04.025 |
| 12 |
Schiegnitz E , Reinicke K , Sagheb K , et al. Dental implants in patients with head and neck cancer: A systematic review and meta-analysis of the influence of radiotherapy on implant survival[J]. Clin Oral Implants Res, 2022, 33 (10): 967- 999.
doi: 10.1111/clr.13976 |
| 13 |
Lee ZH , Avraham T , Monaco C , et al. Optimizing functional outcomes in mandibular condyle reconstruction with the free fibula flap using computer-aided design and manufacturing technology[J]. J Oral Maxillofac Surg, 2018, 76 (5): 1098- 1106.
doi: 10.1016/j.joms.2017.11.008 |
| 14 |
González-García R , Naval-Gías L , Rodríguez-Campo FJ , et al. Vascularized fibular flap for reconstruction of the condyle after mandibular ablation[J]. J Oral Maxillofac Surg, 2008, 66 (6): 1133- 1137.
doi: 10.1016/j.joms.2007.06.680 |
| 15 |
Powers DB , Breeze J , Erdmann D . Vascularized fibula TMJ reconstruction: A report of five cases featuring computerized patient-specific surgical planning[J]. Plast Reconstr Surg Glob Open, 2022, 10 (8): e4465.
doi: 10.1097/GOX.0000000000004465 |
| 16 |
Yu Y , Zhang WB , Liu XJ , et al. Three-dimensional accuracy of virtual planning and surgical navigation for mandibular reconstruction with free fibula flap[J]. J Oral Maxillofac Surg, 2016, 74 (7): 1503.e1- e10.
doi: 10.1016/j.joms.2016.02.020 |
| 17 |
Smolka K , Kraehenbuehl M , Eggensperger N , et al. Fibula free flap reconstruction of the mandible in cancer patients: Evaluation of a combined surgical and prosthodontic treatment concept[J]. Oral Oncol, 2008, 44 (6): 571- 581.
doi: 10.1016/j.oraloncology.2007.07.005 |
| 18 | Brauner E , Valentini V , Jamshir S , et al. Retrospective review of 78 rehabilitated head and neck postoncological patients: A new classification method[J]. Minerva Stomatol, 2016, 65 (1): 17- 32. |
| 19 |
Roumanas ED , Garrett N , Blackwell KE , et al. Masticatory and swallowing threshold performances with conventional and implant-supoprted prostheses after mandibular fibula free-flap reconstruction[J]. J Prosthet Dent, 2006, 96 (4): 289- 297.
doi: 10.1016/j.prosdent.2006.08.015 |
| 20 |
Lodders JN , van Baar GJC , Vergeer MR , et al. Implant-based dental rehabilitation in head and neck cancer patients after maxillofacial reconstruction with a free vascularized fibula flap: The effect on health-related quality of life[J]. Support Care Cancer, 2022, 30 (6): 5411- 5420.
doi: 10.1007/s00520-022-06944-4 |
| 21 |
Sozzi D , Novelli G , Silva R , et al. Implant rehabilitation in fibula-free flap reconstruction: A retrospective study of cases at 1-18 years following surgery[J]. J Craniomaxillofac Surg, 2017, 45 (10): 1655- 1661.
doi: 10.1016/j.jcms.2017.06.021 |
| 22 |
Pellegrino G , Tarsitano A , Ferri A , et al. Long-term results of osseointegrated implant-based dental rehabilitation in oncology patients reconstructed with a fibula free flap[J]. Clin Implant Dent Relat Res, 2018, 20 (5): 852- 859.
doi: 10.1111/cid.12658 |
| 23 | Ali R , Al-Khayatt A , Barclay C . The use of dental implants, cast bars and sleeve overdentures in oral cancer patients[J]. Br Dent J, 2018, 224 (8): 611- 619. |
| [1] | 丁茜,李文锦,孙丰博,谷景华,林元华,张磊. 表面处理对氧化钇和氧化镁稳定的氧化锆种植体晶相及断裂强度的影响[J]. 北京大学学报(医学版), 2023, 55(4): 721-728. |
| [2] | 孙菲,刘建,李思琪,危伊萍,胡文杰,王翠. 种植体黏膜下微生物在健康种植体和种植体周炎中的构成与差异:一项横断面研究[J]. 北京大学学报(医学版), 2023, 55(1): 30-37. |
| [3] | 蔡天怡,章文博,于尧,王洋,毛驰,郭传瑸,俞光岩,彭歆. 头颈部游离组织瓣移植术后预防性气管切开的临床分析[J]. 北京大学学报(医学版), 2022, 54(2): 363-368. |
| [4] | 梁峰,吴敏节,邹立东. 后牙区单牙种植修复5年后的临床修复疗效观察[J]. 北京大学学报(医学版), 2021, 53(5): 970-976. |
| [5] | 释栋,曹婕,戴世爱,孟焕新. 植体周炎再生治疗短期疗效观察[J]. 北京大学学报(医学版), 2020, 52(1): 58-63. |
| [6] | 林春平,卢松鹤,朱浚鑫,胡洪成,岳兆国,唐志辉. 个性化根形种植体的螺纹形态对周围牙槽骨应力分布影响的三维有限元分析[J]. 北京大学学报(医学版), 2019, 51(6): 1130-1137. |
| [7] | 刘潇倩,陈秋雯,冯海兰,王兵,屈健,孙振,衡墨迪,潘韶霞. 无牙颌患者locator附着体种植覆盖义齿修复后口腔卫生维护的纵向研究[J]. 北京大学学报(医学版), 2019, 51(1): 136-144. |
| [8] | 吴敏节,邹立东,梁峰. 上前牙即刻种植即刻修复负载3年后软、硬组织变化的临床观察[J]. 北京大学学报(医学版), 2018, 50(4): 694-699. |
| [9] | 刘婧寅,陈飞,葛严军,魏菱,潘韶霞,冯海兰. 选择性激光熔化种植体对早期骨矿化沉积率的影响[J]. 北京大学学报(医学版), 2018, 50(1): 117-122. |
| [10] | 梁乃文,石磊,黄颖,邓旭亮. 不同形貌纯钛表面对人脐静脉内皮细胞生物学行为的影响[J]. 北京大学学报(医学版), 2017, 49(1): 43-048. |
| [11] | 李贝贝, 林野, 崔宏燕, 郝强, 胥加斌, 邸萍. 碳纤维增强“All-on-4”即刻修复体的临床评价[J]. 北京大学学报(医学版), 2016, 48(1): 133-137. |
| [12] | 崔宏燕, 邸萍, 李健慧, 林野, 刘蓉蓉. 电火花蚀刻技术在种植修复体制作中的应用[J]. 北京大学学报(医学版), 2015, 47(2): 336-339. |
| [13] | 韩劼, 陈智滨, 李玮, 孟焕新. 早期愈合阶段牙种植体周沟液骨代谢相关因子的检测和种植体稳定性共振频率分析[J]. 北京大学学报(医学版), 2015, 47(1): 37-41. |
| [14] | 吴敏节, 张相皞, 邹立东, 梁峰. 临时冠成型术后1年牙龈稳定性的临床观察[J]. 北京大学学报(医学版), 2014, 46(6): 954-957. |
| [15] | 赵旭, 邸萍, 林野, 李健慧, 邱立新, 罗佳, 崔宏燕. “All-on-4”无牙颌种植即刻修复技术的初步临床观察[J]. 北京大学学报(医学版), 2014, 46(5): 720-726. |
|
||