北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (6): 1023-1028. doi: 10.19723/j.issn.1671-167X.2024.06.012
育龄期系统性红斑狼疮患者卵巢功能的评价及其影响因素
陈丹丹1,2, 李云1, 卢情怡1, 相晓红1, 孙峰1, 李英妮1, 赵静1, 王红彦1, 李春*( )
)
- 1. 北京大学人民医院风湿免疫科,北京 100044
2. 秦皇岛市第一医院检验中心,河北秦皇岛 066000
Ovarian function in patients of childbearing age with systemic lupus erythematosus
Dandan CHEN1,2, Yun LI1, Qingyi LU1, Xiaohong XIANG1, Feng SUN1, Yingni LI1, Jing ZHAO1, Hongyan WANG1, Chun LI*( )
)
- 1. Department of Rheumatology and Immunology, Peking University People' s Hospital, Beijing 100044, China
2. Department of Laboratory, First Hospital of Qin Huang Dao, Qinhuangdao 066000, Hebei, China
摘要:
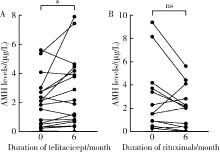
目的: 探讨育龄期系统性红斑狼疮(systemic lupus erythematosus,SLE)女性患者的卵巢功能及其影响因素。方法: 选取2017年1月至2024年5月于北京大学人民医院就诊明确诊断的SLE女性患者107例,年龄20~40岁,同时选取40例年龄在20~40岁之间的健康女性作为对照。采用化学发光法检测健康对照及SLE患者血清中抗缪勒氏管激素(anti-Müllerian hormone,AMH)水平,通过病例检索形式收集SLE患者的一般临床特征、用药情况(包括激素、免疫抑制剂及生物制剂),分析SLE患者接受生物制剂治疗前后血清中AMH水平的变化。结果: (1) SLE患者的AMH水平显著低于健康对照组[1.475(0.344, 3.030) μg/L vs. 2.934(1.893, 4.761) μg/L,P < 0.001]。(2)SLE患者月经正常组AMH水平显著高于月经不规律组[1.931(0.638,3.414) μg/L vs. 0.335(0.159,1.527) μg/L,P=0.004],AMH降低组与AMH正常组在临床特征及实验室指标方面差异无统计学意义。(3)多因素Logistic回归分析结果显示,年龄(OR=1.124,95%CI1.033~1.224,P=0.007)和病程(OR=1.100,95%CI1.017~1.190,P=0.018)是AMH下降的危险因素。(4)接受泰它西普治疗6个月后,患者AMH水平显著高于治疗前[治疗后2.050(0.763,4.259) μg/L vs.治疗前1.988(0.473,2.822) μg/L,P=0.043];接受利妥昔单抗治疗6个月后,患者AMH水平与治疗前差异无统计学意义[治疗后2.026(0.376,2.267) μg/L vs.治疗前1.545(0.503,3.414) μg/L,P=0.127]。结论: 育龄期SLE患者存在卵巢功能下降,年龄和病程是其危险因素;生物制剂的使用对于育龄期SLE患者的卵巢功能有较好的安全性。
中图分类号:
- R593.2
| 1 | 中华医学会风湿病学分会, 国家皮肤与免疫疾病临床医学研究中心, 中国系统性红斑狼疮研究协作组. 2020中国系统性红斑狼疮诊疗指南[J]. 中华内科杂志, 2020, 59 (3): 172- 185. |
| 2 | 刘霞, 张丽丽, 赵伟, 等. 环磷酰胺对育龄系统性红斑狼疮患者卵巢功能影响的评价[J]. 中华医学杂志, 2019, 99 (3): 174- 177. |
| 3 | 中国医师协会生殖医学专业委员会. 抗米勒管激素临床应用专家共识(2023年版)[J]. 中国实用妇科与产科杂志, 2023, 39 (4): 431- 439. |
| 4 | Gladman DD , Ibañez D , Urowitz MB . Systemic lupus erythematosus disease activity index 2000[J]. J Rheumatol, 2002, 29 (2): 288- 291. |
| 5 | 卵巢储备功能减退临床诊治专家共识专家组, 中华预防医学会生育力保护分会生殖内分泌生育保护学组. 卵巢储备功能减退临床诊治专家共识[J]. 生殖医学杂志, 2022, 31 (4): 425- 434. |
| 6 |
Dewailly D , Andersen CY , Balen A , et al. The physiology and clinical utility of anti-Mullerian hormone in women[J]. Hum Reprod Update, 2014, 20 (3): 370- 385.
doi: 10.1093/humupd/dmt062 |
| 7 |
Broer SL , Broekmans FJ , Laven JS , et al. Anti-Mullerian hormone: Ovarian reserve testing and its potential clinical implications[J]. Hum Reprod Update, 2014, 20 (5): 688- 701.
doi: 10.1093/humupd/dmu020 |
| 8 |
Garcia-Velasco JA , Moreno L , Pacheco A , et al. The aromatase inhibitor letrozole increases the concentration of intraovarian androgens and improves in vitro fertilization outcome in low responder patients: A pilot study[J]. Fertil Steril, 2005, 84 (1): 82- 87.
doi: 10.1016/j.fertnstert.2005.01.117 |
| 9 | Grossman MP , Nakajima ST , Fallat ME , et al. Müllerian-inhibiting substance inhibits cytochrome P450 aromatase activity in human granulosa lutein cell culture[J]. Fertil Steril, 2008, 89 (Suppl 5): S1364- S1370. |
| 10 | La Marca A , Grisendi V , Griesinger G . How much does AMH really vary in normal women?[J]. Int J Endocrinol, 2013, 2013, 959487. |
| 11 |
Khan HL , Bhatti S , Suhail S , et al. Antral follicle count (AFC) and serum anti-Müllerian hormone (AMH) are the predictors of natural fecundability have similar trends irrespective of fertility status and menstrual characteristics among fertile and infertile women below the age of 40 years[J]. Reprod Biol Endocrinol, 2019, 17 (1): 20.
doi: 10.1186/s12958-019-0464-0 |
| 12 |
Sharara FI , Scott JRT , Seifer DB . The detection of diminished ovarian reserve in infertile women[J]. Am J Obstet Gynecol, 1998, 179 (3): 804- 812.
doi: 10.1016/S0002-9378(98)70087-0 |
| 13 | 王国倩. 血清AMH水平与复发性流产的相关性分析[D]. 河南: 郑州大学, 2023. |
| 14 |
Luo W , Mao P , Zhang L , et al. Assessment of ovarian reserve by serum anti-Müllerian hormone in patients with systemic lupus erythematosus: A meta-analysis[J]. Ann Palliat Med, 2020, 9 (2): 207- 215.
doi: 10.21037/apm.2020.02.11 |
| 15 | Morales-Martínez FA , Salas-Castro C , García-Garza MR , et al. Evaluation of the ovarian reserve in women with systemic lupus erythematosus[J]. J Family Reprod Health, 2021, 15 (1): 38- 44. |
| 16 | 何瑞芬, 杨永秀, 梁晓磊. 卵巢储备功能减退动物模型研究进展[J]. 中国实验动物学报, 2024, 32 (2): 254- 259. |
| 17 |
Sun F , Wu H , Wang Z , et al. Effectiveness and safety of belimumab in chinese lupus patients: A multicenter, real-world observational study[J]. Biomedicines, 2023, 11 (3): 962.
doi: 10.3390/biomedicines11030962 |
| 18 |
Zhang F , Bae SC , Bass D , et al. A pivotal phase Ⅲ, rando-mised, placebo-controlled study of belimumab in patients with systemic lupus erythematosus located in China, Japan and South Korea[J]. Ann Rheum Dis, 2018, 77 (3): 355- 363.
doi: 10.1136/annrheumdis-2017-211631 |
| 19 |
Zhang F , Zheng J , Li Y , et al. Phase 3, long-term, open-label extension period of safety and efficacy of belimumab in patients with systemic lupus erythematosus in China, for up to 6 years[J]. RMD Open, 2022, 8 (1): e001669.
doi: 10.1136/rmdopen-2021-001669 |
| 20 |
Cai J , Gao D , Liu D , et al. Telitacicept for autoimmune nephro-pathy[J]. Front Immunol, 2023, 14, 1169084.
doi: 10.3389/fimmu.2023.1169084 |
| 21 | 耿研, 武丽君, 谢其冰, 等. 生物制剂在系统性红斑狼疮中应用的中国专家共识(2024版)[J]. 中华风湿病学杂志, 2024, 28 (2): 78- 92. |
| 22 |
Wood MA , Rajkovic A . Genomic markers of ovarian reserve[J]. Semin Reprod Med, 2013, 31 (6): 399- 415.
doi: 10.1055/s-0033-1356476 |
| 23 | 卢悦双. 早发性卵巢功能不全患者B细胞亚群及免疫球蛋白异常[D]. 山东: 山东大学, 2023. |
| [1] | 王红彦, 李鑫铭, 房柯池, 朱华群, 贾汝琳, 王晶. 系统性红斑狼疮疾病活动度相关特征分析及评估模型的构建[J]. 北京大学学报(医学版), 2024, 56(6): 1017-1022. |
| [2] | 王莉, 高超, 任欢欢, 沈艳平, 黄晓玮, 姚鸿, 韩丹丹. 系统性红斑狼疮患者自我管理能力现状及相关因素分析[J]. 北京大学学报(医学版), 2024, 56(6): 1029-1035. |
| [3] | 柴静, 王钥, 穆荣, 赵金霞. 系统性红斑狼疮累及穹窿柱导致低钠血症1例[J]. 北京大学学报(医学版), 2024, 56(6): 1115-1118. |
| [4] | 王明霞, 丁菱, 王敏, 邹婵娟, 颜丝语, 梁颖文, 王伟佳, 何善智. 双靶点嵌合抗原受体T细胞治疗系统性红斑狼疮患者停药后安全孕产1例[J]. 北京大学学报(医学版), 2024, 56(6): 1119-1125. |
| [5] | 武志慧, 胡明智, 赵巧英, 吕凤凤, 张晶莹, 张伟, 王永福, 孙晓林, 王慧. miR-125b-5p修饰脐带间充质干细胞对系统性红斑狼疮的免疫调控机制[J]. 北京大学学报(医学版), 2024, 56(5): 860-867. |
| [6] | 乔佳佳,田聪,黄晓波,刘军. 肾结石合并系统性红斑狼疮行经皮肾镜碎石取石术的安全性和有效性评估[J]. 北京大学学报(医学版), 2024, 56(4): 745-749. |
| [7] | 任立敏,赵楚楚,赵义,周惠琼,张莉芸,王友莲,沈凌汛,范文强,李洋,厉小梅,王吉波,程永静,彭嘉婧,赵晓珍,邵苗,李茹. 系统性红斑狼疮低疾病活动度及缓解状况的真实世界研究[J]. 北京大学学报(医学版), 2024, 56(2): 273-278. |
| [8] | 赵祥格,刘佳庆,黄会娜,陆智敏,白自然,李霞,祁荆荆. 干扰素-α介导系统性红斑狼疮外周血CD56dimCD57+自然杀伤细胞功能的损伤[J]. 北京大学学报(医学版), 2023, 55(6): 975-981. |
| [9] | 姚海红,杨帆,唐素玫,张霞,何菁,贾园. 系统性红斑狼疮及成人Still病合并巨噬细胞活化综合征的临床特点及诊断指标[J]. 北京大学学报(医学版), 2023, 55(6): 966-974. |
| [10] | 罗芷筠,吴佳佳,宋优,梅春丽,杜戎. 伴神经精神系统病变的系统性红斑狼疮相关巨噬细胞活化综合征2例[J]. 北京大学学报(医学版), 2023, 55(6): 1111-1117. |
| [11] | 邵苗,郭惠芳,雷玲彦,赵清,丁艳杰,林进,吴锐,于峰,李玉翠,苗华丽,张莉芸,杜燕,焦瑞英,庞丽霞,龙丽,栗占国,李茹. 短间期小剂量环磷酰胺治疗系统性红斑狼疮耐受性的多中心对照研究[J]. 北京大学学报(医学版), 2022, 54(6): 1112-1116. |
| [12] | 李敏,侯林卿,金月波,何菁. 系统性红斑狼疮合并视网膜病变的临床及免疫学特点[J]. 北京大学学报(医学版), 2022, 54(6): 1106-1111. |
| [13] | 张琳崎,赵静,王红彦,王宗沂,李英妮,汤稷旸,李思莹,曲进锋,赵明威. 抗ENO1抗体与狼疮性视网膜病变的相关性[J]. 北京大学学报(医学版), 2022, 54(6): 1099-1105. |
| [14] | 邹健梅,武丽君,罗采南,石亚妹,吴雪. 血清25-羟维生素D与系统性红斑狼疮活动的关系[J]. 北京大学学报(医学版), 2021, 53(5): 938-941. |
| [15] | 夏芳芳,鲁芙爱,吕慧敏,杨国安,刘媛. 系统性红斑狼疮伴间质性肺炎的临床特点及相关因素分析[J]. 北京大学学报(医学版), 2021, 53(2): 266-272. |
|
||