北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (6): 1017-1022. doi: 10.19723/j.issn.1671-167X.2024.06.011
系统性红斑狼疮疾病活动度相关特征分析及评估模型的构建
王红彦1, 李鑫铭2,3, 房柯池2,3, 朱华群1, 贾汝琳1,*( ), 王晶2,3,*(
), 王晶2,3,*( )
)
- 1. 北京大学人民医院风湿免疫科,北京 100044
2. 中国科学院心理研究所,中国科学院心理健康重点实验室,北京 100101
3. 中国科学院大学心理学系,北京 100049
Analysis of characteristics related to the disease activity of systemic lupus erythematosus and construction of an evaluation model
Hongyan WANG1, Xinming LI2,3, Kechi FANG2,3, Huaqun ZHU1, Rulin JIA1,*( ), Jing WANG2,3,*(
), Jing WANG2,3,*( )
)
- 1. Department of Rheumatology and Immunology, Peking University People's Hospital, Beijing 100044, China
2. Institute of Psychology, Chinese Academy of Sciences; Key Laboratory of Mental Health, Chinese Academy of Sciences, Beijing 100101, China
3. Department of Psychology, University of Chinese Academy of Sciences, Beijing 100049, China
摘要:
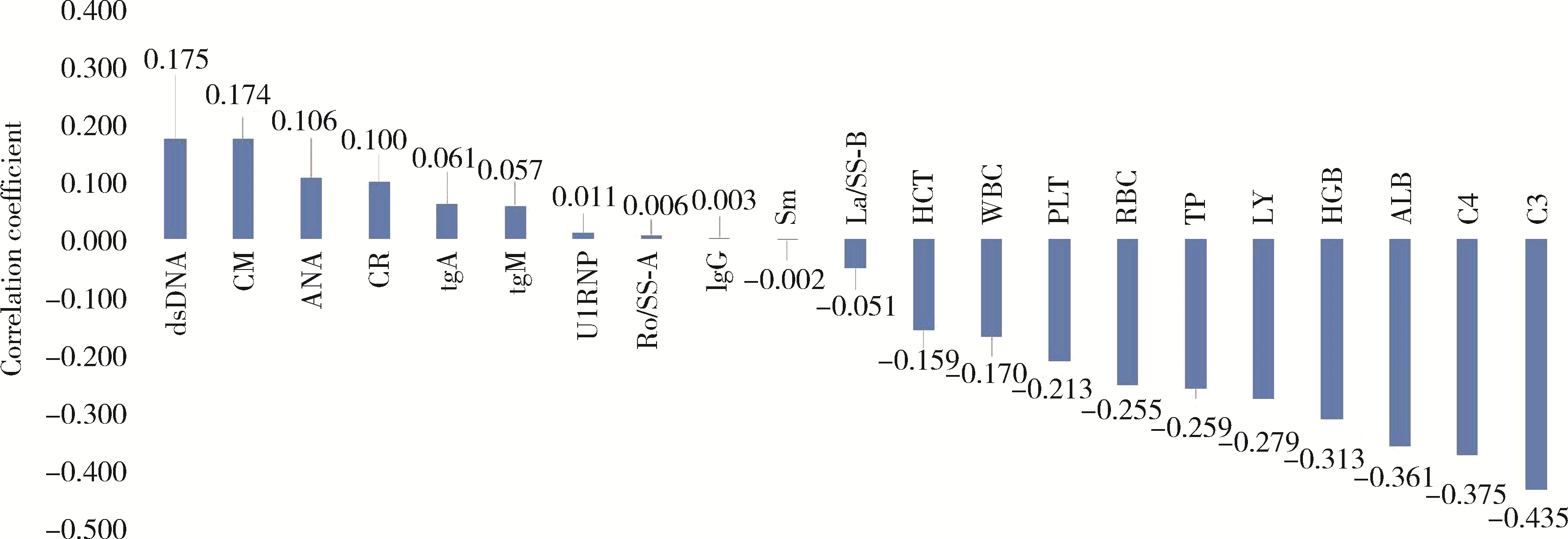
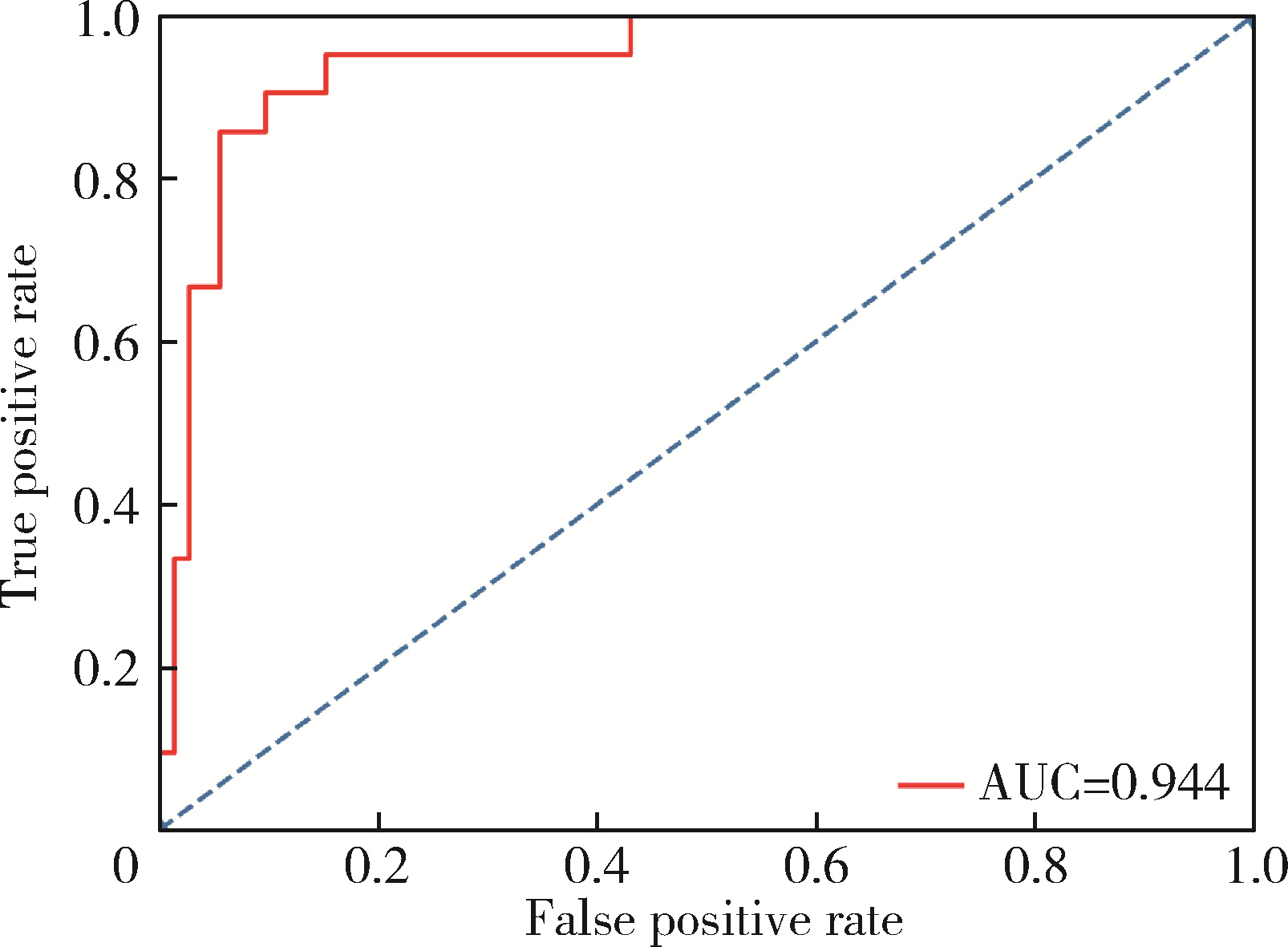
目的: 对系统性红斑狼疮(systemic lupus erythematosus, SLE)患者进行临床分层,分析不同活动度患者的临床特征,并探讨关键临床指标在SLE疾病活动度评估中的应用价值及评估模型的构建。方法: 回顾性分析1995年5月至2014年4月北京大学人民医院确诊的SLE患者临床资料。收集患者的人口学信息、临床表现、实验室检查结果,根据SLE疾病活动度指数2000(systemic lupus erythematosus disease activity index 2000, SLEDAI-2000)将患者分为疾病活动组与无疾病活动组。采用t检验、Mann-Whitney U检验以及χ2检验比较两组间差异,并使用Spearman相关性分析评估疾病活动组中与SLE活动度相关的临床指标。基于统计学分析结果,构建了逻辑回归模型,并对模型性能进行评估。结果: 两组在基本人口学特征上差异无统计学意义。疾病活动组中,抗核抗体(antinuclear antibodies,ANA)及抗双链DNA抗体(anti-double-stranded DNA antibodies,anti-dsDNA)阳性率升高;白细胞计数(white blood cell, WBC)、红细胞计数(red blood cell, RBC)、血红蛋白(hemoglobin, HGB)、淋巴细胞(lymphocytes, LY)、总蛋白(total protein, TP)、白蛋白(albumin, ALB)及补体C3水平显著降低,免疫球蛋白A(immunoglobulin A,IgA)、免疫球蛋白G(immunoglobulin G, IgG)水平明显升高。相关性分析结果显示,血红蛋白、白蛋白、补体C3和补体C4与其他临床指标相比具有更高的相关性指数,其中补体C3与疾病活动度具有一定负相关性。基于12项差异具有统计学意义的指标构建的逻辑回归模型准确率为91.4%,敏感性为94.4%,特异性为81.0%,受试者工作特征曲线(receiver operating characteristic, ROC)的线下面积(area under curve, AUC)为0.944。结论: 全面评估与SLE疾病活动度相关的临床指标,以实验室检查指标为主构建的逻辑回归模型能够较准确地评估SLE患者疾病活动度,为SLE患者的个体化治疗提供参考。
中图分类号:
- R593.2
| 1 |
Barber MRW , Drenkard C , Falasinnu T , et al. Global epidemio-logy of systemic lupus erythematosus[J]. Nat Rev Rheumatol, 2021, 17 (9): 515- 532.
doi: 10.1038/s41584-021-00668-1 |
| 2 |
Schwartz N , Stock AD , Putterman C . Neuropsychiatric lupus: New mechanistic insights and future treatment directions[J]. Nat Rev Rheumatol, 2019, 15 (3): 137- 152.
doi: 10.1038/s41584-018-0156-8 |
| 3 |
Stamm TA , Bauernfeind B , Coenen M , et al. Concepts important to persons with systemic lupus erythematosus and their coverage by standard measures of disease activity and health status[J]. Arthritis Care Res (Hoboken), 2007, 57 (7): 1287- 1295.
doi: 10.1002/art.23013 |
| 4 | Gladman DD , Ibañez D , Urowitz MB , et al. Systemic lupus erythematosus disease activity index 2000[J]. J Rheumatol, 2002, 29 (2): 288- 291. |
| 5 |
Isenberg DA , Rahman A , Allen E , et al. BILAG 2004. Development and initial validation of an updated version of the British Isles Lupus Assessment Group's disease activity index for patients with systemic lupus erythematosus[J]. Rheumatology (Oxford), 2005, 44 (7): 902- 906.
doi: 10.1093/rheumatology/keh624 |
| 6 |
Sutton EJ , Davidson JE , Bruce IN . The systemic lupus international collaborating clinics (SLICC) damage index: A systematic literature review[J]. Semin Arthritis Rheum, 2013, 43 (3): 352- 361.
doi: 10.1016/j.semarthrit.2013.05.003 |
| 7 |
Emamikia S , Oon S , Gomez A , et al. Impact of remission and low disease activity on health-related quality of life in patients with systemic lupus erythematosus[J]. Rheumatology (Oxford), 2022, 61 (12): 4752- 4762.
doi: 10.1093/rheumatology/keac185 |
| 8 |
Wang Y , Han M , Pedigo CE , et al. Chinese herbal medicine for systemic lupus erythematosus: A systematic review and meta-analysis of randomized, placebo-controlled trials[J]. Chin J Integr Med, 2021, 27 (10): 778- 787.
doi: 10.1007/s11655-021-3497-0 |
| 9 |
Chen C , Wang L , Han B , et al. Autoimmune hemolytic anemia in hospitalized patients: 450 patients and their red blood cell transfusions[J]. Medicine (Baltimore), 2020, 99 (2): e18739.
doi: 10.1097/MD.0000000000018739 |
| 10 |
Yin X , Kim K , Suetsugu H , et al. Biological insights into syste-mic lupus erythematosus through an immune cell-specific transcriptome-wide association study[J]. Ann Rheum Dis, 2022, 81 (9): 1273- 1280.
doi: 10.1136/annrheumdis-2022-222345 |
| 11 | Tobón GJ , Izquierdo JH , Cañas CA . B lymphocytes: Development, tolerance, and their role in autoimmunity-focus on systemic lupus erythematosus[J]. Autoimmune Dis, 2013, 2013 (1): 827254. |
| 12 | Wang Y , Xiao S , Xia Y , et al. The therapeutic strategies for SLE by targeting anti-dsDNA antibodies[J]. Clin Rev Allergy Immunol, 2022, 63 (2): 152- 165. |
| 13 |
Qiu W , Yu T , Deng GM . The role of organ-deposited IgG in the pathogenesis of multi-organ and tissue damage in systemic lupus erythematosus[J]. Front Immunol, 2022, 13, 924766.
doi: 10.3389/fimmu.2022.924766 |
| 14 |
Lundtoft C , Sjöwall C , Rantapää-Dahlqvist S , et al. Strong association of combined genetic deficiencies in the classical complement pathway with risk of systemic lupus erythematosus and primary Sjögren' s syndrome[J]. Arthritis Rheumatol, 2022, 74 (11): 1842- 1850.
doi: 10.1002/art.42270 |
| 15 |
Jesus D , Rodrigues M , Matos A , et al. Performance of SLEDAI-2K to detect a clinically meaningful change in SLE disease activity: A 36-month prospective cohort study of 334 patients[J]. Lupus, 2019, 28 (5): 607- 612.
doi: 10.1177/0961203319836717 |
| 16 |
Koo M , Lu MC . Performance of a new instrument for the measurement of systemic lupus erythematosus disease activity: The SLE-DAS[J]. Medicina (Kaunas), 2023, 59 (12): 2097.
doi: 10.3390/medicina59122097 |
| 17 | 王蒙, 韩迪迪, 王力宁, 等. 系统性红斑狼疮两种评分系统对狼疮肾炎活动临床评价的比较[J]. 中华风湿病学杂志, 2016, 20 (6): 391- 395. |
| [1] | 陈丹丹, 李云, 卢情怡, 相晓红, 孙峰, 李英妮, 赵静, 王红彦, 李春. 育龄期系统性红斑狼疮患者卵巢功能的评价及其影响因素[J]. 北京大学学报(医学版), 2024, 56(6): 1023-1028. |
| [2] | 王莉, 高超, 任欢欢, 沈艳平, 黄晓玮, 姚鸿, 韩丹丹. 系统性红斑狼疮患者自我管理能力现状及相关因素分析[J]. 北京大学学报(医学版), 2024, 56(6): 1029-1035. |
| [3] | 柴静, 王钥, 穆荣, 赵金霞. 系统性红斑狼疮累及穹窿柱导致低钠血症1例[J]. 北京大学学报(医学版), 2024, 56(6): 1115-1118. |
| [4] | 王明霞, 丁菱, 王敏, 邹婵娟, 颜丝语, 梁颖文, 王伟佳, 何善智. 双靶点嵌合抗原受体T细胞治疗系统性红斑狼疮患者停药后安全孕产1例[J]. 北京大学学报(医学版), 2024, 56(6): 1119-1125. |
| [5] | 翟佳羽, 赵金霞, 安卓, 刘蕊. 低疾病活动度的中轴型脊柱关节炎患者残留症状评估及其相关因素分析[J]. 北京大学学报(医学版), 2024, 56(6): 987-993. |
| [6] | 武志慧, 胡明智, 赵巧英, 吕凤凤, 张晶莹, 张伟, 王永福, 孙晓林, 王慧. miR-125b-5p修饰脐带间充质干细胞对系统性红斑狼疮的免疫调控机制[J]. 北京大学学报(医学版), 2024, 56(5): 860-867. |
| [7] | 乔佳佳,田聪,黄晓波,刘军. 肾结石合并系统性红斑狼疮行经皮肾镜碎石取石术的安全性和有效性评估[J]. 北京大学学报(医学版), 2024, 56(4): 745-749. |
| [8] | 任立敏,赵楚楚,赵义,周惠琼,张莉芸,王友莲,沈凌汛,范文强,李洋,厉小梅,王吉波,程永静,彭嘉婧,赵晓珍,邵苗,李茹. 系统性红斑狼疮低疾病活动度及缓解状况的真实世界研究[J]. 北京大学学报(医学版), 2024, 56(2): 273-278. |
| [9] | 赵祥格,刘佳庆,黄会娜,陆智敏,白自然,李霞,祁荆荆. 干扰素-α介导系统性红斑狼疮外周血CD56dimCD57+自然杀伤细胞功能的损伤[J]. 北京大学学报(医学版), 2023, 55(6): 975-981. |
| [10] | 姚海红,杨帆,唐素玫,张霞,何菁,贾园. 系统性红斑狼疮及成人Still病合并巨噬细胞活化综合征的临床特点及诊断指标[J]. 北京大学学报(医学版), 2023, 55(6): 966-974. |
| [11] | 罗芷筠,吴佳佳,宋优,梅春丽,杜戎. 伴神经精神系统病变的系统性红斑狼疮相关巨噬细胞活化综合征2例[J]. 北京大学学报(医学版), 2023, 55(6): 1111-1117. |
| [12] | 张警丰,金银姬,魏慧,姚中强,赵金霞. 体重指数与类风湿关节炎临床特征的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 993-999. |
| [13] | 邵苗,郭惠芳,雷玲彦,赵清,丁艳杰,林进,吴锐,于峰,李玉翠,苗华丽,张莉芸,杜燕,焦瑞英,庞丽霞,龙丽,栗占国,李茹. 短间期小剂量环磷酰胺治疗系统性红斑狼疮耐受性的多中心对照研究[J]. 北京大学学报(医学版), 2022, 54(6): 1112-1116. |
| [14] | 李敏,侯林卿,金月波,何菁. 系统性红斑狼疮合并视网膜病变的临床及免疫学特点[J]. 北京大学学报(医学版), 2022, 54(6): 1106-1111. |
| [15] | 张琳崎,赵静,王红彦,王宗沂,李英妮,汤稷旸,李思莹,曲进锋,赵明威. 抗ENO1抗体与狼疮性视网膜病变的相关性[J]. 北京大学学报(医学版), 2022, 54(6): 1099-1105. |
|
||