北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (4): 656-660. doi: 10.19723/j.issn.1671-167X.2024.04.018
带线输尿管支架自排技术在肾移植受者中的效果及安全性
- 北京大学人民医院泌尿外科, 北京大学应用碎石技术研究所, 北京 100044
Effect and safety of self-draining ureteral stent with thread in kidney transplant reci-pients
Wenbo YANG,Lei YU,Weiyu ZHANG,Tao XU,Qiang WANG*( )
)
- Department of Urology, Peking University People's Hospital; The Institute of Applied Lithotripsy Technology, Peking University, Beijing 100044, China
摘要:
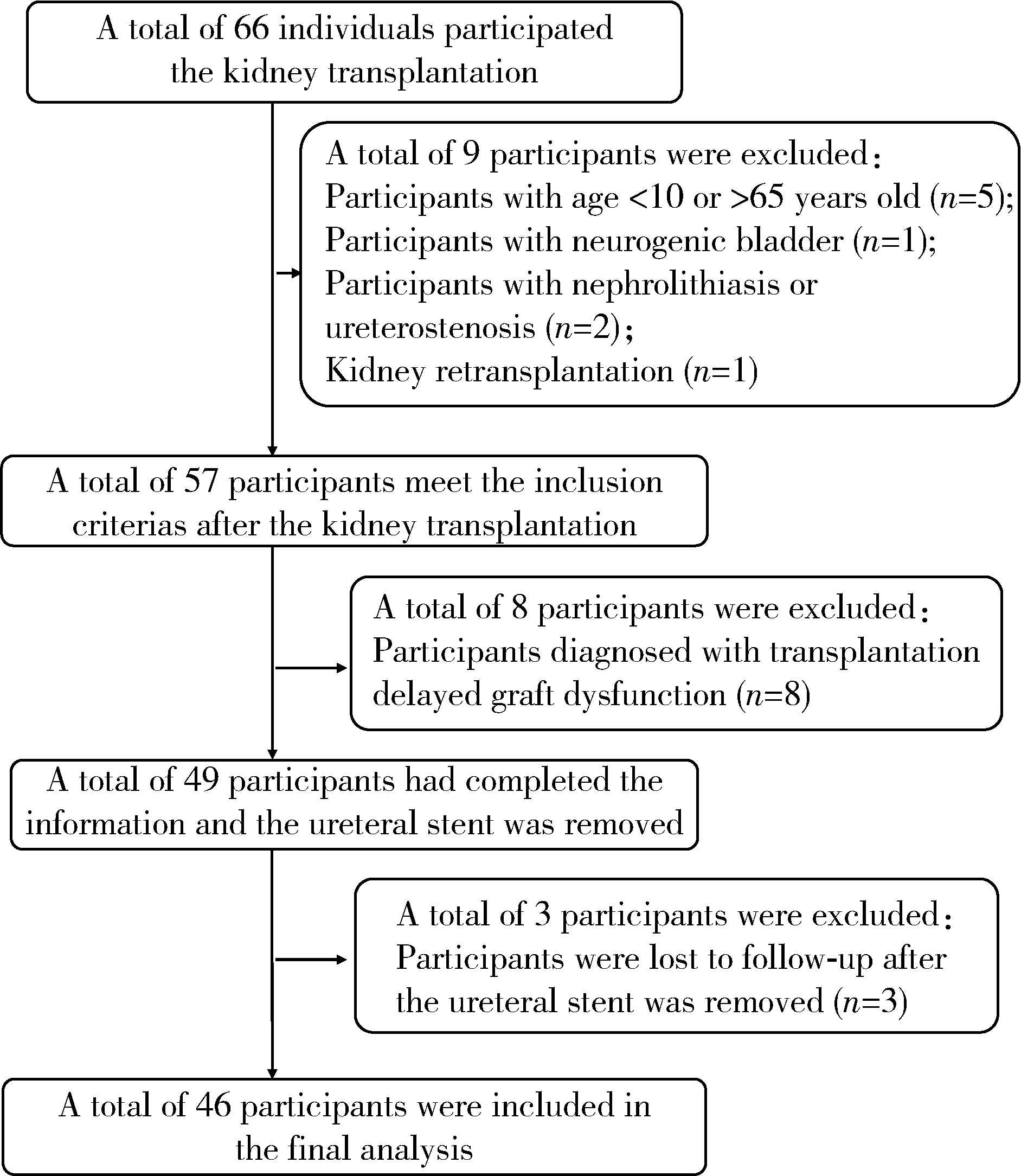
目的: 探讨采用带线输尿管支架自排技术完成肾移植术中输尿管支架置入的临床安全性和有效性。方法: 本研究为前瞻性队列研究,研究对象为2022年11月至2024年1月就诊于北京大学人民医院泌尿外科的肾移植受者,根据情况将其分为带线输尿管支架组和膀胱镜组。带线输尿管支架组术中输尿管支架膀胱端采用2-0慕丝线20~30 cm挂线,术后第9天拔出导尿管时,输尿管支架末端的挂线随尿液排出尿道口,拔除输尿管支架末端挂线时可带出输尿管支架。膀胱镜组肾移植术中常规置入输尿管支架,术后通过膀胱镜尿道局部浸润麻醉下常规拔除输尿管支架。采用成组t检验比较两组留置和拔除输尿管支架的疼痛程度[用数字等级评定量表(numerical rating scale,NRS)-11评分表示],用卡方检验比较两组术后3个月内泌尿系统并发症发生情况,P<0.05为差异有统计学意义。结果: 共纳入46例肾移植受者,其中带线输尿管支架组21例,膀胱镜组25例。截至2024年3月,所有受者术后平均随访6个月(3~12个月)。带线输尿管支架组和膀胱镜组年龄分布、男女比例、死亡供体与活体供体移植物方面差异均没有统计学意义。肾移植术后3个月内膀胱镜组和带线输尿管支架组分别有15例(60%)和4例(19%)发生尿路感染(P=0.007),但两组均未发生明显尿瘘、伤口感染和输尿管狭窄,且均未观察到与支架相关的并发症,也未发现输尿管支架结壳、迁移或结石形成。膀胱镜组和带线输尿管支架组术后留置输尿管支架疼痛评分分别为4.4±2.5和4.6±2.4,差异无统计学意义(t=0.29,P=0.773),但两组输尿管支架拔除时的疼痛评分分别为4.9±1.6和3.0±1.0,差异具有统计学意义(t=5.017,P<0.001)。膀胱镜组和带线输尿管支架组与输尿管支架相关的医疗费用分别为6 452.0(5 539.5,6 452.0)元和3 225.0(3 225.0,3 225.0)元,差异有统计学意义(P<0.001)。结论: 较常规移植肾输尿管支架,带线输尿管支架自排技术操作简便,输尿管支架留置时间短,患者拔除输尿管支架时不适症状减轻,拔除输尿管支架费用显著降低,且术后泌尿系统并发症少,是一种值得推广的改良术式。
中图分类号:
- R693.2
| 1 |
Duty BD , Barry JM . Diagnosis and management of ureteral complications following renal transplantation[J]. Asian J Urol, 2015, 2 (4): 202- 207.
doi: 10.1016/j.ajur.2015.08.002 |
| 2 |
Goldman JD , Julian K . Urinary tract infections in solid organ transplant recipients: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice[J]. Clin Transplant, 2019, 33 (9): e13507.
doi: 10.1111/ctr.13507 |
| 3 | Arabi Z , Al Thiab K , Altheaby A , et al. The impact of timing of stent removal on the incidence of UTI, recurrence, symptoma-tology, resistance, and hospitalization in renal transplant recipients[J]. J Transplant, 2021, 2021, 3428260. |
| 4 | 中华人民共和国卫生部. 医院感染诊断标准(试行)[J]. 中华医学杂志, 2001, 81 (5): 61- 67. |
| 5 | Le HK , Gleber R , Bush RA , et al. Cost analysis of removing pediatric ureteral stents with and without a retrieval string[J]. J Pediatr Urol, 2019, 15 (6): 624. |
| 6 |
Lempinen M , Stenman J , Kyllonen L , et al. Surgical complications following 1 670 consecutive adult renal transplantations: A single center study[J]. Scand J Surg, 2015, 104 (4): 254- 259.
doi: 10.1177/1457496914565419 |
| 7 |
Fiorentino M , Pesce F , Schena A , et al. Updates on urinary tract infections in kidney transplantation[J]. J Nephrol, 2019, 32 (5): 751- 761.
doi: 10.1007/s40620-019-00585-3 |
| 8 |
龚丽英, 张鲁伟, 刘晓立, 等. 肾移植术后泌尿系感染的研究进展[J]. 实用器官移植电子杂志, 2021, 9 (4): 327- 332.
doi: 10.3969/j.issn.2095-5332.2021.04.016 |
| 9 | Saemann M , Horl WH . Urinary tract infection in renal transplant recipients[J]. Eur J Clin Invest, 2008, 38 (Suppl 2): 58- 65. |
| 10 |
Pelle G , Vimont S , Levy PP , et al. Acute pyelonephritis represents a risk factor impairing long-term kidney graft function[J]. Am J Transplant, 2007, 7 (4): 899- 907.
doi: 10.1111/j.1600-6143.2006.01700.x |
| 11 | Simforoosh N , Obeid K , Javanmard B , et al. Stent removal in 200 kidney transplant recipients: Nonoperative versus endoscopic removal[J]. Exp Clin Transplant, 2016, 14 (4): 385- 388. |
| 12 |
Dong J , Lu J , Zu Q , et al. Routine short-term ureteral stent in living donor renal transplantation: Introduction of a simple stent removal technique without using anesthesia and cystoscope[J]. Transplant Proc, 2011, 43 (10): 3747- 3750.
doi: 10.1016/j.transproceed.2011.09.062 |
| 13 |
Visser IJ , van der Staaij JPT , Muthusamy A , et al. Timing of ureteric stent removal and occurrence of urological complications after kidney transplantation: A systematic review and meta-analysis[J]. J Clin Med, 2019, 8 (5): 689.
doi: 10.3390/jcm8050689 |
| [1] | 丁汉东, 王琴, 廖贵益, 郝宗耀. 肾移植术后并发消化道出血的诊治[J]. 北京大学学报(医学版), 2024, 56(5): 902-907. |
| [2] | 王明瑞, 王起, 胡浩, 赖金惠, 唐鑫伟, 万春艳, 许克新, 徐涛. 覆膜金属输尿管支架治疗盆腔脂肪增多症所致肾积水的疗效[J]. 北京大学学报(医学版), 2024, 56(5): 919-922. |
| [3] | 赖金惠,王起,姬家祥,王明瑞,唐鑫伟,许克新,徐涛,胡浩. 新型冠状病毒肺炎疫情期间延迟拔除输尿管支架对泌尿系结石术后患者生活质量和心理状态的影响[J]. 北京大学学报(医学版), 2023, 55(5): 857-864. |
| [4] | 韩金涛,张宇翔,贾子昌,姜除寒,刘恋,栾景源,梁飞,赵彦清. Neuroform Atlas支架辅助弹簧圈栓塞未破裂性颅内宽颈动脉瘤[J]. 北京大学学报(医学版), 2023, 55(1): 139-143. |
| [5] | 李雨柯,王梅,唐琳,刘玉华,陈晓颖. 不同pH值对脱细胞小肠黏膜下层海绵支架螯合锶离子的影响[J]. 北京大学学报(医学版), 2023, 55(1): 44-51. |
| [6] | 张春龙,王明瑞,王起,许克新,徐涛,胡浩. 覆膜金属输尿管支架维持性治疗输尿管镜碎石术后难治性输尿管狭窄的远期疗效评价[J]. 北京大学学报(医学版), 2022, 54(4): 674-679. |
| [7] | 邓艺,张一,李博文,王梅,唐琳,刘玉华. 不同交联剂处理对脱细胞小肠黏膜下层多孔支架的影响[J]. 北京大学学报(医学版), 2022, 54(3): 557-564. |
| [8] | 朱正达,高岩,何汶秀,方鑫,刘洋,魏攀,闫志敏,华红. 红色诺卡氏菌细胞壁骨架治疗糜烂型口腔扁平苔藓的疗效及安全性[J]. 北京大学学报(医学版), 2021, 53(5): 964-969. |
| [9] | 庄金满,李天润,李选,栾景源,王昌明,冯琦琛,韩金涛. Rotarex 旋切导管在下肢动脉硬化闭塞症支架内再狭窄中的应用[J]. 北京大学学报(医学版), 2021, 53(4): 740-743. |
| [10] | 洪鹏,田晓军,赵小钰,杨飞龙,刘茁,陆敏,赵磊,马潞林. 肾移植术后双侧乳头状肾癌1例[J]. 北京大学学报(医学版), 2021, 53(4): 811-813. |
| [11] | 董文敏,王明瑞,胡浩,王起,许克新,徐涛. Allium覆膜金属输尿管支架长期留置治疗输尿管-回肠吻合口狭窄的初期临床经验及随访结果[J]. 北京大学学报(医学版), 2020, 52(4): 637-641. |
| [12] | 李秋钰,程秦,赵志伶,代妮妮,曾琳,朱兰,郭炜,李超,王军红,李姝,葛庆岗,沈宁. 肾移植术后感染新型冠状病毒1例[J]. 北京大学学报(医学版), 2020, 52(4): 780-784. |
| [13] | 赵磊,张洪宪,侯小飞,刘磊,陆敏,韩永,马潞林. 来氟米特联合羟苯磺酸钙治疗肾移植术后BK病毒相关性肾病[J]. 北京大学学报(医学版), 2020, 52(2): 385-389. |
| [14] | 曹春玲,杨聪翀,屈小中,韩冰,王晓燕. 可注射羟乙基壳聚糖基水凝胶理化性能及其对人牙髓细胞增殖和成牙本质向分化的作用[J]. 北京大学学报(医学版), 2020, 52(1): 10-17. |
| [15] | 贾子昌,李选,郑梅,栾景源,王昌明,韩金涛. 复合手术治疗无残端的症状性长段颈内动脉慢性闭塞[J]. 北京大学学报(医学版), 2020, 52(1): 177-180. |
|
||