北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (3): 557-563. doi: 10.19723/j.issn.1671-167X.2020.03.024
高脂饲料诱导肥胖胰岛素抵抗大鼠模型的建立
- 北京大学第三医院运动医学研究所, 北京 100191
Establishment of high-fat diet-induced obesity and insulin resistance model in rats
Xiao-yuan ZHANG,Cheng-cheng GUO,Ying-xiang YU,Lan XIE,Cui-qing CHANG( )
)
- Institute of Sports Medicine, Peking University Third Hospital, Beijing 100191, China
摘要:
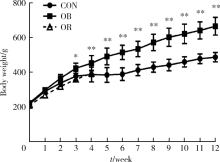
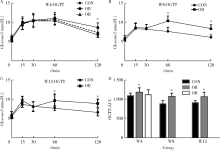
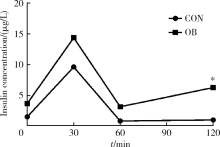
目的 通过普通饲料和高脂饲料喂养大鼠,探讨建立肥胖胰岛素抵抗大鼠模型的适宜条件和时间。方法 将45只6周龄雄性SD大鼠随机分为普通饲料对照组和高脂饲料组(脂肪供能比为45%), 喂养4周后剔除高脂饲料组肥胖抵抗(obesity resistance,OR)大鼠,肥胖(obese,OB)大鼠继续喂养至12周。分别于4、8、12周末进行口服葡萄糖耐量试验(oral glucose tolerance test,OGTT),12周末检测胰岛素释放、内脏脂肪、胰腺、肝脏等组织的病理变化。结果 高脂饲料喂养4周后,高脂饲料组大鼠的体质量比对照组高17.8%(P=0.001),肥胖成模率为67.6%~78.4%,OB大鼠出现糖耐量降低,OGTT 120 min血糖比对照组高27.5%(P<0.001),曲线下面积(area under the curve, AUC)比对照组高8.3%(P=0.037),79.3%的大鼠出现肥胖胰岛素抵抗;喂养8周时,OB大鼠体质量比对照组高30.4%(P<0.001),OGTT 60 min和120 min血糖分别比对照组高35.6%(P<0.001)和36.4%(P<0.001),AUC比对照组高21.7%(P<0.001),100.0%大鼠出现肥胖胰岛素抵抗;喂养12周时,OB大鼠体质量比对照组高36.9%(P<0.001),OGTT 60 min和120 min血糖分别比对照组高24.8%(P=0.001)和34.6%(P<0.001),AUC比对照组高16.1%(P=0.019),93.3%的大鼠出现肥胖胰岛素抵抗。胰岛素释放实验显示,高脂饲料组各时间点血清胰岛素均高于对照组,120 min时胰岛素浓度是对照组的6.3倍(P=0.008),胰岛和肝脏出现病理改变。结论 使用脂肪供能比为45%的高脂饲料喂养6周龄SD大鼠4周后淘汰OR大鼠,OB大鼠中出现糖耐量异常,8~12周后成模率更高。
中图分类号:
- R-332
| [1] | Rees DA, Alcolado JC. Animal models of diabetes mellitus[J]. Diabet Med, 2005,22(4):359-370. |
| [2] | Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications[J]. Nat Rev Endocrinol, 2013,9(1):13-27. |
| [3] | Chen D, Wang MW. Development and application of rodent models for type 2 diabetes[J]. Diabetes Obes Metab, 2005,7(4):307-317. |
| [4] | Panchal SK, Brown L. Rodent models for metabolic syndrome research[J]. J Biomed Biotechnol, 2011,2011:351982. doi: 10.1155/2011/351982. |
| [5] | 张小华, 张汝学, 贾正平, 等. 高脂饮食和地塞米松联合诱导胰岛素抵抗大鼠模型[J]. 中国实验动物学报, 2008,16(5):325-329. |
| [6] | Chen SH, Zhuang XH, Liu YT, et al. Expression and significance of lipin1 and AMPKalpha in hepatic insulin resistance in diet-induced insulin resistance rats[J]. Exp Clin Endocrinol Diabetes, 2012,120(2):84-88. |
| [7] |
Marques C, Meireles M, Norberto S, et al. High-fat diet-induced obesity rat model: a comparison between Wistar and Sprague-Dawley rat[J]. Adipocyte, 2016,5(1):11-21.
doi: 10.1080/21623945.2015.1061723 pmid: 27144092 |
| [8] |
Davidson EP, Coppey LJ, Dake B, et al. Effect of treatment of Sprague-Dawley rats with AVE7688, enalapril, or candoxatril on diet-induced obesity [J]. J Obes, 2011, 2011: pii: 686952. doi: 10.1155/2011/686952.
pmid: 20847891 |
| [9] |
Reed MJ, Meszaros K, Entes LJ, et al. A new rat model of type 2 diabetes: the fat-fed, streptozotocin-treated rat[J]. Metabolism, 2000,49(11):1390-1394.
doi: 10.1053/meta.2000.17721 pmid: 11092499 |
| [10] | 王智华, 宋光耀, 刘晶, 等. 高脂饮食诱发胰岛素抵抗大鼠模型的建立与评价[J]. 现代中西医结合杂志, 2012,21(3):244-245. |
| [11] | Svegliati-Baroni G, Candelaresi C, Saccomanno S, et al. A model of insulin resistance and nonalcoholic steatohepatitis in rats: role of peroxisome proliferator-activated receptor-alpha and n-3 polyunsa-turated fatty acid treatment on liver injury[J]. Am J Pathol, 2006,169(3):846-860. |
| [12] | Hariri N, Thibault L. High-fat diet-induced obesity in animal models[J]. Nutr Res Rev, 2010,23(2):270-299. |
| [13] | 那立欣, 赵丹, 宁华, 等. 减肥功能实验动物模型的改良[J]. 卫生研究, 2010,39(2):162-164. |
| [14] |
Kleiner DE Brunt EM van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease[J]. Hepatology, 2005,41(6):1313-1321.
pmid: 15915461 |
| [15] |
Levin BE, Dunn-Meynell AA, Balkan B, et al. Selective breeding for diet-induced obesity and resistance in Sprague-Dawley rats[J]. Am J Physiol, 1997,273(2 Pt 2):R725-R730.
doi: 10.1152/ajpregu.1997.273.2.R725 pmid: 9277561 |
| [16] |
Cheng HS, Ton SH, Phang S, et al. Increased susceptibility of post-weaning rats on high-fat diet to metabolic syndrome[J]. J Adv Res, 2017,8(6):743-752.
pmid: 29062573 |
| [17] | Giles ED, Jackman MR, Maclean PS. Modeling diet-induced obesity with obesity-prone rats: Implications for studies in females[J]. Front Nutr, 2016,3(3):50. |
| [18] | Ghibaudi L, Cook J, Farley C, et al. Fat intake affects adiposity, comorbidity factors, and energy metabolism of sprague-dawley rats[J]. Obes Res, 2002,10(9):956-963. |
| [19] |
Chalkley SM, Hettiarachchi M, Chisholm DJ, et al. Long-term high-fat feeding leads to severe insulin resistance but not diabetes in Wistar rats[J]. Am J Physiol Endocrinol Metab, 2002,282(6):E1231-E1238.
pmid: 12006352 |
| [20] | Malvi P, Piprode V, Chaube B, et al. High fat diet promotes achievement of peak bone mass in young rats[J]. Biochem Biophys Res Commun, 2014,455(1-2):133-138. |
| [21] | Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease[J]. J Clin Invest, 2011,121(6):2111-2117. |
| [22] |
Karalis KP, Giannogonas P, Kodela E, et al. Mechanisms of obesity and related pathology: Linking immune responses to metabolic stress[J]. FEBS J, 2009,276(20):5747-5754.
pmid: 19754872 |
| [23] | Hotamisligil GS. Inflammatory pathways and insulin action[J]. Int J Obes Relat Metab Disord, 2003,27(Suppl 3):S53-55. |
| [24] | Shapiro H, Lutaty A, Ariel A. Macrophages, meta-inflammation, and immuno-metabolism[J]. Scientific World J, 2011,11(6):2509-2529. |
| [1] | 刘思民,赵一姣,王晓燕,王祖华. 动态导航下不同深度环钻定位精确度的体外评价[J]. 北京大学学报(医学版), 2022, 54(1): 146-152. |
| [2] | 贾睿璇,姜尚伟,赵琳,杨丽萍. Cyp4v3基因敲除小鼠模型的表型分析[J]. 北京大学学报(医学版), 2021, 53(6): 1099-1106. |
| [3] | 王贵红,左婷,李然,左正才. 瑞巴派特在大鼠痛风性关节炎急性发作中的作用[J]. 北京大学学报(医学版), 2021, 53(4): 716-720. |
| [4] | 尹雪倩, 张晓玄, 文婧, 刘思奇, 刘欣然, 周若宇, 王军波. 荞麦、燕麦、豌豆复配对糖尿病大鼠血糖的影响[J]. 北京大学学报(医学版), 2021, 53(3): 447-452. |
| [5] | 刘秋萍,陈汐瑾,王佳敏,刘晓非,司亚琴,梁靖媛,沈鹏,林鸿波,唐迅,高培. 基于马尔可夫模型的社区人群心血管病筛查策略的效果评价[J]. 北京大学学报(医学版), 2021, 53(3): 460-466. |
| [6] | 王晓琪,陈美君,云青萍,孙思伟,王熙凯,史宇晖,纪颖,管仲军,常春. 门诊患者健康素养对就医体验的影响及机制[J]. 北京大学学报(医学版), 2021, 53(3): 560-565. |
| [7] | 张佳伟, 韩沛恩, 杨莉. 新型冠状病毒肺炎疫情分级防控水平下北京市发热门诊空间可及性[J]. 北京大学学报(医学版), 2021, 53(3): 543-548. |
| [8] | 陈怀安,刘硕,李秀君,王哲,张潮,李凤岐,苗文隆. 炎症生物标志物对输尿管尿路上皮癌患者预后预测的临床价值[J]. 北京大学学报(医学版), 2021, 53(2): 302-307. |
| [9] | 王志成,郭岩. 中国社区社会经济地位和成人自评健康的关联研究[J]. 北京大学学报(医学版), 2021, 53(2): 314-319. |
| [10] | 王双佳,王婷婷,王军波. 北京某高校医学院师生营养知信行水平及其影响因素[J]. 北京大学学报(医学版), 2020, 52(5): 881-885. |
| [11] | 萧宁,孙玉春,赵一姣,王勇. 三种数字化分析算法测量咬合接触分布及面积的对比研究[J]. 北京大学学报(医学版), 2020, 52(1): 144-151. |
| [12] | 白珊珊,莫思怡,徐啸翔,刘云,谢秋菲,曹烨. 大鼠咬合干扰致口颌面痛敏的自我赏罚实验行为学特点[J]. 北京大学学报(医学版), 2020, 52(1): 51-57. |
| [13] | 张勇,刘畅,陈彬,陈帆,段晋瑜,张孟钧,焦剑. 糖尿病前期患者糖代谢异常与慢性牙周炎的相关性[J]. 北京大学学报(医学版), 2020, 52(1): 71-76. |
| [14] | 杨飞龙,洪锴,赵国江,刘承,宋一萌,马潞林. 基于长链非编码RNA的生物信息学分析构建膀胱癌预后模型并确定预后生物标志物[J]. 北京大学学报(医学版), 2019, 51(4): 615-622. |
| [15] | 朱学华,杨明钰,夏海缀,何为,张智荧,刘余庆,肖春雷,马潞林,卢剑. 机器学习模型在预测肾结石输尿管软镜碎石术后早期结石清除率中的应用[J]. 北京大学学报(医学版), 2019, 51(4): 653-659. |
|