Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (5): 928-932. doi: 10.19723/j.issn.1671-167X.2021.05.019
Previous Articles Next Articles
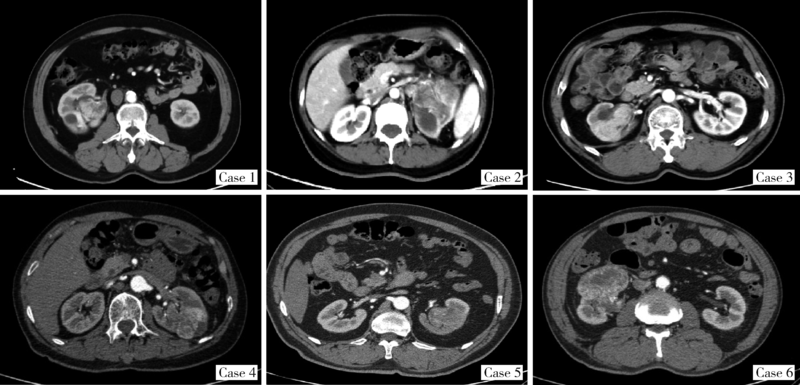
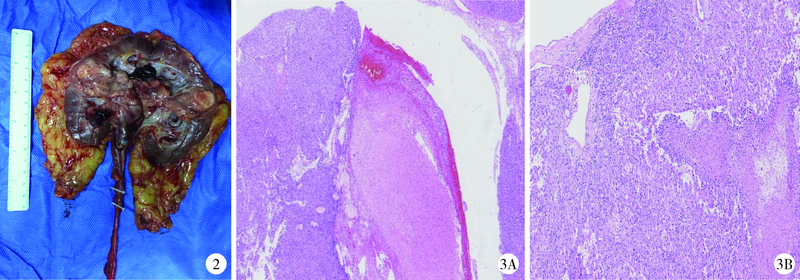
Clinical and pathological features of renal cell carcinoma with urinary tract tumor thrombus: 6 cases report and literature review
TIAN Yu1,CHENG Xiao-yue2,HE Hui-ying3,WANG Guo-liang1,△( ),MA Lu-lin1
),MA Lu-lin1
- 1. Department of Urology, Peking University Third Hospital, Beijing 100191, China
2. Department of Radiology, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China
3. Department of Pathology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R737.11
| [1] |
Munechika H, Kushihashi T, Gokan T, et al. A renal cell carcinoma extending into the renal pelvis simulating transitional cell carcinoma [J]. Urol Radiol, 1990, 12(1):11-14.
pmid: 2333668 |
| [2] | Chen WC, Lee YH, Huang JK. Renal cell carcinoma with renal pelvic extension simulating transitional cell carcinoma: a case report [J]. Zhonghua Yi Xue Za Zhi, 1996, 58(2):147-150. |
| [3] |
Gulati M, Gore JL, Pantuek AJ, et al. Ureteral tumor thrombus from renal cell carcinoma extending into bladder [J]. Urol Oncol, 2007, 25(5):393-395.
doi: 10.1016/j.urolonc.2007.01.011 |
| [4] |
Fujita O, Wada K, Yamasaki T, et al. Renal cell carcinoma with a tumor thrombus in the ureter: a case report [J]. BMC Urol, 2011, 11(16):1-5.
doi: 10.1186/1471-2490-11-1 |
| [5] |
Kitazono MT, Coakley FV, Naeger DM, et al. CT of unusual renal masses invading the pelvicaliceal system: potential mimics of upper tract transitional cell carcinoma [J]. Clin Imaging, 2011, 35(1):77-80.
doi: 10.1016/j.clinimag.2010.02.012 |
| [6] |
Jeong YB, Kim HJ. Is it transitional cell carcinoma or renal cell carcinoma on computed tomography image? [J]. Urology, 2012, 79(3):e42-e43.
doi: 10.1016/j.urology.2011.11.001 |
| [7] | Kakutani S, Kume H, Hirano Y, et al. Renal cell carcinoma with intraluminal spread of the entire upper urinary tract [J]. Case Rep Med, 2013, 2013:371387. |
| [8] |
Li Y, Ding YU, Chen D. Renal cell carcinoma growing into the renal pelvis and mimicking transitional cell carcinoma: A case report and literature review [J]. Oncol Lett, 2015, 9(4):1869-1872.
doi: 10.3892/ol.2015.2898 |
| [9] | 李嘉临, 纪志刚. 肾嫌色细胞癌侵入肾盂一例分析及文献复习 [J]. 国际外科学杂志, 2016, 43(9):625-627. |
| [10] |
Komatsubara M, Yamazaki M, Fujisaki A, et al. Tumor thrombus of renal cell carcinoma extending into the inferior vena cava, ova-rian vein, and ureter treated with neoadjuvant axitinib [J]. Urology, 2016, 95:e3-e4.
doi: 10.1016/j.urology.2016.05.057 |
| [11] | Parikesit D, Mochtar CA, Tanurahardja B, et al. Thrombus-like tumor of renal cell carcinoma mimicking transitional cell carcinoma of kidney: a case report [J]. Urol Case Rep, 2016, 10:26-29. |
| [12] |
Ishikawa T, Izumi K, Kondo T, et al. A case of renal cell carcinoma growing into the renal pelvis with a fibrin cap in the ureter and bladder [J]. Hinyokika Kiyo, 2018, 64(3):117-122.
doi: 10.14989/ActaUrolJap_64_3_117 pmid: 29684961 |
| [13] |
Jeff J, Alessandro P. Clear cell renal cell carcinoma with a urete-ral thrombus [J]. J Endourol Case Rep, 2018, 4(1):159-162.
doi: 10.1089/cren.2018.0067 pmid: 30426074 |
| [14] |
Bowman M, Reinstatler L, Pettus J, et al. An unusual case of renal cell carcinoma with tumor thrombosis of the proximal ureter [J]. Urol Case Rep, 2019, 23:60-61.
doi: 10.1016/j.eucr.2018.12.009 pmid: 30596019 |
| [15] | Kumar L, Jain S, Kaushal S, et al. A case of type 1 papillary renal cell cancer with pelvic tumor thrombus masquerading as urothelial cancer with review of literature [J]. J Endourol Case Rep, 2019, 5(4):157-160. |
| [16] | Riehie JP. Carcinoma of the renal pelvis and ureter. Diagnosis and management of genitourinary cancer [M]. Philadelphia: Saunders, 1988: 323-336. |
| [17] | National Cancer Institute. SEER Stat Fact Sheets: Kidney and renal pelvis cancer [EB/OL]. (2015-11-29) [2020-18-16]. http://seer.cancer.gov/statfacts/html/kidrp.html . |
| [18] | 李松年. 中华影像医学: 泌尿生殖系统卷 [M]. 北京: 人民卫生出版社, 2002. |
| [19] |
Bata P, Tarnoki DL, Tarnoki AD, et al. Transitional cell and clear cell renal carcinoma: Differentiation of distinct histological types with multiphase CT [J]. Acta Radiol, 2014, 55(9):1112-1119.
doi: 10.1177/0284185113510493 pmid: 24243889 |
| [20] | Amin MB, Edge SB, Greene FL, et al. AJCC cancer staging manual [M]. 8th ed. New York: Springer, 2017. |
| [1] | Junyong OU,Kunming NI,Lulin MA,Guoliang WANG,Ye YAN,Bin YANG,Gengwu LI,Haodong SONG,Min LU,Jianfei YE,Shudong ZHANG. Prognostic factors of patients with muscle invasive bladder cancer with intermediate-to-high risk prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 582-588. |
| [2] | Fan SHU,Yichang HAO,Zhanyi ZHANG,Shaohui DENG,Hongxian ZHANG,Lei LIU,Guoliang WANG,Xiaojun TIAN,Lei ZHAO,Lulin MA,Shudong ZHANG. Functional and oncologic outcomes of partial nephrectomy for cystic renal cell carcinoma: A single-center retrospective study [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 667-672. |
| [3] | Zezhen ZHOU,Shaohui DENG,Ye YAN,Fan ZHANG,Yichang HAO,Liyuan GE,Hongxian ZHANG,Guoliang WANG,Shudong ZHANG. Predicting the 3-year tumor-specific survival in patients with T3a non-metastatic renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 673-679. |
| [4] | Yun-chong LIU,Zong-long WU,Li-yuan GE,Tan DU,Ya-qian WU,Yi-meng SONG,Cheng LIU,Lu-lin MA. Mechanism of nuclear protein 1 in the resistance to axitinib in clear cell renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 781-792. |
| [5] | Dong LAN,Zhuo LIU,Yu-xuan LI,Guo-liang WANG,Xiao-jun TIAN,Lu-lin MA,Shu-dong ZHANG,Hong-xian ZHANG. Risk factors for massive hemorrhage after radical nephrectomy and removal of venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 825-832. |
| [6] | Han LU,Jian-yun ZHANG,Rong YANG,Le XU,Qing-xiang LI,Yu-xing GUO,Chuan-bin GUO. Clinical factors affecting the prognosis of lower gingival squamous cell carcinoma [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 702-707. |
| [7] | Yun-yi XU,Zheng-zheng SU,Lin-mao ZHENG,Meng-ni ZHANG,Jun-ya TAN,Ya-lan YANG,Meng-xin ZHANG,Miao XU,Ni CHEN,Xue-qin CHEN,Qiao ZHOU. Read-through circular RNA rt-circ-HS promotes hypoxia inducible factor 1α expression and renal carcinoma cell proliferation, migration and invasiveness [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 217-227. |
| [8] | Qi SHEN,Yi-xiao LIU,Qun HE. Mucinous tubular and spindle cell carcinoma of kidney: Clinicopathology and prognosis [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 276-282. |
| [9] | Quan ZHANG,Hai-feng SONG,Bing-lei MA,Zhe-nan ZHANG,Chao-hui ZHOU,Ao-lin LI,Jun LIU,Lei LIANG,Shi-yu ZHU,Qian ZHANG. Pre-operative prognostic nutritional index as a predictive factor for prognosis in non-metastatic renal cell carcinoma treated with surgery [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 149-155. |
| [10] | Mei-ni ZUO,Yi-qing DU,Lu-ping YU,Xiang DAI,Tao XU. Correlation between metabolic syndrome and prognosis of patients with clear cell renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 636-643. |
| [11] | Tian-yu CAI,Zhen-peng ZHU,Chun-ru XU,Xing JI,Tong-de LV,Zhen-ke GUO,Jian LIN. Expression and significance of fibroblast growth factor receptor 2 in clear cell renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 628-635. |
| [12] | Er-shu BO,Peng HONG,Yu ZHANG,Shao-hui DENG,Li-yuan GE,Min LU,Nan LI,Lu-lin MA,Shu-dong ZHANG. Clinicopathological features and prognostic analysis of papillary renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 615-620. |
| [13] | Cai-peng QIN,Yu-xuan SONG,Meng-ting DING,Fei WANG,Jia-xing LIN,Wen-bo YANG,Yi-qing DU,Qing LI,Shi-jun LIU,Tao XU. Establishment of a mutation prediction model for evaluating the efficacy of immunotherapy in renal carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 663-668. |
| [14] | HONG Peng,TIAN Xiao-jun,ZHAO Xiao-yu,YANG Fei-long,LIU Zhuo,LU Min,ZHAO Lei,MA Lu-lin. Bilateral papillary renal cell carcinoma following kidney transplantation: A case report [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 811-813. |
| [15] | HAN Song-chen,HUANG Zi-xiong,LIU Hui-xin,XU Tao. Renal functional compensation after unilateral radical nephrectomy of renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 680-685. |
|
||