北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (2): 279-285. doi: 10.19723/j.issn.1671-167X.2021.02.008
慢性踝关节不稳患者足底压力特征及相关因素分析
侯宗辰1,敖英芳1,胡跃林1,焦晨1,郭秦炜1,黄红拾1,任爽1,张思1,谢兴1,陈临新1,赵峰1,皮彦斌1,李楠2,江东1,Δ( )
)
- 1.运动医学科, 北京大学第三医院北京 100191
2.临床流行病学研究中心, 北京大学第三医院 北京 100191
Characteristics and related factors of plantar pressure in the chronic ankle instability individuals
HOU Zong-chen1,AO Ying-fang1,HU Yue-lin1,JIAO Chen1,GUO Qin-wei1,HUANG Hong-shi1,REN Shuang1,ZHANG Si1,XIE Xing1,CHEN Lin-xin1,ZHAO Feng1,PI Yan-bin1,LI Nan2,JIANG Dong1,Δ( )
)
- 1. Institute of Sports Medicine, Peking University Third Hospital, Beijing 100191, China
2. Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing 100191, China
摘要:
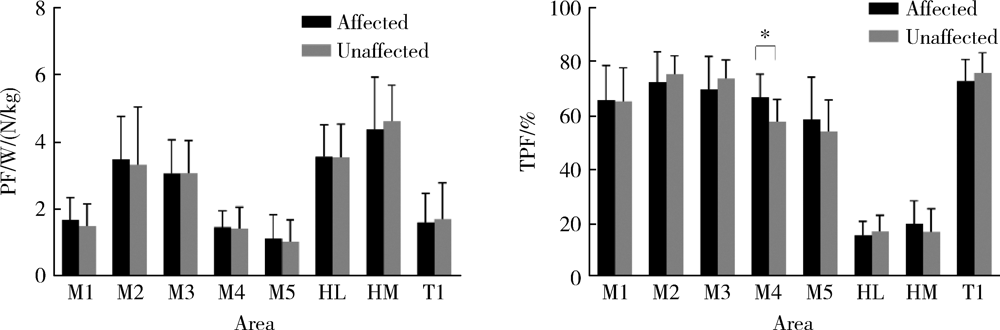
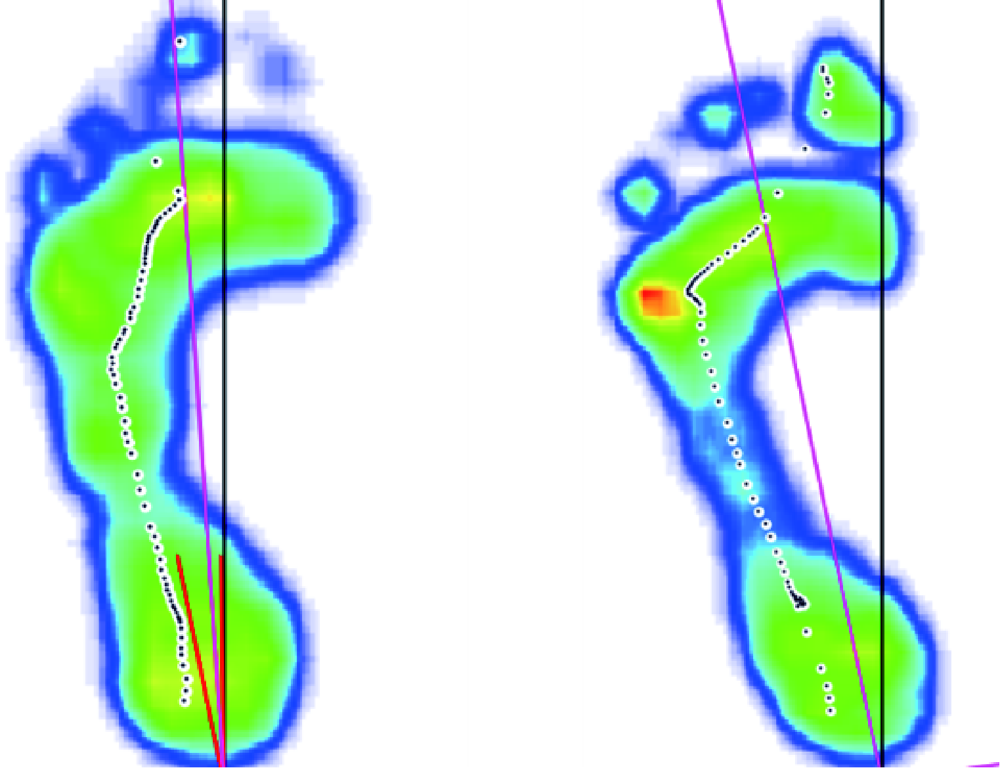
目的: 探讨慢性踝关节不稳(chronic ankle instability,CAI)患者在步行与单足支撑时的足底压力分布特点及其相关因素。方法: 纳入75例CAI患者及40例正常人,对步行及单足站立时的足底压力参数进行对比分析,测量指标为足底每个区域的压强峰值、达峰时间、边界时间(time to boundary,TTB)和压力中心(center of pressure,COP)偏移速度等系列指标。评估CAI患、健侧差异以及与正常对照组的差异,并分析存在差异的足底压力指标与患者年龄、性别、侧别、体重指数、Beighton评分的相关性。结果: CAI患者患、健侧步行时均化峰值压力差异无统计学意义,但是与正常人相比,患侧的第一跖骨(t=2.99,P=0.02)和第二跖骨(t=2.09,P=0.01)、双侧的足跟内侧(患侧t=2.33,P=0.01;健侧t=3.74,P=0.02)和足趾区峰值压力(患侧t=2.23,P=0.01;健侧t=3.28,P=0.02)较小,患侧的第五跖骨区域(t=-3.86,P=0.03)的均化峰值压力较大,且患侧第四跖骨达峰时间较晚(t=3.33,P=0.01)。患侧的内外侧TTB最小值(t=-2.67,P=0.03)、极小值的平均值(t=-3.54,P=0.02)和标准差(t=-2.86,P=0.04)均明显小于健侧,与正常人相比,TTB系列与压力中心系列指标提示患、健侧在内外向和前后向均存在明显的稳定性缺陷(P<0.05)。女性、Beighton评分高的CAI患者内外向稳定性缺陷更明显(P<0.05)。结论: CAI患者在平地步行时患、健侧的足底压力分布特征与正常人存在明显差异,患侧足底COP明显向足外侧偏移。单足支撑时,患侧前后向及双侧的内外向姿势控制稳定性均明显弱于正常人,女性及伴有全身韧带松弛症的CAI患者内外向稳定性缺陷更明显。
中图分类号:
- R648
| [1] |
Doherty C, Bleakley C, Hertel J, et al. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: A prospective cohort analysis[J]. Am J Sports Med, 2016,44(4):995-1003.
pmid: 26912285 |
| [2] |
Nanbancha A, Tretriluxana J, Limroongreungrat W, et al. Decreased supraspinal control and neuromuscular function controlling the ankle joint in athletes with chronic ankle instability[J]. Eur J Appl Physiol, 2019,119(9):2041-2052.
pmid: 31321512 |
| [3] |
Herb CC, Grossman K, Feger MA, et al. Lower extremity biomechanics during a drop-vertical jump in participants with or without chronic ankle instability[J]. J Athl Train, 2018,53(4):364-371.
pmid: 29667844 |
| [4] |
Webster KA, Pietrosimone BG, Gribble PA. Muscle activation during landing before and after fatigue in individuals with or without chronic ankle instability[J]. J Athl Train, 2016,51(8):629-636.
pmid: 27626836 |
| [5] | 侯宗辰, 江东, 胡跃林. 足底压力分析在慢性踝关节不稳诊疗中的研究进展[J]. 中国微创外科杂志, 2019,19(2):186-189. |
| [6] | Koldenhoven RM, Feger MA, Fraser JJ, et al. Surface electromyography and plantar pressure during walking in young adults with chronic ankle instability[J]. Knee Surg, Sports Traumatol, Arthrosc, 2016,24(4):1060-1070. |
| [7] | Mineta S, Inami T, Mariano R, et al. High lateral plantar pressure is related to an increased tibialis anterior/fibularis longus activity ratio in patients with recurrent lateral ankle sprain[J]. Open Access J Sports Med, 2017(8):123-131. |
| [8] |
Hertel J, Olmsted-Kramer LC. Deficits in time-to-boundary mea-sures of postural control with chronic ankle instability[J]. Gait & Posture, 2007,25(1):33-39.
doi: 10.1016/j.gaitpost.2005.12.009 pmid: 16446093 |
| [9] |
Nyska M, Amir H, Porath A, et al. Radiological assessment of a modified anterior drawer test of the ankle[J]. Foot Ankle, 1992,13(7):400-403.
doi: 10.1177/107110079201300707 pmid: 1427531 |
| [10] | 张冉, 胡志伟, 于惠贤, 等. 功能性踝关节不稳患者动态足底压力分布及平衡特征研究[J]. 足踝外科电子杂志, 2016,3(4):14-18. |
| [11] | 李灿杨, 张宏宁. 原发性踝关节骨性关节炎与慢性踝关节不稳的足底压力特征分析[J]. 齐齐哈尔医学院学报, 2019,40(19):2434-2436. |
| [12] |
Becker HP, Rosenbaum D, Claes L, et al. Dynamic pedography for assessing functional ankle joint instability[J]. Unfallchirurg, 1997,100(2):133-139.
pmid: 9157562 |
| [13] |
Lee JH, Lee SH, Choi GW, et al. Individuals with recurrent ankle sprain demonstrate postural instability and neuromuscular control deficits in unaffected side[J]. Knee Surg Sports Traumatol Arthrosc, 2020,28(1):184-192.
doi: 10.1007/s00167-018-5190-1 pmid: 30291398 |
| [14] |
Terada M, Beard M, Carey S, et al. Nonlinear dynamic measures for evaluating postural control in individuals with and without chronic ankle instability[J]. Motor Control, 2019,23(2):243-261.
doi: 10.1123/mc.2017-0001 pmid: 30318988 |
| [15] |
Powden CJ, Hoch JM, Jamali BE, et al. A 4-week multimodal intervention for individuals with chronic ankle instability: Examination of disease-oriented and patient-oriented outcomes[J]. J Athl Train, 2019,54(4):384-396.
pmid: 30589387 |
| [16] |
Mckeon PO, Wikstrom EA. The effect of sensory-targeted ankle rehabilitation strategies on single-leg center of pressure elements in those with chronic ankle instability: A randomized clinical trial[J]. J Sci Med Sport, 2019,22(3):288-293.
pmid: 30244979 |
| [17] | Nigg BM, G KE, Federolf P, et al. Gender differences in lower extremity gait biomechanics during walking using an unstable shoe[J]. Clin Biomech (Bristol, Avon), 2010,25(10):1047-1052. |
| [18] | Mckeon PO, Hertel J. Spatiotemporal postural control deficits are present in those with chronic ankle instability[J]. BMC Musculoskelet Disord, 2008(9):76. |
| [19] |
Russek LN, Errico DM. Prevalence, injury rate and, symptom frequency in generalized joint laxity and joint hypermobility syndrome in a “healthy” college population[J]. Clin Rheumatol, 2016,35(4):1029-1039.
doi: 10.1007/s10067-015-2951-9 pmid: 25930211 |
| [20] |
Wolf JM, Cameron KL, Owens BD. Impact of joint laxity and hypermobility on the musculoskeletal system[J]. J Am Acad Orthop Surg, 2011,19(8):463-471.
pmid: 21807914 |
| [21] | Brown CN, Ko J, Rosen AB, et al. Individuals with both perceived ankle instability and mechanical laxity demonstrate dynamic postural stability deficits[J]. Clin Biomech (Bristol, Avon), 2015,30(10):1170-1174. |
| [1] | 李文菁,张保宙,李恒,赖良鹏,杜辉,孙宁,龚晓峰,李莹,王岩,武勇. 胫距跟融合治疗终末期踝和后足病变的中短期临床结果[J]. 北京大学学报(医学版), 2024, 56(2): 299-306. |
| [2] | 熊士凯,史尉利,王安鸿,谢兴,郭秦炜. 腓骨远端撕脱骨折的影像学诊断:踝关节X线与CT三维重建的比较[J]. 北京大学学报(医学版), 2023, 55(1): 156-159. |
| [3] | 敖明昕,李学民,于媛媛,时会娟,黄红拾,敖英芳,王薇. 视觉重建对老年人行走动态足底压力的影响[J]. 北京大学学报(医学版), 2021, 53(5): 907-914. |
| [4] | 邵振兴,宋庆法,赵宇晴,崔国庆. 一种结合线袢固定的关节镜下“嵌入式”喙突移位术:手术技术及术后影像学分析[J]. 北京大学学报(医学版), 2021, 53(5): 896-901. |
| [5] | 蒋艳芳,王健,王永健,刘佳,裴殷,刘晓鹏,敖英芳,马勇. 前交叉韧带翻修重建术后中长期临床疗效及影响因素[J]. 北京大学学报(医学版), 2021, 53(5): 857-863. |
| [6] | 江东,胡跃林,焦晨,郭秦炜,谢兴,陈临新,赵峰,皮彦斌. 慢性踝关节不稳合并后踝撞击同期手术中长期疗效及影响因素分析[J]. 北京大学学报(医学版), 2019, 51(3): 505-509. |
| [7] | 王荣丽,周志浩,席宇诚,王启宁,王宁华,黄真. 机器人辅助脑瘫儿童踝关节康复临床初步研究[J]. 北京大学学报(医学版), 2018, 50(2): 207-212. |
| [8] | 荣艳波,田光磊,陈山林. 深层桡尺远侧韧带对桡尺远侧关节稳定作用的生物力学研究[J]. 北京大学学报(医学版), 2017, 49(3): 518-521. |
| [9] | 姬洪全,周方,田耘,张志山,郭琰,吕扬,杨钟玮,侯国进. 手术治疗Maisonneuve骨折失误1例报告[J]. 北京大学学报(医学版), 2017, 49(2): 354-356. |
| [10] | 龚晓峰,吕艳伟,王金辉,王岩,武勇,王满宜. 踝关节CT与踝关节骨折分型的相关性研究[J]. 北京大学学报(医学版), 2017, 49(2): 281-285. |
| [11] | 王子昀,吴新宝. 手术复位不良导致的腓骨前脱位1例[J]. 北京大学学报(医学版), 2016, 48(2): 361-365. |
| [12] | 张辉,刘心,洪雷,耿向苏,冯华. 全关节镜下腘肌腱重建与切开腘腓韧带重建治疗膝关节后外旋转不稳定的对比[J]. 北京大学学报(医学版), 2016, 48(2): 237-243. |
| [13] | 张子安,吴新宝,王满宜. 踝关节骨折合并脱位急诊手术与择期手术的结果对比[J]. 北京大学学报(医学版), 2015, 47(5): 791-795. |
| [14] | 吴关, 姜春岩, 鲁谊, 朱以明, 李奉龙, 李旭. 改良关节镜下喙突移位Latarjet手术治疗肩关节前方不稳定[J]. 北京大学学报(医学版), 2015, 47(2): 321-325. |
| [15] | 徐海林,徐雷,张培训,王天兵,付中国,张殿英,姜保国. 踝关节三角韧带损伤的手术治疗[J]. 北京大学学报(医学版), 2013, 45(5): 704-707. |
|
||