北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (5): 874-883. doi: 10.19723/j.issn.1671-167X.2024.05.019
老年髋部骨折患者住院期间发生术后心力衰竭的列线图预测模型的构建及验证
- 北京大学第三医院老年内科,北京 100191
Construction and validation of a nomogram for predicting in-hospital postoperative heart failure in elderly patients with hip fracture
Yuanmei LIU, Yicheng FU, Jingxin HAO, Fuchun ZHANG, Huilin LIU*( )
)
- Department of Geriatrics, Peking University Third Hospital, Beijing 100191, China
摘要:
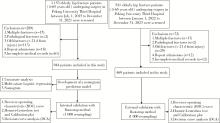
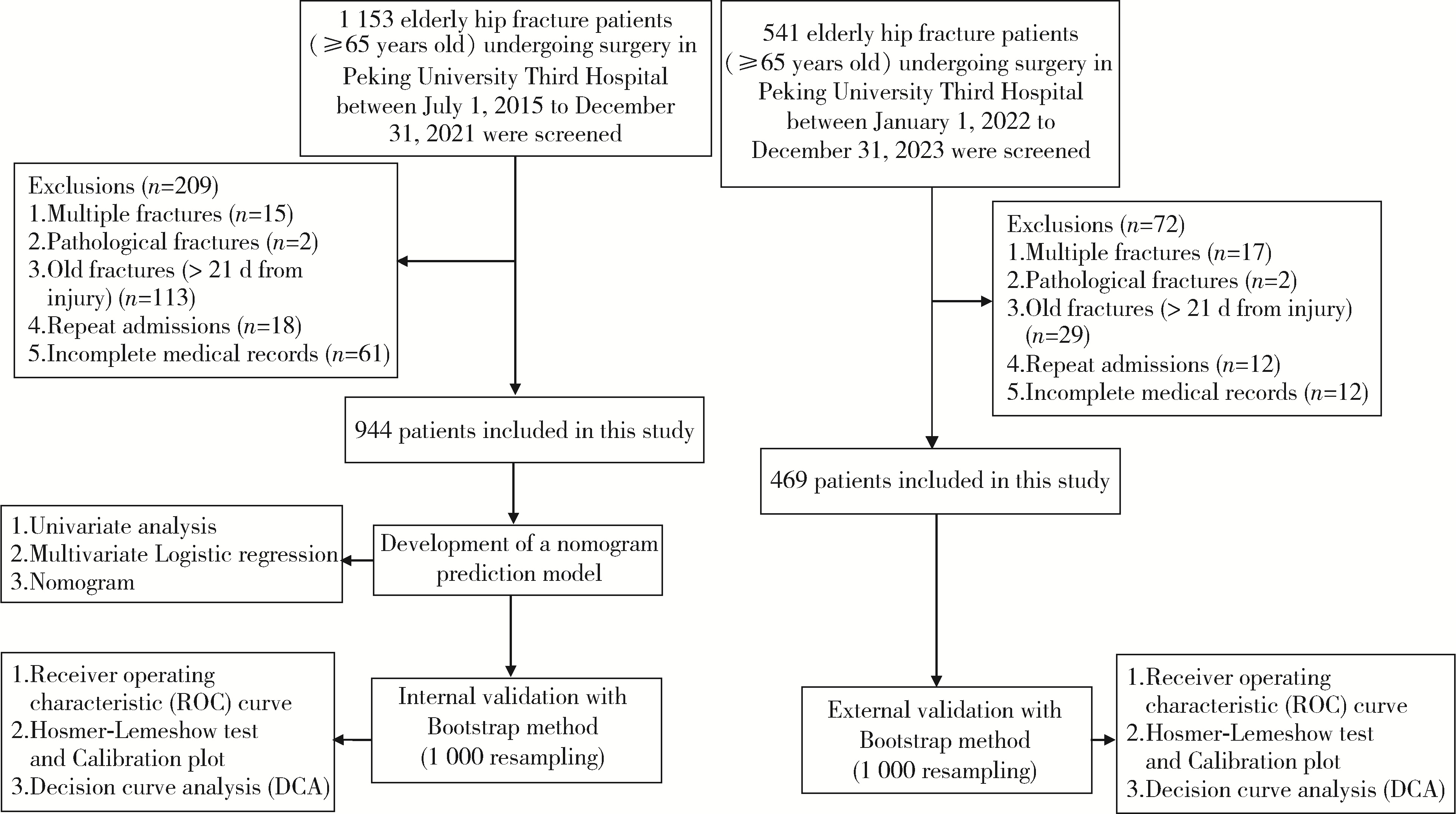
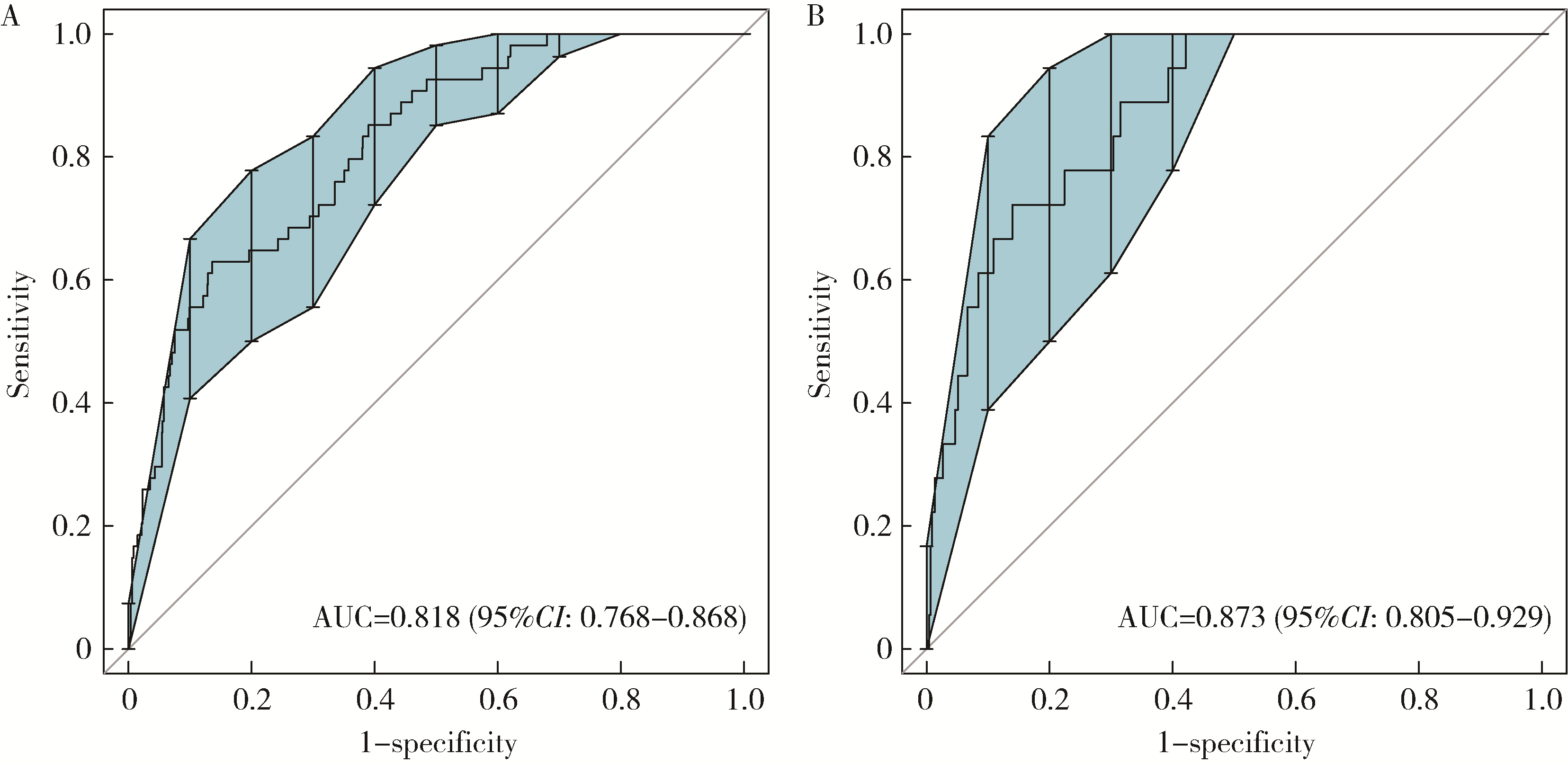
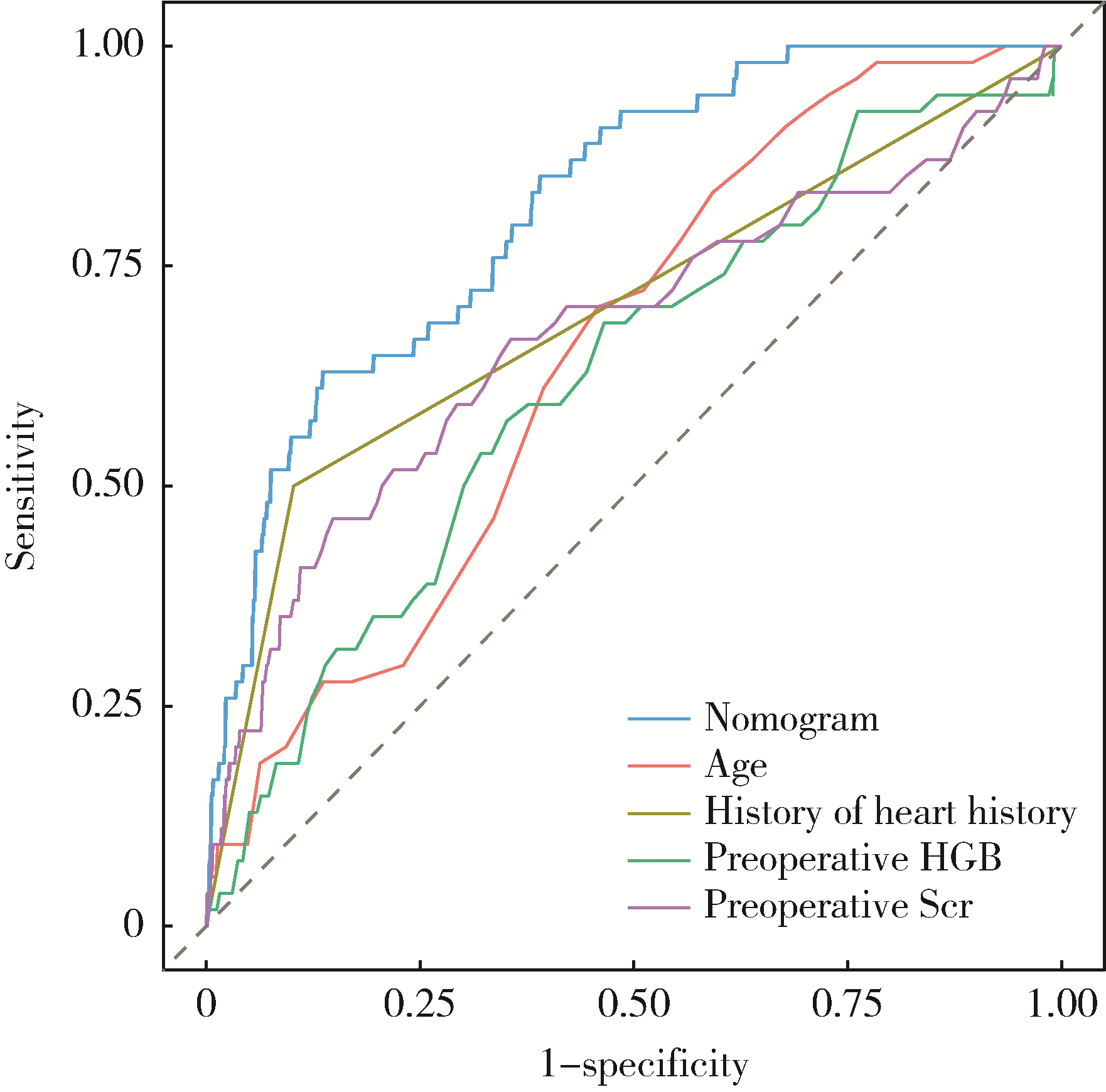
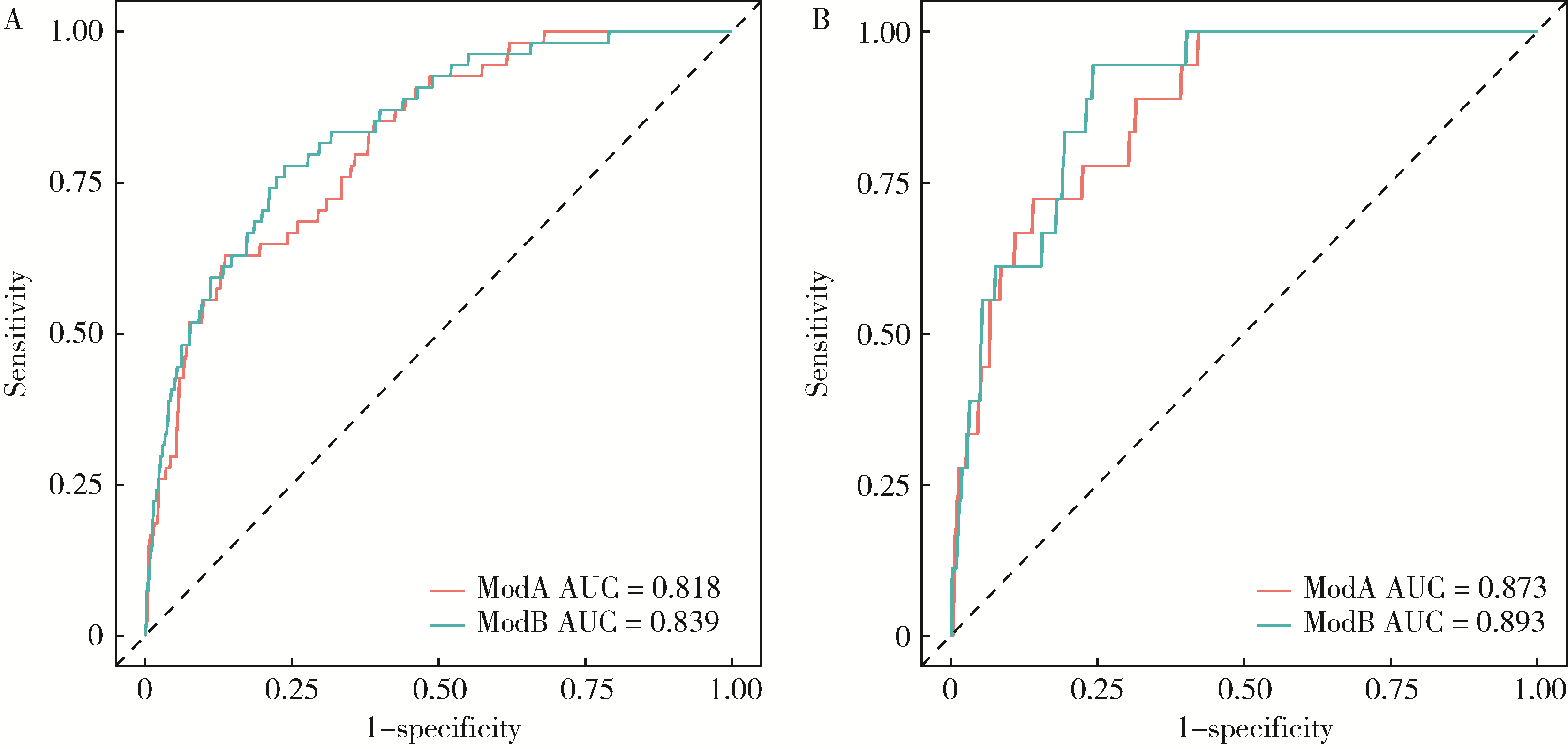
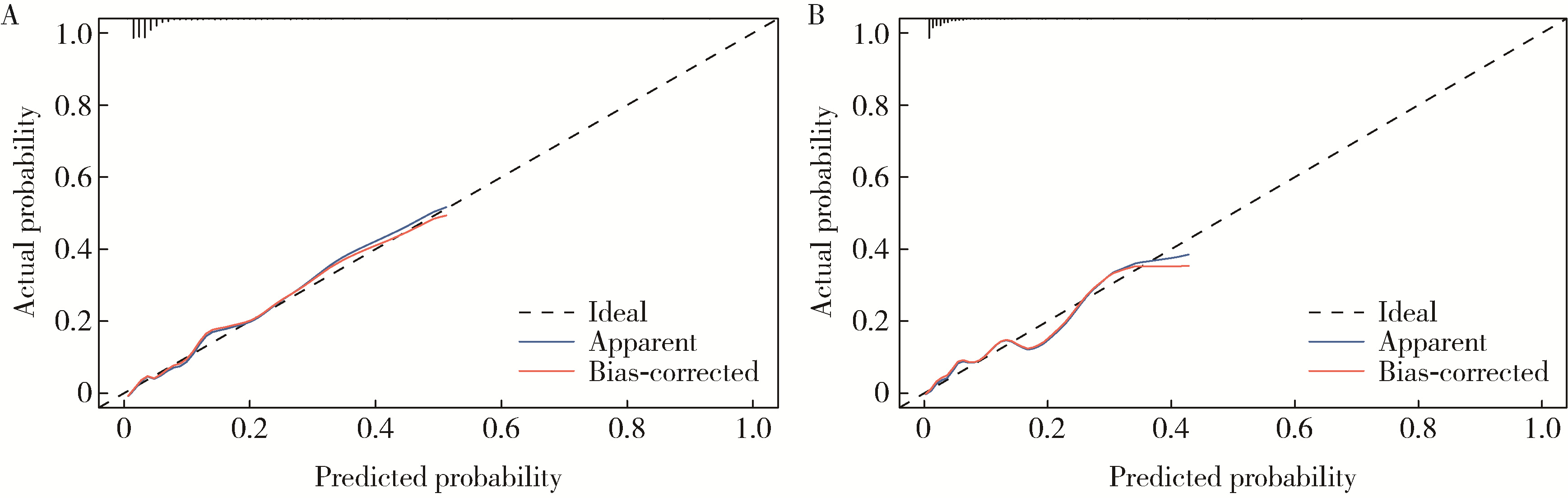
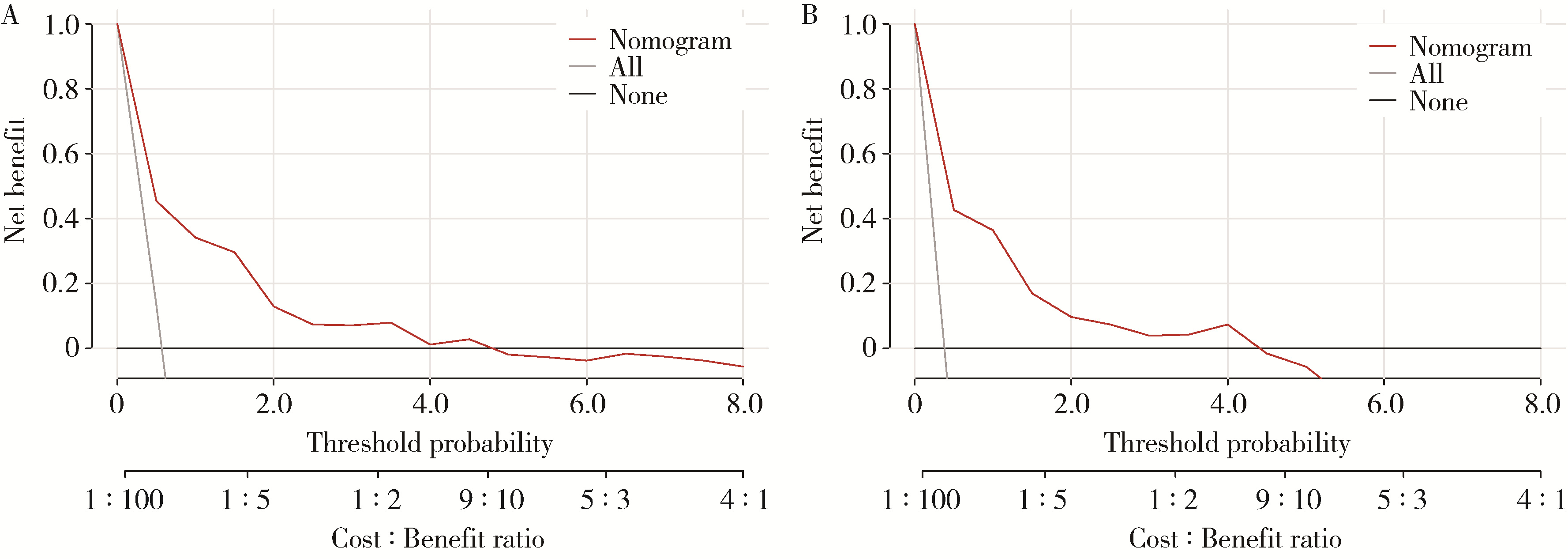
目的: 构建预测老年髋部骨折患者住院期间发生术后心力衰竭(postoperative heart failure, PHF)的列线图预测模型并验证其效能。方法: 采用回顾性队列研究设计,将2015年7月至2023年12月在北京大学第三医院住院接受手术治疗的老年髋部骨折患者(≥65岁)纳入研究,以2015年7月至2021年12月入院的患者为开发队列,以2022年1月至2023年12月入院的患者为验证队列,通过电子病历系统收集患者的临床资料。采用单因素及多因素Logistic回归分析筛选老年髋部骨折患者PHF的预测因素,并通过R语言构建列线图预测模型,采用Bootstrap方法进行内外部验证。分别采用受试者工作特征(receiver operating characteristic, ROC)曲线下面积(area under the curve, AUC)、校准曲线、Hosmer-Lemeshow拟合优度检验、决策曲线分析(decision curve analysis, DCA)评价模型的区分度、校准度和临床适用性。结果: 开发队列共944例患者,其中54例(5.7%)住院期间发生PHF;验证队列共469例患者,其中18例(3.8%)住院期间发生PHF。多因素Logistic回归分析显示,年龄(OR=1.071, 95%CI: 1.019~1.127, P=0.008)、合并心脏病史(OR=5.360, 95%CI: 2.808~10.234, P < 0.001)、术前血红蛋白(OR=0.979, 95%CI: 0.960~0.999, P=0.041)、术前血肌酐(OR=1.007, 95%CI: 1.001~1.013, P=0.015)、髋关节置换术(OR=2.513, 95%CI: 1.259~5.019, P=0.009)和全身麻醉(OR=2.024, 95%CI: 1.053~3.890, P=0.034)是老年髋部骨折患者发生PHF的独立预测因素。基于4个术前预测因素构建列线图预测模型,模型内外部验证的AUC值分别为0.818(95%CI: 0.768~0.868)、0.873(95%CI: 0.805~0.929),显示其预测效能良好。校准曲线和Hosmer-Lemeshow拟合优度检验(内部验证χ2=9.958, P=0.354; 外部验证χ2=5.477, P=0.791)显示模型的预测准确性较高。DCA表明该模型具有一定的临床适用性。结论: 本研究建立了一个简单易用的术前列线图预测模型,可有效预测老年髋部骨折患者发生PHF的风险,有助于早期识别PHF高危患者,优化围手术期管理。
中图分类号:
- R541.6
| 1 |
Roche JJ , Wenn RT , Sahota O , et al. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: Prospective observational cohort study[J]. BMJ, 2005, 331 (7529): 1374.
doi: 10.1136/bmj.38643.663843.55 |
| 2 |
Cullen MW , Gullerud RE , Larson DR , et al. Impact of heart failure on hip fracture outcomes: A population-based study[J]. J Hosp Med, 2011, 6 (9): 507- 512.
doi: 10.1002/jhm.918 |
| 3 | Cordero J , Maldonado A , Iborra S . Surgical delay as a risk factor for wound infection after a hip fracture[J]. Injury, 2016, 47 (Suppl 3): S56- S60. |
| 4 |
You F , Ma C , Sun F , et al. The risk factors of heart failure in elderly patients with hip fracture: What should we care?[J]. BMC Musculoskelet Disord, 2021, 22 (1): 832.
doi: 10.1186/s12891-021-04686-8 |
| 5 |
Tian M , Li W , Wang Y , et al. Risk factors for perioperative acute heart failure in older hip fracture patients and establishment of a nomogram predictive model[J]. J Orthop Surg Res, 2023, 18 (1): 347.
doi: 10.1186/s13018-023-03825-2 |
| 6 |
Brown CA , Boling J , Manson M , et al. Relation between prefracture characteristics and perioperative complications in the elderly adult patient with hip fracture[J]. South Med J, 2012, 105 (6): 306- 310.
doi: 10.1097/SMJ.0b013e3182574bfd |
| 7 |
季日旭, 陈作喜, 吴银生, 等. 老年股骨颈骨折关节置换围术期发生心功能衰竭的危险因素分析[J]. 中华创伤杂志, 2018, 34 (11): 1030- 1034.
doi: 10.3760/cma.j.issn.1001-8050.2018.11.014 |
| 8 |
李长华, 王伟良, 林光锚, 等. 老年股骨转子间骨折患者围手术期发生心力衰竭的相关因素分析[J]. 中华创伤骨科杂志, 2018, 20 (5): 407- 411.
doi: 10.3760/cma.j.issn.1671-7600.2018.05.007 |
| 9 | 梅迎晨, 韩蕊, 陈游洲, 等. 老年髋部骨折围术期心力衰竭的临床特点及危险因素分析[J]. 中国医刊, 2021, 56 (2): 140- 144. |
| 10 |
Gualandro DM , Puelacher C , Chew MS , et al. Acute heart failure after non-cardiac surgery: Incidence, phenotypes, determinants and outcomes[J]. Eur J Heart Fail, 2023, 25 (3): 347- 357.
doi: 10.1002/ejhf.2773 |
| 11 |
McDonagh TA , Metra M , Adamo M , et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Eur Heart J, 2021, 42 (36): 3599- 3726.
doi: 10.1093/eurheartj/ehab368 |
| 12 |
Collins GS , Reitsma JB , Altman DG , et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement[J]. Ann Intern Med, 2015, 162 (1): 55- 63.
doi: 10.7326/M14-0697 |
| 13 |
Hao G , Wang X , Chen Z , et al. Prevalence of heart failure and left ventricular dysfunction in China: The China Hypertension Survey, 2012-2015[J]. Eur J Heart Fail, 2019, 21 (11): 1329- 1337.
doi: 10.1002/ejhf.1629 |
| 14 |
Jiang Y , Luo Y , Li J , et al. Chronic kidney disease and risk of postoperative cardiovascular events in elderly patients receiving hip fracture surgery[J]. Injury, 2022, 53 (2): 596- 602.
doi: 10.1016/j.injury.2021.12.032 |
| 15 |
Liu Y , Liu H , Zhang F . Development and internal validation of a nomogram for predicting postoperative cardiac events in elderly hip fracture patients[J]. Clin Interv Aging, 2023, 18, 2063- 2078.
doi: 10.2147/CIA.S435264 |
| 16 |
Ye CY , Liu A , Xu MY , et al. Arthroplasty versus internal fixation for displaced intracapsular femoral neck fracture in the elderly: Systematic review and meta-analysis of short- and long-term effectiveness[J]. Chin Med J (Engl), 2016, 129 (21): 2630- 2638.
doi: 10.4103/0366-6999.192788 |
| 17 |
Fisher MA , Matthei JD , Obirieze A , et al. Open reduction internal fixation versus hemiarthroplasty versus total hip arthroplasty in the elderly: A review of the National Surgical Quality Improvement Program database[J]. J Surg Res, 2013, 181 (2): 193- 198.
doi: 10.1016/j.jss.2012.07.004 |
| 18 |
Miller AG , Bercik MJ , Ong A . Nonagenarian hip fracture: Treatment and complications[J]. J Trauma Acute Care Surg, 2012, 72 (5): 1411- 1415.
doi: 10.1097/TA.0b013e318246f3f8 |
| 19 |
O'Hara DA , Duff A , Berlin JA , et al. The effect of anesthetic technique on postoperative outcomes in hip fracture repair[J]. Anesthesiology, 2000, 92 (4): 947- 957.
doi: 10.1097/00000542-200004000-00011 |
| 20 |
Chen X , Li H , Li S , et al. Comparison of risk of complication between neuraxial anaesthesia and general anaesthesia for hip fracture surgery: A systematic review and meta-analysis[J]. Int J Surg, 2023, 109 (3): 458- 468.
doi: 10.1097/JS9.0000000000000291 |
| 21 |
Weinstein ER , Boyer RB , White RS , et al. Improved outcomes for spinal versus general anesthesia for hip fracture surgery: A retrospective cohort study of the National Surgical Quality Improvement Program[J]. Reg Anesth Pain Med, 2024, 49 (1): 4- 9.
doi: 10.1136/rapm-2022-104217 |
| 22 |
Chowdary AR , Beale J , Martinez J , et al. Postoperative complications of spinal vs general anesthesia in elderly patients undergoing hip hemiarthroplasty[J]. Arch Orthop Trauma Surg, 2023, 143 (9): 5615- 5621.
doi: 10.1007/s00402-023-04876-0 |
| [1] | 李志存, 吴天俣, 梁磊, 范宇, 孟一森, 张骞. 穿刺活检单针阳性前列腺癌术后病理升级的危险因素分析及列线图模型构建[J]. 北京大学学报(医学版), 2024, 56(5): 896-901. |
| [2] | 周泽臻,邓绍晖,颜野,张帆,郝一昌,葛力源,张洪宪,王国良,张树栋. 非转移性T3a肾细胞癌患者3年肿瘤特异性生存期预测[J]. 北京大学学报(医学版), 2024, 56(4): 673-679. |
| [3] | 张浩宇,石逸雯,潘薇,刘爱萍,孙昕霙,李曼,张旭熙. 基于不同失能水平的老年人照料需求的影响因素[J]. 北京大学学报(医学版), 2024, 56(3): 431-440. |
| [4] | 靖婷,江华,李婷,申倩倩,叶兰,曾银丹,梁文欣,冯罡,司徒文佑,张玉梅. 中国西部5城市中老年人血清25羟基维生素D与握力的相关性[J]. 北京大学学报(医学版), 2024, 56(3): 448-455. |
| [5] | 林郁婷,王华丽,田宇,巩俐彤,常春. 北京市老年人认知功能的影响因素[J]. 北京大学学报(医学版), 2024, 56(3): 456-461. |
| [6] | 汤华萌,袁典琪,王明星,杨晗冰,郭超. 数字融入和健康生活方式对社会经济状况与老年人抑郁关系的序列中介作用[J]. 北京大学学报(医学版), 2024, 56(2): 230-238. |
| [7] | 苏俊琪,王晓颖,孙志强. 舌鳞状细胞癌根治性切除术后患者预后预测列线图的构建与验证[J]. 北京大学学报(医学版), 2024, 56(1): 120-130. |
| [8] | 毛海,张帆,张展奕,颜野,郝一昌,黄毅,马潞林,褚红玲,张树栋. 基于MRI前列腺腺体相关参数构建腹腔镜前列腺癌术后尿失禁的预测模型[J]. 北京大学学报(医学版), 2023, 55(5): 818-824. |
| [9] | 刘慧丽,吕彦函,王晓晓,李民. 老年患者腹腔镜泌尿系肿瘤根治术后慢性疼痛的影响因素[J]. 北京大学学报(医学版), 2023, 55(5): 851-856. |
| [10] | 祝春素,连至炜,崔一民. 中国中老年人抑郁和慢性病的关联[J]. 北京大学学报(医学版), 2023, 55(4): 606-611. |
| [11] | 姜保国,张培训. 老年髋部骨折的围手术期风险评估[J]. 北京大学学报(医学版), 2022, 54(5): 803-809. |
| [12] | 刘光奇,庞元捷,吴疆,吕敏,于孟轲,李雨橦,黄旸木. 2013—2019年流感季北京市住院老年人流感疫苗接种趋势分析[J]. 北京大学学报(医学版), 2022, 54(3): 505-510. |
| [13] | 丁婷婷,曾楚雄,胡丽娜,余明华. 基于癌症基因组图谱数据库结直肠癌免疫细胞浸润预测模型的建立[J]. 北京大学学报(医学版), 2022, 54(2): 203-208. |
| [14] | 刘杰,郭超. 正/负性情绪对中国老年人死亡风险影响的前瞻性队列研究[J]. 北京大学学报(医学版), 2022, 54(2): 255-260. |
| [15] | 李佳,徐钰,王优雅,高占成. 老年流感肺炎的临床特征及D-二聚体与疾病严重程度的相关性[J]. 北京大学学报(医学版), 2022, 54(1): 153-160. |
|
||