北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (6): 1069-1074. doi: 10.19723/j.issn.1671-167X.2024.06.020
使用中文版威斯康星结石生活质量问卷预测肾结石患者生活质量降低的危险因素
王明瑞, 赖金惠, 姬家祥, 唐鑫伟, 胡浩浦, 王起, 许克新, 徐涛, 胡浩*( )
)
- 北京大学人民医院泌尿外科,北京大学应用碎石技术研究所,北京 100044
Risk factors for decreased quality of life in patients with kidney stones predicted by the Chinese version of Wisconsin stone quality of life questionnaire
Mingrui WANG, Jinhui LAI, Jiaxiang JI, Xinwei TANG, Haopu HU, Qi WANG, Kexin XU, Tao XU, Hao HU*( )
)
- Department of Urology, Peking University People' s Hospital, The Institute of Applied Lithotripsy Technology, Peking University, Beijing 100044, China
摘要:
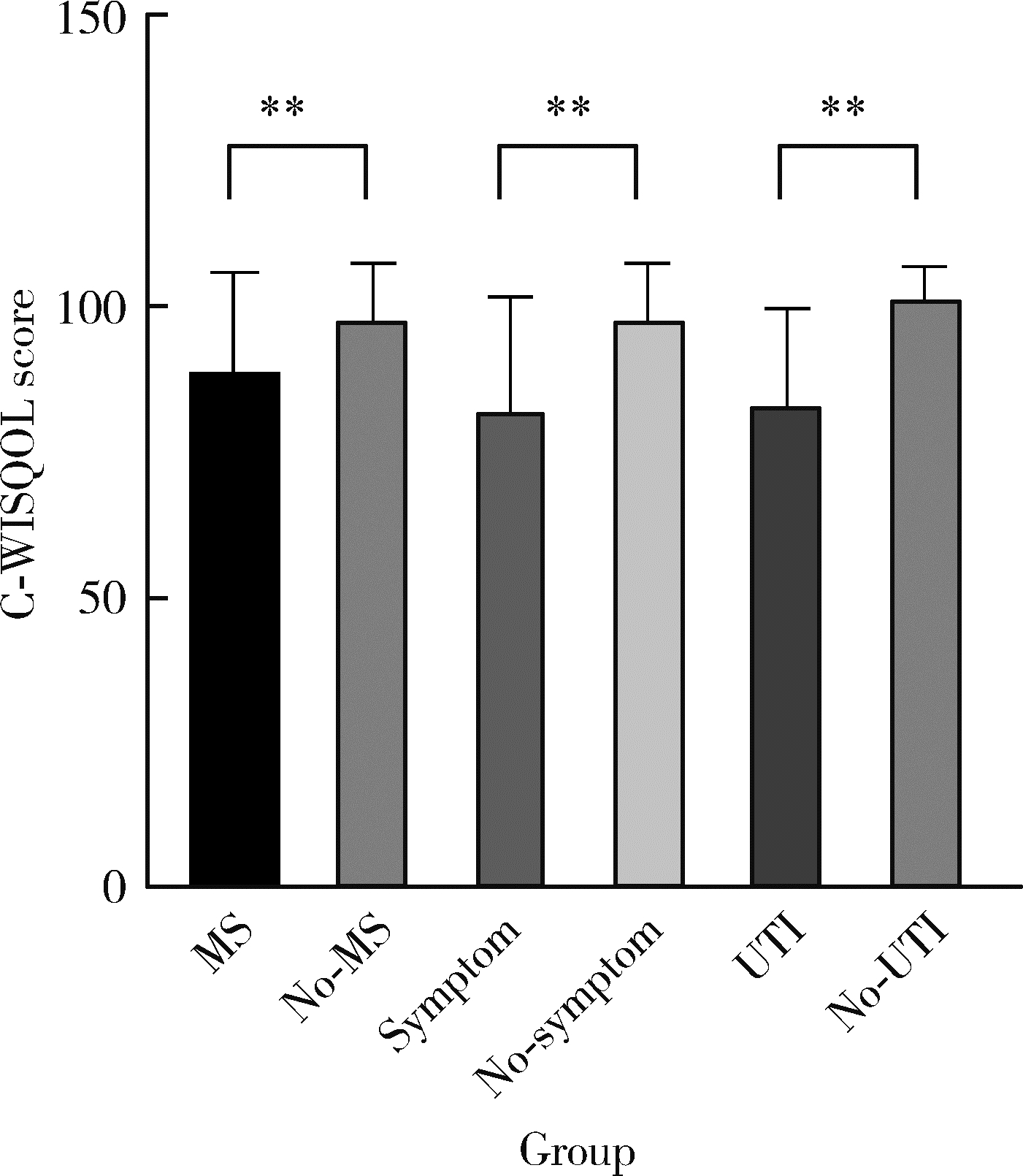
目的: 使用中文版威斯康星结石生活质量问卷(Chinese version of Wisconsin stone quality of life questionnaire,C-WISQOL)评估肾结石患者的健康相关生活质量(health related quality of life,HRQOL),预测导致患者HRQOL降低的危险因素。方法: 自2020年7月至2021年6月前瞻性纳入就诊于北京大学人民医院的肾结石患者,入组标准为18~80岁有足够汉语基础的肾结石患者,排除标准包括体内留置输尿管支架管的患者以及患有恶性肿瘤、脓毒症等的患者。收集患者的人口统计学资料和肾结石相关的临床资料,记录患者填写的C-WISQOL问卷和健康调查简表(short form 36 health survey, SF-36)。C-WISQOL包括四个维度(domain, D):情感影响(D1)、社会影响(D2)、结石相关影响(D3)和活力影响(D4)。使用Cronbach’ s α系数验证C-WISQOL的内部一致性,使用Spearman’ s rho系数验证C-WISQOL和SF-36之间的校标关联效度,使用验证性因子分析验证C-WISQOL的结构效度、聚合效度和区分效度,使用单因素和多因素分析探讨导致肾结石患者HRQOL下降的危险因素。结果: 共纳入307例肾结石患者,其中212例(69.1%)为男性,平均年龄(51.9±13.5)岁,平均体重指数(body mass index,BMI) (25.4±3.6) kg/m2,160例(52.1%)患者合并代谢综合征(metabolic syndrome, MS),202例(65.8%)有既往结石病史,217例(70.7%)有结石相关症状,53例(17.3%)为双侧肾结石,82例(26.7%)合并输尿管结石,199例(64.8%)伴有肾积水,78例(25.4%)伴有肾功能不全,168例(54.7%)合并泌尿系感染(urinary tract infection, UTI),肾结石的平均直径为(15.6±5.9) mm。所有患者C-WISQOL问卷的平均总分为(94.9±13.7) 分,D1为(27.2±4.2) 分,D2为(23.8±3.7) 分,D3为(27.0±3.6) 分,D4为(10.1±1.9) 分。C-WISQOL问卷总分的Cronbach’ s α系数为0.968,四个维度为0.860~0.898。C-WISQOL和SF-36问卷总分相关性的Spearman’ s rho系数为0.564,维度间相关性为0.684~0.901,表明C-WISQOL有较好的内部一致性和校标关联效度。验证性因子分析显示,C-WISQOL具有较好的结构效度、聚合效度和区分效度。单因素分析显示,合并MS(OR=1.607,P < 0.001)、有结石相关症状(OR=1.268,P < 0.001)、双侧肾结石(OR=1.900,P < 0.001)、合并输尿管结石(OR=1.018,P < 0.001)、伴有肾积水(OR=1.685,P < 0.001)、伴有UTI(OR=1.275,P < 0.001)是肾结石患者HRQOL降低的危险因素;多因素分析表明,合并MS(OR=1.475,P < 0.001)、合并输尿管结石(OR=1.546,P=0.043)、伴有UTI(OR=1.646,P=0.005)是肾结石患者HRQOL下降的独立危险因素。t检验结果显示,无MS、结石相关症状和UTI患者的C-WISQOL得分均显著高于合并相关危险因素组(P < 0.001)。结论: C-WISQOL问卷可用于评估肾结石患者的HRQOL,具有较好的可靠性。合并MS、结石相关症状和UTI是肾结石患者HRQOL降低的独立危险因素。
中图分类号:
- R692.4
| 1 |
Thongprayoon C , Krambeck AE , Rule AD .Determining the true burden of kidney stone disease[J].Nat Rev Nephrol,2020,16(12):736-746.
doi: 10.1038/s41581-020-0320-7 |
| 2 |
Zeng G , Mai Z , Xia S , et al.Prevalence of kidney stones in China: An ultrasonography based cross-sectional study[J].BJU Int,2017,120(1):109-116.
doi: 10.1111/bju.13828 |
| 3 | Khan SR , Pearle MS , Robertson WG , et al.Kidney stones[J].Nat Rev Dis Primers,2016,25,16008. |
| 4 |
Streeper NM , Galida M , Boltz S , et al.Is stone-free status after surgical intervention for kidney stones associated with better health-related quality of life? A multicenter study from the North American Stone Quality of Life Consortium[J].Urology,2021,148,77-82.
doi: 10.1016/j.urology.2020.09.058 |
| 5 | Arafa MA , Rabah DM .Study of quality of life and its determinants in patients after urinary stone fragmentation[J].Health Qual Life Outcomes,2010,19,119. |
| 6 |
Penniston KL , Nakada SY .Development of an instrument to assess the health related quality of life of kidney stone formers[J].J Urol,2013,189(3):921-930.
doi: 10.1016/j.juro.2012.08.247 |
| 7 |
Penniston KL , Antonelli JA , Viprakasit DP , et al.Validation and reliability of the wisconsin stone quality of life questionnaire[J].J Urol,2017,197(5):1280-1288.
doi: 10.1016/j.juro.2016.11.097 |
| 8 | 茅亦馨, 张子君, 潘姝丞, 等.威斯康星州肾结石生活质量量表的汉化及信效度检验[J].护理与康复,2019,18(10):12-17. |
| 9 |
Haraldstad K , Wahl A , Andenes R , et al.A systematic review of quality of life research in medicine and health sciences[J].Qual Life Res,2019,28(10):2641-2650.
doi: 10.1007/s11136-019-02214-9 |
| 10 |
Patel N , Brown RD , Sarkissian C , et al.Quality of life and urolithiasis: The patient-reported outcomes measurement information system (PROMIS)[J].Int Braz J Urol,2017,43(5):880-886.
doi: 10.1590/s1677-5538.ibju.2016.0649 |
| 11 |
Bryant M , Angell J , Tu H , et al.Health related quality of life for stone formers[J].J Urol,2012,188(2):436-440.
doi: 10.1016/j.juro.2012.04.015 |
| 12 |
Ragab M , Baldin N , Collie J , et al.Qualitative exploration of the renal stone patients ' experience and development of the renal stone-specific patient-reported outcome measure[J].BJU Int,2020,125(1):123-132.
doi: 10.1111/bju.14873 |
| 13 |
Tran MGB , Sut MK , Collie J , et al.Development of a disease-specific ureteral calculus patient reported outcome measurement instrument[J].J Endourol,2018,32(6):548-558.
doi: 10.1089/end.2017.0795 |
| 14 |
Okada T , Hamamoto S , Taguchi K , et al.Validation of the Japanese version of the Wisconsin stone quality of life questionnaire: Results from SMART Study Group[J].J Endourol,2021,35(12):1852-1856.
doi: 10.1089/end.2021.0292 |
| 15 |
Gottstein M , Pratsinis M , Güsewell S , et al.The German linguistic validation of the Wisconsin stone quality of life questionnaire (WisQoL)[J].World J Urol,2021,39(6):2163-2168.
doi: 10.1007/s00345-020-03405-7 |
| 16 | Atalay HA , ülker V , Canat L , et al.Validation of the Turkish version of the Wisconsin stone-quality of life questionnaire[J].Turk J Urol,2018,45(2):118-123. |
| 17 |
Lim JRZ , Scotland KB , Bechis SK , et al.Metabolic syndrome negatively impacts stone-specific quality of life[J].J Endourol,2020,34(11):1203-1208.
doi: 10.1089/end.2020.0247 |
| 18 |
Kohjimoto Y , Sasaki Y , Iguchi M , et al.Association of metabolic syndrome traits and severity of kidney stones: Results from a nationwide survey on urolithiasis in Japan[J].Am J Kidney Dis,2013,61(6):923-929.
doi: 10.1053/j.ajkd.2012.12.028 |
| 19 | Streeper NM , Wertheim ML , Nakada SY , et al.Cystine stone formers have impaired health-related quality of life compared with noncystine stone formers: A case-referent study piloting the Wisconsin stone quality of life questionnaire among patients with cystine stones[J].J Endourol,2017,31(Suppl1):S48-S53. |
| 20 |
Modersitzki F , Goldfarb DS , Goldstein RL , et al.Assessment of health-related quality of life in patients with cystinuria on tiopronin therapy[J].Urolithiasis,2020,48(4):313-320.
doi: 10.1007/s00240-019-01174-6 |
| 21 |
Wu X , Li Z , Cao J , et al.The association between major complications of immobility during hospitalization and quality of life among bedridden patients: A 3 month prospective multi-center study[J].PLoS One,2018,13(10):e0205729.
doi: 10.1371/journal.pone.0205729 |
| 22 | Lundeen C , Lim JRZ , Scotland KB , et al.What is the relationship of stress to patients ' kidney stone-related quality of life?[J].Can Urol Assoc J,2021,15(5):E256-E260. |
| 23 |
Svihra J Jr , Sopilko I , Svihrova V , et al.Is health-related quality of life of patients after single-use flexible ureteroscopy superior to extracorporeal shock wave lithotripsy? A randomised prospective study[J].Urolithiasis,2021,49(1):73-79.
doi: 10.1007/s00240-020-01224-4 |
| 24 |
Sarica K , Eryildirim B , Sahin C , et al.Emergency management of ureteral stones: Evaluation of two different approaches with an emphasis on patients ' life quality[J].Arch Ital Urol Androl,2016,88(3):201-205.
doi: 10.4081/aiua.2016.3.201 |
| 25 |
Sasmaz MI , Kirpat V .The relationship between the severity of pain and stone size, hydronephrosis and laboratory parameters in renal colic attack[J].Am J Emerg Med,2019,37(11):2107-2110.
doi: 10.1016/j.ajem.2019.06.013 |
| [1] | 李钰锴, 王红彦, 罗靓, 李云, 李春. 抗磷脂抗体在白塞病合并血栓中的临床意义[J]. 北京大学学报(医学版), 2024, 56(6): 1036-1040. |
| [2] | 田杨, 韩永正, 李娇, 王明亚, 曲音音, 房景超, 金辉, 李民, 王军, 徐懋, 王圣林, 郭向阳. 颈椎前路手术后硬膜外血肿的发生率和危险因素[J]. 北京大学学报(医学版), 2024, 56(6): 1058-1064. |
| [3] | 李志存, 吴天俣, 梁磊, 范宇, 孟一森, 张骞. 穿刺活检单针阳性前列腺癌术后病理升级的危险因素分析及列线图模型构建[J]. 北京大学学报(医学版), 2024, 56(5): 896-901. |
| [4] | 颜野,李小龙,夏海缀,朱学华,张羽婷,张帆,刘可,刘承,马潞林. 前列腺癌根治术后远期膀胱过度活动症的危险因素[J]. 北京大学学报(医学版), 2024, 56(4): 589-593. |
| [5] | 王明瑞,刘军,熊六林,于路平,胡浩,许克新,徐涛. 经皮微通道-微电子肾镜-微超声探针碎石术治疗1.5~2.5 cm肾结石的疗效和安全性[J]. 北京大学学报(医学版), 2024, 56(4): 605-609. |
| [6] | 郑生旗,花天池,殷桂草,张伟,姚曳,李一帆. 甘油三酯葡萄糖指数与男性肾结石风险的关联[J]. 北京大学学报(医学版), 2024, 56(4): 610-616. |
| [7] | 陈延,李况蒙,洪锴,张树栋,程建星,郑仲杰,唐文豪,赵连明,张海涛,姜辉,林浩成. 阴茎海绵体注射试验对阴茎血管功能影响的回顾性研究[J]. 北京大学学报(医学版), 2024, 56(4): 680-686. |
| [8] | 庞博,郭桐君,陈曦,郭华棋,石嘉章,陈娟,王欣梅,李耀妍,单安琪,余恒意,黄婧,汤乃军,王艳,郭新彪,李国星,吴少伟. 天津与上海35岁以上人群氮氧化物个体暴露水平及其影响因素[J]. 北京大学学报(医学版), 2024, 56(4): 700-707. |
| [9] | 和静,房中则,杨颖,刘静,马文瑶,霍勇,高炜,武阳丰,谢高强. 血浆中脂质代谢分子与颈动脉粥样硬化斑块、传统心血管危险因素及膳食因素的关系[J]. 北京大学学报(医学版), 2024, 56(4): 722-728. |
| [10] | 蔡珊,张依航,陈子玥,刘云飞,党佳佳,师嫡,李佳欣,黄天彧,马军,宋逸. 北京市中小学生身体活动时间现状及影响因素的路径[J]. 北京大学学报(医学版), 2024, 56(3): 403-410. |
| [11] | 张祖洪,陈天娇,马军. 中小学生青春发动时相与心血管代谢危险因素的相关性[J]. 北京大学学报(医学版), 2024, 56(3): 418-423. |
| [12] | 林郁婷,王华丽,田宇,巩俐彤,常春. 北京市老年人认知功能的影响因素[J]. 北京大学学报(医学版), 2024, 56(3): 456-461. |
| [13] | 朱金荣,赵亚娜,黄巍,赵微微,王悦,王松,苏春燕. 感染新型冠状病毒的血液透析患者的临床特征[J]. 北京大学学报(医学版), 2024, 56(2): 267-272. |
| [14] | 赖展鸿,李嘉辰,贠泽霖,张永刚,张昊,邢晓燕,邵苗,金月波,王乃迪,李依敏,李玉慧,栗占国. 特发性炎性肌病完全临床应答相关因素的单中心真实世界研究[J]. 北京大学学报(医学版), 2024, 56(2): 284-292. |
| [15] | 司筱芊,赵秀娟,朱凤雪,王天兵. 创伤出血性休克后急性呼吸窘迫综合征的危险因素[J]. 北京大学学报(医学版), 2024, 56(2): 307-312. |
|
||