北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (6): 1134-1140. doi: 10.19723/j.issn.1671-167X.2022.06.013
尿枸橼酸定量检测在原发性痛风患者肾结石诊断中的应用价值
王昱1,张慧敏2,邓雪蓉1,刘伟伟3,陈璐4,赵宁5,张晓慧1,宋志博1,耿研1,季兰岚1,王玉2,张卓莉1,*( )
)
- 1. 北京大学第一医院风湿免疫科,北京 100034
2. 北京大学第一医院肾内科,北京 100034
3. 河北省沧州市渤海新区中捷医院综合内科,河北沧州 061108
4. 北京航空总医院中医科,北京 100012
5. 北京中医药大学附属护国寺中医医院针灸科,北京 100035
Diagnostic values of urinary citrate for kidney stones in patients with primary gout
Yu WANG1,Hui-min ZHANG2,Xue-rong DENG1,Wei-wei LIU3,Lu CHEN4,Ning ZHAO5,Xiao-hui ZHANG1,Zhi-bo SONG1,Yan GENG1,Lan-lan JI1,Yu WANG2,Zhuo-li ZHANG1,*( )
)
- 1. Department of Rheumatology and Immunology, Peking University First Hospital, Beijing 100034, China
2. Department of Nephrology, Peking University First Hospital, Beijing 100034, China
3. Department of Internal General Medicine, Zhongjie Hospital, Cangzhou 061108, Hebei, China
4. Department of Traditional Chinese Medicine, Aviation General Hospital of China Medical University, Beijing 100012, China
5. Department of Acupuncture, Huguosi Traditional Chinese Medicine Hospital affiliated to Beijing University of Chinese Medicine, Beijing 100035, China
摘要:
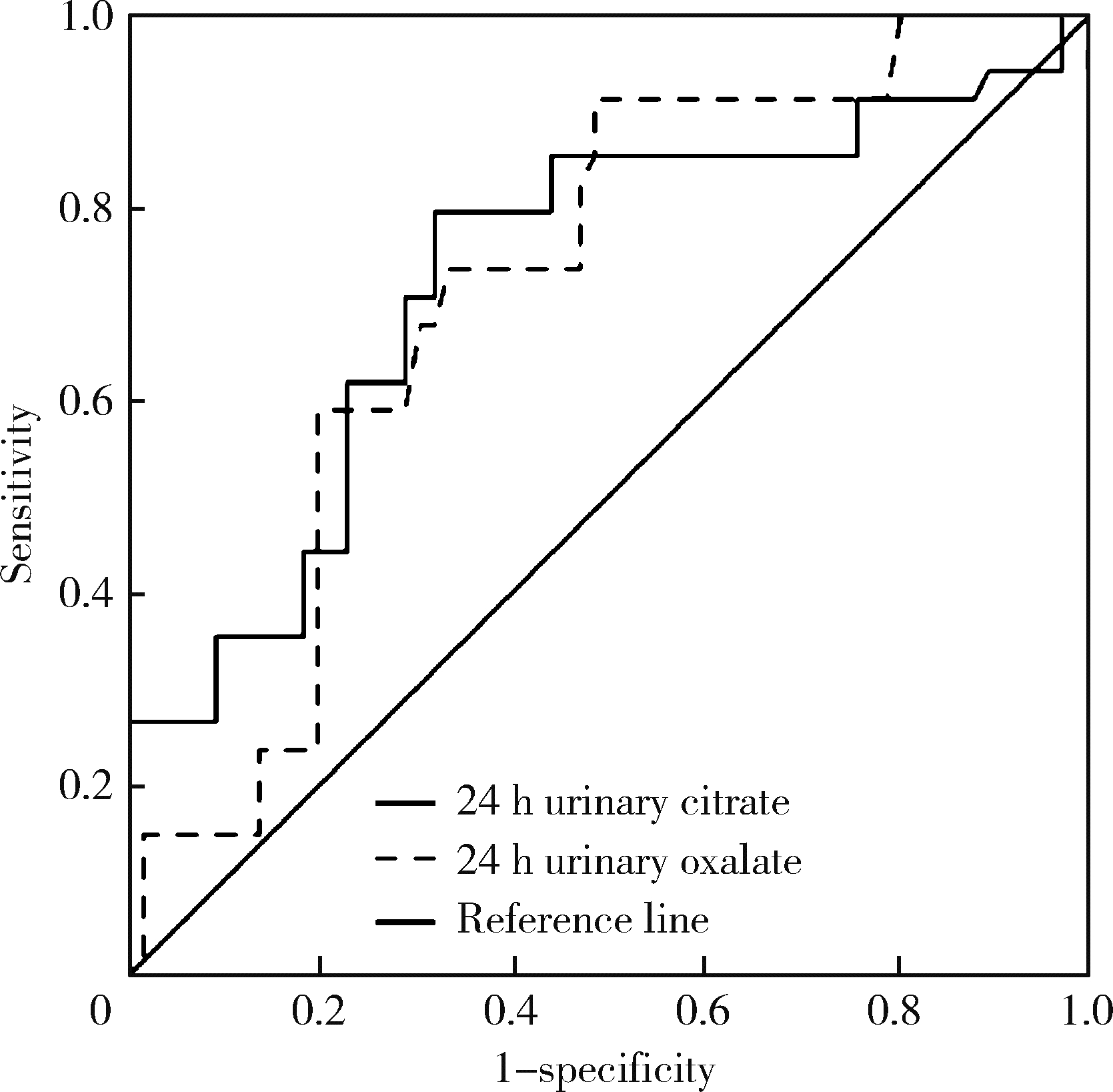
目的: 分析原发性痛风患者24 h尿液离子含量及其与肾结石的关系,探讨其在痛风合并肾结石诊断中的价值。方法: 回顾性分析2020年1月至2021年5月在北京大学第一医院风湿免疫科门诊连续就诊且资料完整的痛风患者,根据临床和超声资料,分析肾结石与尿液离子成分的相关性以及肾结石形成的危险因素。进一步以双能CT证实的肾尿酸盐结石为金标准,探讨尿液离子异常对于痛风合并肾尿酸盐结石的诊断价值。结果: 100例患者中80例超声发现下肢关节尿酸盐晶体沉积,61例超声发现肾结石,34例双能CT检查证实为尿酸盐结石。与超声检查无肾结石组患者相比,肾结石组的痛风病程更长[(48.7±26.6)个月vs. (84.0±30.6)个月,P=0.01],24 h尿草酸总量更高[(20.1±9.6) mg vs. (28.6±20.7) mg,P=0.001],24 h尿枸橼酸总量更低[(506.3±315.4) mg vs. (355.7±219.6) mg,P=0.001]。与双能CT无肾结石组患者相比,肾尿酸盐结石组痛风病程更长[(49.1±28.4)个月vs. (108.3±72.2)个月,P=0.001],24 h尿草酸总量更高[(23.6±16.9) mg vs. (28.5±18.8) mg,P < 0.05],24 h尿枸橼酸总量更低[(556.0±316.3) mg vs. (391.7±261.2) mg,P < 0.05],平均血尿酸水平及24 h尿尿酸总量更高[(466.2±134.5) μmol/L vs. (517.2±18.1) μmol/L,P < 0.05;(1 518.1±893.4) mg vs. (1 684.2±812.1) mg,P < 0.05]。以病程、既往痛风发作频率、血尿酸、血肌酐及24 h尿草酸、枸橼酸、尿酸为自变量进行Logistic回归分析,结果显示长病程(OR=1.229,95%CI:1.062~1.522,P < 0.05)、高血尿酸(OR=1.137,95%CI:1.001~1.213,P=0.01)、低24 h尿枸橼酸总量(OR=0.821,95%CI:0.659~0.952,P=0.01)为痛风患者超声发现肾结石的危险因素;长病程(OR=1.201,95%CI:1.101~1.437,P=0.005)、高血肌酐(OR=1.145,95%CI:1.001~1.182,P=0.04)、低24 h尿枸橼酸总量(OR=0.837,95%CI:0.739~0.931,P=0.02)为痛风患者出现肾尿酸盐结石的危险因素。结论: 长病程、低24 h尿枸橼酸的痛风患者更容易出现肾结石。
中图分类号:
- R589.7
| 1 |
Wallace SL , Robinson H , Masi AT , et al. Preliminary criteria for the classification of the acute arthritis of primary gout[J]. Arthritis Rheum, 1977, 20 (3): 895- 900.
doi: 10.1002/art.1780200320 |
| 2 |
Filippou G , Pascart T , Iagnocco A . Utility of ultrasound and dual energy CT in crystal disease diagnosis and management[J]. Curr Rheumatol Rep, 2020, 22 (5): 15.
doi: 10.1007/s11926-020-0890-1 |
| 3 |
Skolarikos A , Straub M , Knoll T , et al. Metabolic evaluation and recurrence prevention for urinary stone patients: EAU guidelines[J]. Eur Urol, 2015, 67 (4): 750- 763.
doi: 10.1016/j.eururo.2014.10.029 |
| 4 |
Neogi T , Jansen TL , Dalbeth N , et al. 2015 gout classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative[J]. Ann Rheum Dis, 2015, 74 (10): 1789- 1798.
doi: 10.1136/annrheumdis-2015-208237 |
| 5 |
Gutierrez M , Schmidt WA , Thiele RG , et al. International consensus for ultrasound lesions in gout: Results of Delphi process and web-reliability exercise[J]. Rheumatology (Oxford), 2015, 54 (10): 1797- 1805.
doi: 10.1093/rheumatology/kev112 |
| 6 |
范兵, 王霄英, 邱建星, 等. 能谱CT与常规CT对泌尿系结石CT值的相关性分析[J]. CT理论与应用研究, 2016, 25 (4): 403- 408.
doi: 10.15953/j.1004-4140.2016.25.04.03 |
| 7 |
《泌尿外科杂志(电子版)》编辑部. 泌尿系结石诊治指南解读(一)[J]. 泌尿外科杂志(电子版), 2010, 2 (4): 56- 57.
doi: 10.3969/j.issn.1674-7410.2010.04.017 |
| 8 |
Richette P , Doherty M , Pascual E , et al. 2018 updated European League Against Rheumatism evidence-based recommendations for the diagnosis of gout[J]. Ann Rheum Dis, 2020, 79 (1): 31- 38.
doi: 10.1136/annrheumdis-2019-215315 |
| 9 |
王昱, 陈育青, 张蓓, 等. 原发性痛风患者24 h尿液化学成分分析与尿酸结石形成风险的研究[J]. 中华风湿病学杂志, 2018, 22 (3): 165- 170.
doi: 10.3760/cma.j.issn.1007-7480.2018.03.005 |
| 10 |
Tzelves L , Türk C , Skolarikos A . European Association of Urology urolithiasis guidelines: Where are we going?[J]. Eur Urol Focus, 2021, 7 (1): 34- 38.
doi: 10.1016/j.euf.2020.09.011 |
| 11 |
Pearle MS , Goldfarb DS , Assimos DG , et al. Medical management of kidney stones: AUA guideline[J]. J Urol, 2014, 192 (2): 316- 324.
doi: 10.1016/j.juro.2014.05.006 |
| 12 |
Nestler T , Nestler K , Neisius A , et al. Diagnostic accuracy of third-generation dual-source dual-energy CT: A prospective trial and protocol for clinical implementation[J]. World J Urol, 2019, 37 (4): 735- 741.
doi: 10.1007/s00345-018-2430-4 |
| 13 | 张晓洁, 姜林娣. 痛风患者肾脏结石与关节部位尿酸盐晶体沉积的相关性[J]. 中国临床医学, 2017, 24 (5): 767- 769. |
| 14 |
Siener R , Glatz S , Nicolay C , et al. Prospective study on the efficacy of a selective treatment and risk factors for relapse in recurrent calcium oxalate stone patients[J]. Eur Urol, 2003, 44 (4): 467- 474.
doi: 10.1016/S0302-2838(03)00317-8 |
| 15 |
Mittal A , Tandon S , Singla SK , et al. In vitro inhibition of cal-cium oxalate crystallization and crystal adherence to renal tubular epithelial cells by Terminalia arjuna[J]. Urolithiasis, 2016, 44 (2): 117- 125.
doi: 10.1007/s00240-015-0822-0 |
| 16 | 闫晓煜, 黄志红, 孟胜兰, 等. 24小时尿枸橼酸、草酸定量检测在泌尿系结石诊断中的应用[J]. 标记免疫分析与临床, 2018, 25 (5): 634- 668. |
| 17 |
Smith LH . Diet and hyperoxaluria in the syndrome of idiopathic calcium oxalate urolithiasis[J]. Am J Kidney Dis, 1991, 17 (4): 370- 375.
doi: 10.1016/S0272-6386(12)80625-1 |
| 18 |
Holmes RP , Goodman HO , Assimos DG . Contribution of dietary oxalate to urinary oxalate excretion[J]. Kidney Int, 2001, 59 (1): 270- 276.
doi: 10.1046/j.1523-1755.2001.00488.x |
| 19 |
Robijn S , Hoppe B , Vervaet BA , et al. Hyperoxaluria: A gut-kidney axis?[J]. Kidney Int, 2011, 80 (11): 1146- 1158.
doi: 10.1038/ki.2011.287 |
| 20 |
Taylor EN , Curhan GC . Oxalate intake and the risk for nephroli-thiasis[J]. J Am Soc Nephrol, 2007, 18 (7): 2198- 2204.
doi: 10.1681/ASN.2007020219 |
| 21 |
Curhan GC , Taylor EN . 24 h uric acid excretion and the risk of kidney stones[J]. Kidney Int, 2008, 73 (4): 489- 496.
doi: 10.1038/sj.ki.5002708 |
| 22 |
Kok DJ , Papapoulos SE , Bijvoet OL . Crystal agglomeration is a major element in calcium oxalate urinary stone formation[J]. Kidney Int, 1990, 37 (1): 51- 56.
doi: 10.1038/ki.1990.7 |
| 23 |
Mandel EI , Taylor EN , Curhan GC . Dietary and lifestyle factors and medical conditions associated with urinary citrate excretion[J]. Clin J Am Soc Nephrol, 2013, 8 (6): 901- 908.
doi: 10.2215/CJN.07190712 |
| 24 |
Domrongkitchaiporn S , Stitchantrakul W , Kochakarn W . Causes of hypocitraturia in recurrent calcium stone formers: Focusing on urinary potassium excretion[J]. Am J Kidney Dis, 2006, 48 (4): 546- 554.
doi: 10.1053/j.ajkd.2006.06.008 |
| 25 |
Coe FL , Parks JH , Asplin JR . The pathogenesis and treatment of kidney stones[J]. N Engl J Med, 1992, 327 (16): 1141- 1152.
doi: 10.1056/NEJM199210153271607 |
| 26 |
Ettinger B , Tang A , Citron JT , et al. Randomized trial of allopurinol in the prevention of calcium oxalate calculi[J]. N Engl J Med, 1986, 315 (22): 1386- 1389.
doi: 10.1056/NEJM198611273152204 |
| 27 |
Ferraro PM , Curhan GC , D'Addessi A , et al. Risk of recurrence of idiopathic calcium kidney stones: Analysis of data from the lite-rature[J]. J Nephrol, 2017, 30 (2): 227- 233.
doi: 10.1007/s40620-016-0283-8 |
| 28 |
Levy FL , Adams-Huet B , Pak CY . Ambulatory evaluation of nephrolithiasis: An update of a 1980 protocol[J]. Am J Med, 1995, 98 (1): 50- 59.
doi: 10.1016/S0002-9343(99)80080-1 |
| [1] | 原晋芳, 王新利, 崔蕴璞, 王雪梅. 尿促黄体生成素在女童中枢性性早熟预测中的应用[J]. 北京大学学报(医学版), 2024, 56(5): 788-793. |
| [2] | 管仁珍, 丁士刚, 石岩岩, 薛艳. 含铋剂四联疗法根除幽门螺杆菌的疗效:4 261例患者的真实世界研究[J]. 北京大学学报(医学版), 2024, 56(5): 942-945. |
| [3] | 王明瑞,刘军,熊六林,于路平,胡浩,许克新,徐涛. 经皮微通道-微电子肾镜-微超声探针碎石术治疗1.5~2.5 cm肾结石的疗效和安全性[J]. 北京大学学报(医学版), 2024, 56(4): 605-609. |
| [4] | 郑生旗,花天池,殷桂草,张伟,姚曳,李一帆. 甘油三酯葡萄糖指数与男性肾结石风险的关联[J]. 北京大学学报(医学版), 2024, 56(4): 610-616. |
| [5] | 董泓,王丽敏,王志强,刘彦卿,张晓刚,张明明,刘娟,李振彬. 急性痛风发作的昼夜差异: 一项男性痛风患者的临床研究[J]. 北京大学学报(医学版), 2023, 55(5): 915-922. |
| [6] | 田聪,刘军,杨波,乔佳佳,黄晓波,许清泉. 经皮肾镜取石术中异常肾盂黏膜活检结果分析[J]. 北京大学学报(医学版), 2023, 55(5): 948-952. |
| [7] | 傅强,高冠英,徐雁,林卓华,孙由静,崔立刚. 无症状髋关节前上盂唇撕裂超声与磁共振检查的对比研究[J]. 北京大学学报(医学版), 2023, 55(4): 665-669. |
| [8] | 叶一林,刘恒,潘利平,柴卫兵. 全膝关节置换术后假体周围痛风发作误诊1例[J]. 北京大学学报(医学版), 2023, 55(2): 362-365. |
| [9] | 谢晓炜,李芬,凌光辉,谢希,许素清,陈谊月. 痛风患者健康教育知识知晓度测量问卷的研制及临床应用[J]. 北京大学学报(医学版), 2022, 54(4): 699-704. |
| [10] | 安立哲,熊六林,陈亮,王焕瑞,陈伟男,黄晓波. 腹腔镜肾盂成形术联合肾盂镜超声碎石取石术治疗肾盂输尿管连接部梗阻合并肾结石[J]. 北京大学学报(医学版), 2022, 54(4): 746-750. |
| [11] | 张学武. 痛风关节炎治疗中几个备受关注的问题[J]. 北京大学学报(医学版), 2021, 53(6): 1017-1019. |
| [12] | 邓雪蓉,孙晓莹,张卓莉. 类风湿关节炎患者足踝部体征和超声下病变的一致性[J]. 北京大学学报(医学版), 2021, 53(6): 1037-1042. |
| [13] | 彭喆,丁亚敏,裴林,姚海红,张学武,唐素玫. 痛风患者发生关节及肌腱内晶体沉积的临床特点[J]. 北京大学学报(医学版), 2021, 53(6): 1067-1071. |
| [14] | 王贵红,左婷,李然,左正才. 瑞巴派特在大鼠痛风性关节炎急性发作中的作用[J]. 北京大学学报(医学版), 2021, 53(4): 716-720. |
| [15] | 谢一帆,王昱,邓雪蓉,耿研,季兰岚,张卓莉. 影响双能CT尿酸盐结晶检出率的因素[J]. 北京大学学报(医学版), 2021, 53(2): 261-265. |
|
||