北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (5): 947-955. doi: 10.19723/j.issn.1671-167X.2025.05.020
镜下内侧髌股复合体重建治疗伴高级别滑车发育不良复发性髌骨脱位的临床疗效
胡枫艺, 孟庆阳, 陈拿云, 王佳宁, 刘振龙, 马勇, 杨渝平, 龚熹, 王成, 刘平*( ), 史尉利*(
), 史尉利*( )
)
- 北京大学第三医院运动医学科, 北京大学运动医学研究所, 运动医学关节伤病北京市重点实验室, 北京 100191
Clinical efficacy of arthroscopic medial patellofemoral complex reconstruction for recurrent patellar dislocation with high-grade trochlear dysplasia
Fengyi HU, Qingyang MENG, Nayun CHEN, Jianing WANG, Zhenlong LIU, Yong MA, Yuping YANG, Xi GONG, Cheng WANG, Ping LIU*( ), Weili SHI*(
), Weili SHI*( )
)
- Department of Sports Medicine, Peking University Third Hospital; Institute of Sports Medicine of Peking University; Beijing Key Laboratory of Sports Injuries, Beijing 100191, China
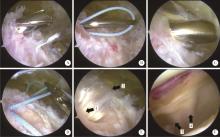
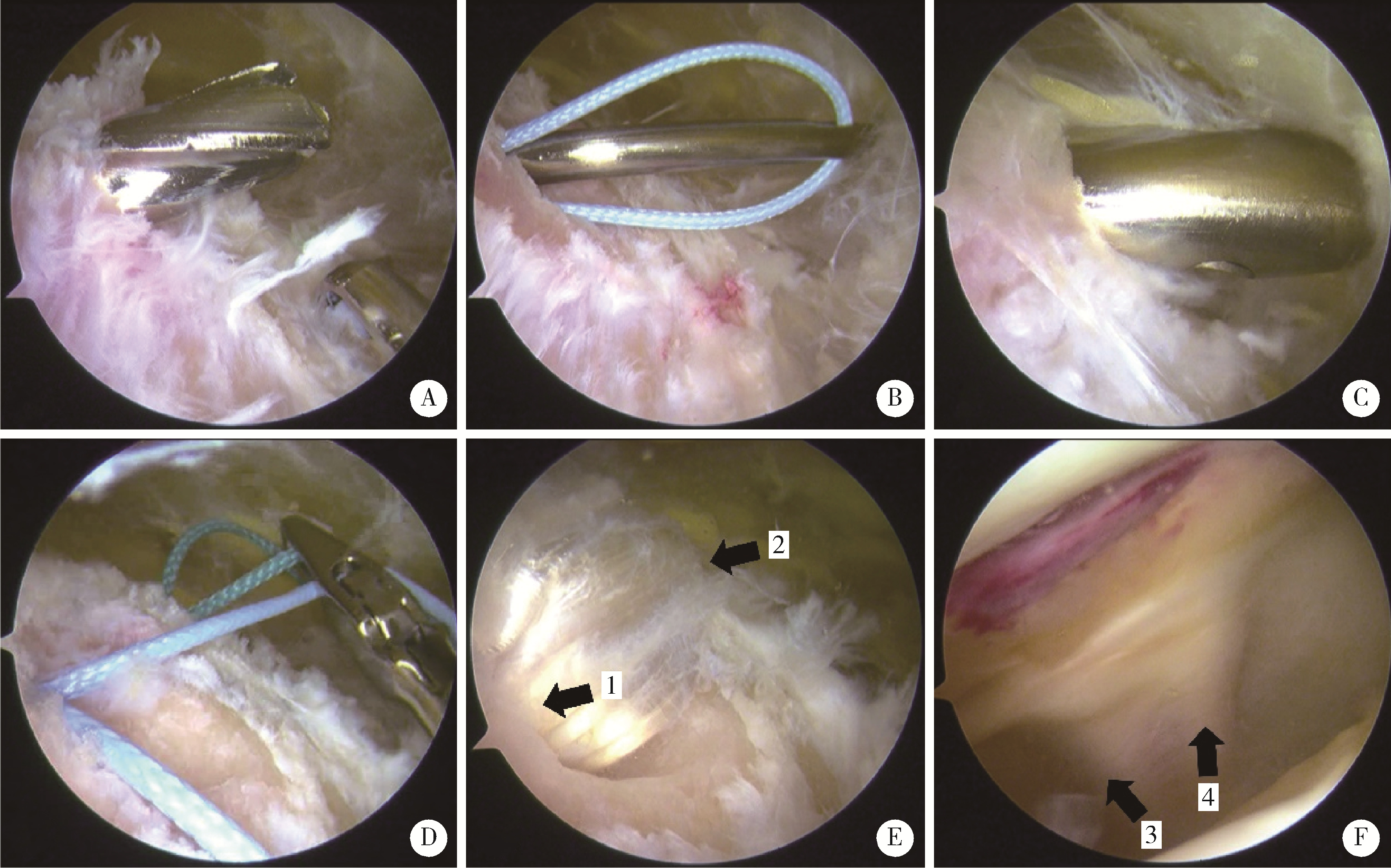
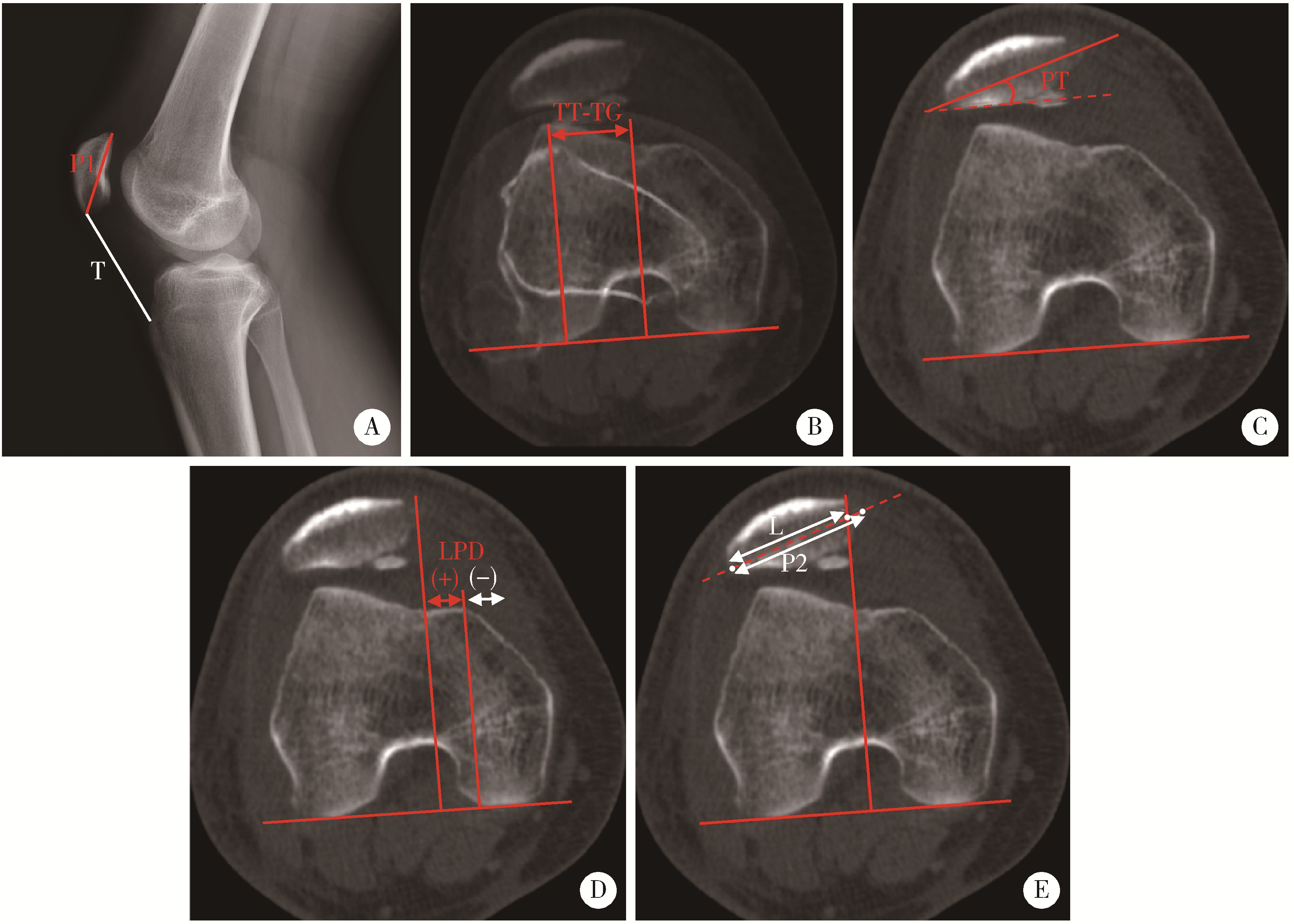
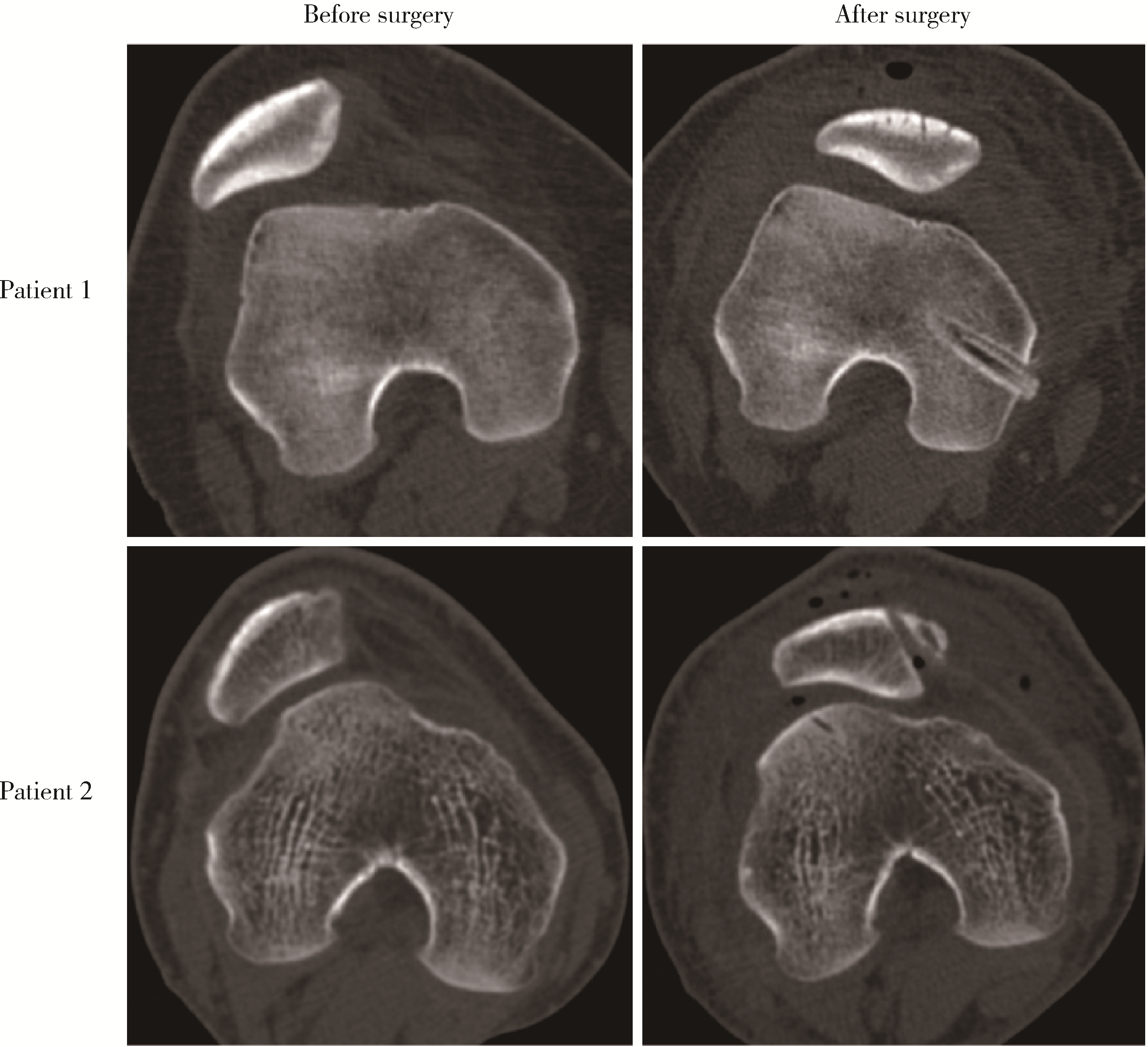
摘要: 目的: 探究关节镜下内侧髌股复合体(medial patellofemoral complex, MPFC)重建治疗伴高级别股骨滑车发育不良复发性髌骨脱位的中期临床疗效。方法: 回顾2014年1月至2020年12月间接受关节镜下MPFC重建的复发性髌骨脱位成人患者的临床资料, 评估Dejour分型以衡量滑车发育不良程度, 测量胫骨结节-股骨滑车沟(tibial tubercle-trochlear groove, TT-TG)间距与Insall-Salvati指数。比较术前和术后国际膝关节文献委员会(International Knee Documentation Committee, IKDC)、Kujala、Lysholm和Tegner评分, 评估运动恢复情况、复发与并发症。基于轴位电子计算机断层扫描影像, 测量术前和术后影像学参数髌骨倾斜角、髌骨外移距离和等分偏移率(bisect offset ratio, BSO)比值, 评估髌股关节对位关系恢复情况。结果: 共纳入43例患者(46膝), 其中男性16例, 女性27例。手术时患者平均年龄为(22.2±7.6)岁(范围为14~44岁), 平均随访(49.9±22.6)个月(范围为18~102个月)。Dejour B、C、D型分别占37.0%(17/46)、43.5%(20/46)和19.6%(9/46), 平均Insall-Salvati指数1.2±0.2(范围为0.85~1.44), 平均TT-TG间距(19.6±3.5) mm(范围为10.6~28.7 mm)。末次随访时, 各膝关节功能评分较术前均有显著提高(P < 0.001): IKDC评分由56.3±15.1至86.2±8.1, Kujala评分由58.9±15.6至92.6±5.4, Lysholm评分由63.7±15.0至94.0±5.7, Tegner评分由3.1±1.4至4.7±1.4, 改善量在Dejour各型之间差异无统计学意义, 总体运动恢复率达90%。1例患者出现术后髌骨半脱位, 所有患者均未报告关节感染、活动受限或髌骨骨折。术后髌骨倾斜角、髌骨外移距离和BSO比值较术前均有明显改善(P < 0.001)。结论: 关节镜下MPFC重建治疗伴高级别滑车发育不良复发性髌骨脱位的中期临床疗效满意, 高级别滑车发育不良各分型之间膝关节功能改善差异无统计学意义。
中图分类号:
- R684.76
| 1 |
doi: 10.1177/1941738117725055 |
| 2 |
doi: 10.1177/0363546517732045 |
| 3 |
doi: 10.1007/s00167-004-0607-4 |
| 4 |
doi: 10.1016/j.eats.2013.01.002 |
| 5 |
doi: 10.2106/JBJS.15.01182 |
| 6 |
doi: 10.1007/s00167-020-05999-2 |
| 7 |
doi: 10.1016/j.arthro.2020.01.058 |
| 8 |
印钰, 陈临新, 梅宇, 等. 内侧股四头肌腱股骨韧带重建联合单骨道内侧髌股韧带重建治疗复发性髌骨脱位的临床疗效[J]. 中国运动医学杂志, 2021, 40 (12): 936- 941.
|
| 9 |
doi: 10.1097/BPO.0000000000001259 |
| 10 |
doi: 10.1016/j.eats.2020.09.026 |
| 11 |
doi: 10.1016/j.eats.2019.01.006 |
| 12 |
doi: 10.1177/0363546516635626 |
| 13 |
doi: 10.1177/0363546515606102 |
| 14 |
doi: 10.1177/0363546520958423 |
| 15 |
doi: 10.1177/0363546517745625 |
| 16 |
doi: 10.1016/j.arthro.2022.06.038 |
| 17 |
|
| 18 |
doi: 10.2214/AJR.19.22400 |
| 19 |
doi: 10.1186/s12891-019-2697-7 |
| 20 |
doi: 10.1177/0363546520916435 |
| 21 |
doi: 10.1097/JSA.0000000000000252 |
| 22 |
doi: 10.1007/s00167-018-5266-y |
| 23 |
doi: 10.1177/0363546515572143 |
| 24 |
doi: 10.1177/03635465211041087 |
| 25 |
doi: 10.1177/0363546519838405 |
| 26 |
doi: 10.1177/0363546513518413 |
| 27 |
doi: 10.1007/s00167-015-3698-1 |
| 28 |
doi: 10.1016/j.arthro.2022.04.019 |
| 29 |
doi: 10.1177/0363546519835800 |
| [1] | 李钰锴, 王红彦, 罗靓, 李云, 李春. 抗磷脂抗体在白塞病合并血栓中的临床意义[J]. 北京大学学报(医学版), 2024, 56(6): 1036-1040. |
| [2] | 李春, 胡晓丹. 关注血栓性抗磷脂综合征的长期抗凝[J]. 北京大学学报(医学版), 2024, 56(6): 947-949. |
| [3] | 朱玉静, 王磊, 吕成银, 谈文峰, 张缪佳. 抗EJ抗体阳性抗合成酶综合征相关间质性肺疾病复发的临床特征分析[J]. 北京大学学报(医学版), 2024, 56(6): 980-986. |
| [4] | 李雨清,王飚,乔鹏,王玮,关星. 经耻骨后尿道中段悬吊带术治疗女性复发性压力性尿失禁的中长期疗效[J]. 北京大学学报(医学版), 2024, 56(4): 600-604. |
| [5] | 姚中强,李常虹,李欣艺,郭苇,翟佳羽,刘蕊,魏慧,穆荣. 抗磷脂酰丝氨酸/凝血酶原抗体与不明原因复发性流产的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 1058-1061. |
| [6] | 陈素华,杨军,陈新,杨辰龙,孙建军,林国中,于涛,杨欣,韩芸峰,吴超,司雨,马凯明. 大型、巨大型上矢状窦中后1/3侵犯颅外复发脑膜瘤的手术治疗[J]. 北京大学学报(医学版), 2022, 54(5): 1006-1012. |
| [7] | 王跃,张爽,张虹,梁丽,徐玲,程元甲,段学宁,刘荫华,李挺. 激素受体阳性/人表皮生长因子受体2阴性乳腺癌临床病理特征及预后[J]. 北京大学学报(医学版), 2022, 54(5): 853-862. |
| [8] | 森本智惠子,王益勤,周蓉,王建六. 子宫内膜非典型增生及子宫内膜癌患者保留生育功能治疗的临床研究[J]. 北京大学学报(医学版), 2022, 54(5): 936-942. |
| [9] | 刘磊,秦艳春,王国良,张树栋,侯小飞,马潞林. 嗜铬细胞瘤和副神经节瘤二次手术策略[J]. 北京大学学报(医学版), 2021, 53(4): 793-797. |
| [10] | 于焕斌,伍文杰,吕晓鸣,石妍,郑磊,张建国. 125I粒子近距离治疗外放疗后复发唾液腺癌[J]. 北京大学学报(医学版), 2020, 52(5): 919-923. |
| [11] | 熊盛炜,王杰,朱伟杰,程嗣达,张雷,李学松,周利群. 二次肾盂成形术在复发性肾盂输尿管连接部梗阻中的研究进展[J]. 北京大学学报(医学版), 2020, 52(4): 794-798. |
| [12] | 侯磊,叶国华,刘筱菁,李自力. 下颌后缩伴颞下颌关节重度骨关节病患者正颌术后颌骨稳定性及髁突体积变化的评价[J]. 北京大学学报(医学版), 2020, 52(1): 113-118. |
| [13] | 张旭初,张建华,王荣福,范岩,付占立,闫平,赵光宇,白艳霞. 18F-FDG PET/CT联合多种肿瘤标志物在结直肠中分化腺癌术后复发及转移中的应用价值[J]. 北京大学学报(医学版), 2019, 51(6): 1071-1077. |
| [14] | 唐琦,林榕城,姚林,张争,郝瀚,张崔建,蔡林,李学松,何志嵩,周利群. 肾癌术后局部复发患者的临床病理特征及预后分析[J]. 北京大学学报(医学版), 2019, 51(4): 628-631. |
| [15] | 朱冉,倪照军,张顺,庞良俊,王传升,鲍彦平,孙洪强. 临床特征对酒精依赖复发的影响:前瞻性队列研究[J]. 北京大学学报(医学版), 2019, 51(3): 519-524. |
|
||