北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (3): 557-563. doi: 10.19723/j.issn.1671-167X.2020.03.024
高脂饲料诱导肥胖胰岛素抵抗大鼠模型的建立
- 北京大学第三医院运动医学研究所, 北京 100191
Establishment of high-fat diet-induced obesity and insulin resistance model in rats
Xiao-yuan ZHANG,Cheng-cheng GUO,Ying-xiang YU,Lan XIE,Cui-qing CHANG( )
)
- Institute of Sports Medicine, Peking University Third Hospital, Beijing 100191, China
摘要:
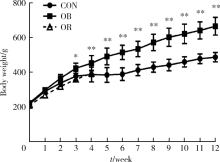
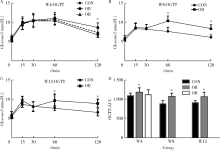
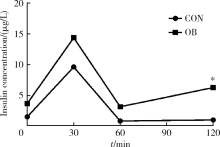
目的 通过普通饲料和高脂饲料喂养大鼠,探讨建立肥胖胰岛素抵抗大鼠模型的适宜条件和时间。方法 将45只6周龄雄性SD大鼠随机分为普通饲料对照组和高脂饲料组(脂肪供能比为45%), 喂养4周后剔除高脂饲料组肥胖抵抗(obesity resistance,OR)大鼠,肥胖(obese,OB)大鼠继续喂养至12周。分别于4、8、12周末进行口服葡萄糖耐量试验(oral glucose tolerance test,OGTT),12周末检测胰岛素释放、内脏脂肪、胰腺、肝脏等组织的病理变化。结果 高脂饲料喂养4周后,高脂饲料组大鼠的体质量比对照组高17.8%(P=0.001),肥胖成模率为67.6%~78.4%,OB大鼠出现糖耐量降低,OGTT 120 min血糖比对照组高27.5%(P<0.001),曲线下面积(area under the curve, AUC)比对照组高8.3%(P=0.037),79.3%的大鼠出现肥胖胰岛素抵抗;喂养8周时,OB大鼠体质量比对照组高30.4%(P<0.001),OGTT 60 min和120 min血糖分别比对照组高35.6%(P<0.001)和36.4%(P<0.001),AUC比对照组高21.7%(P<0.001),100.0%大鼠出现肥胖胰岛素抵抗;喂养12周时,OB大鼠体质量比对照组高36.9%(P<0.001),OGTT 60 min和120 min血糖分别比对照组高24.8%(P=0.001)和34.6%(P<0.001),AUC比对照组高16.1%(P=0.019),93.3%的大鼠出现肥胖胰岛素抵抗。胰岛素释放实验显示,高脂饲料组各时间点血清胰岛素均高于对照组,120 min时胰岛素浓度是对照组的6.3倍(P=0.008),胰岛和肝脏出现病理改变。结论 使用脂肪供能比为45%的高脂饲料喂养6周龄SD大鼠4周后淘汰OR大鼠,OB大鼠中出现糖耐量异常,8~12周后成模率更高。
中图分类号:
- R-332
| [1] | Rees DA, Alcolado JC. Animal models of diabetes mellitus[J]. Diabet Med, 2005,22(4):359-370. |
| [2] | Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications[J]. Nat Rev Endocrinol, 2013,9(1):13-27. |
| [3] | Chen D, Wang MW. Development and application of rodent models for type 2 diabetes[J]. Diabetes Obes Metab, 2005,7(4):307-317. |
| [4] | Panchal SK, Brown L. Rodent models for metabolic syndrome research[J]. J Biomed Biotechnol, 2011,2011:351982. doi: 10.1155/2011/351982. |
| [5] | 张小华, 张汝学, 贾正平, 等. 高脂饮食和地塞米松联合诱导胰岛素抵抗大鼠模型[J]. 中国实验动物学报, 2008,16(5):325-329. |
| [6] | Chen SH, Zhuang XH, Liu YT, et al. Expression and significance of lipin1 and AMPKalpha in hepatic insulin resistance in diet-induced insulin resistance rats[J]. Exp Clin Endocrinol Diabetes, 2012,120(2):84-88. |
| [7] |
Marques C, Meireles M, Norberto S, et al. High-fat diet-induced obesity rat model: a comparison between Wistar and Sprague-Dawley rat[J]. Adipocyte, 2016,5(1):11-21.
doi: 10.1080/21623945.2015.1061723 pmid: 27144092 |
| [8] |
Davidson EP, Coppey LJ, Dake B, et al. Effect of treatment of Sprague-Dawley rats with AVE7688, enalapril, or candoxatril on diet-induced obesity [J]. J Obes, 2011, 2011: pii: 686952. doi: 10.1155/2011/686952.
pmid: 20847891 |
| [9] |
Reed MJ, Meszaros K, Entes LJ, et al. A new rat model of type 2 diabetes: the fat-fed, streptozotocin-treated rat[J]. Metabolism, 2000,49(11):1390-1394.
doi: 10.1053/meta.2000.17721 pmid: 11092499 |
| [10] | 王智华, 宋光耀, 刘晶, 等. 高脂饮食诱发胰岛素抵抗大鼠模型的建立与评价[J]. 现代中西医结合杂志, 2012,21(3):244-245. |
| [11] | Svegliati-Baroni G, Candelaresi C, Saccomanno S, et al. A model of insulin resistance and nonalcoholic steatohepatitis in rats: role of peroxisome proliferator-activated receptor-alpha and n-3 polyunsa-turated fatty acid treatment on liver injury[J]. Am J Pathol, 2006,169(3):846-860. |
| [12] | Hariri N, Thibault L. High-fat diet-induced obesity in animal models[J]. Nutr Res Rev, 2010,23(2):270-299. |
| [13] | 那立欣, 赵丹, 宁华, 等. 减肥功能实验动物模型的改良[J]. 卫生研究, 2010,39(2):162-164. |
| [14] |
Kleiner DE Brunt EM van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease[J]. Hepatology, 2005,41(6):1313-1321.
pmid: 15915461 |
| [15] |
Levin BE, Dunn-Meynell AA, Balkan B, et al. Selective breeding for diet-induced obesity and resistance in Sprague-Dawley rats[J]. Am J Physiol, 1997,273(2 Pt 2):R725-R730.
doi: 10.1152/ajpregu.1997.273.2.R725 pmid: 9277561 |
| [16] |
Cheng HS, Ton SH, Phang S, et al. Increased susceptibility of post-weaning rats on high-fat diet to metabolic syndrome[J]. J Adv Res, 2017,8(6):743-752.
pmid: 29062573 |
| [17] | Giles ED, Jackman MR, Maclean PS. Modeling diet-induced obesity with obesity-prone rats: Implications for studies in females[J]. Front Nutr, 2016,3(3):50. |
| [18] | Ghibaudi L, Cook J, Farley C, et al. Fat intake affects adiposity, comorbidity factors, and energy metabolism of sprague-dawley rats[J]. Obes Res, 2002,10(9):956-963. |
| [19] |
Chalkley SM, Hettiarachchi M, Chisholm DJ, et al. Long-term high-fat feeding leads to severe insulin resistance but not diabetes in Wistar rats[J]. Am J Physiol Endocrinol Metab, 2002,282(6):E1231-E1238.
pmid: 12006352 |
| [20] | Malvi P, Piprode V, Chaube B, et al. High fat diet promotes achievement of peak bone mass in young rats[J]. Biochem Biophys Res Commun, 2014,455(1-2):133-138. |
| [21] | Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease[J]. J Clin Invest, 2011,121(6):2111-2117. |
| [22] |
Karalis KP, Giannogonas P, Kodela E, et al. Mechanisms of obesity and related pathology: Linking immune responses to metabolic stress[J]. FEBS J, 2009,276(20):5747-5754.
pmid: 19754872 |
| [23] | Hotamisligil GS. Inflammatory pathways and insulin action[J]. Int J Obes Relat Metab Disord, 2003,27(Suppl 3):S53-55. |
| [24] | Shapiro H, Lutaty A, Ariel A. Macrophages, meta-inflammation, and immuno-metabolism[J]. Scientific World J, 2011,11(6):2509-2529. |
| [1] | 金江, 陈雪, 赵琰, 贾军, 张建中. 卵清蛋白诱导的特应性皮炎小鼠模型中白细胞介素-25的作用及其调控意义[J]. 北京大学学报(医学版), 2024, 56(5): 756-762. |
| [2] | 柯涵炜, 王起, 许克新. 优化环磷酰胺剂量在间质性膀胱炎/膀胱疼痛综合征啮齿动物模型中的应用[J]. 北京大学学报(医学版), 2024, 56(5): 908-912. |
| [3] | 郑生旗,花天池,殷桂草,张伟,姚曳,李一帆. 甘油三酯葡萄糖指数与男性肾结石风险的关联[J]. 北京大学学报(医学版), 2024, 56(4): 610-616. |
| [4] | 何海龙,李清,徐涛,张晓威. 构建显微精索手术治疗精索疼痛的术后疼痛缓解预测模型[J]. 北京大学学报(医学版), 2024, 56(4): 646-655. |
| [5] | 刘佐相,陈晓薇,赵厚宇,詹思延,孙凤. 真实世界中2型糖尿病患者二甲双胍联用西格列汀的心血管安全性[J]. 北京大学学报(医学版), 2024, 56(3): 424-430. |
| [6] | 周恬静,刘秋萍,张明露,刘晓非,康佳丽,沈鹏,林鸿波,唐迅,高培. 基于马尔科夫模型的社区人群启动降压药物治疗预防心血管病的策略比较[J]. 北京大学学报(医学版), 2024, 56(3): 441-447. |
| [7] | 苏俊琪,王晓颖,孙志强. 舌鳞状细胞癌根治性切除术后患者预后预测列线图的构建与验证[J]. 北京大学学报(医学版), 2024, 56(1): 120-130. |
| [8] | 刘欢锐,彭祥,李森林,苟欣. 基于HER-2相关基因构建风险模型用于膀胱癌生存预后评估[J]. 北京大学学报(医学版), 2023, 55(5): 793-801. |
| [9] | 张云静,乔丽颖,祁萌,严颖,亢伟伟,刘国臻,王明远,席云峰,王胜锋. 乳腺癌患者新发心血管疾病预测模型的建立与验证:基于内蒙古区域医疗数据[J]. 北京大学学报(医学版), 2023, 55(3): 471-479. |
| [10] | 张明露,刘秋萍,巩超,王佳敏,周恬静,刘晓非,沈鹏,林鸿波,唐迅,高培. 阿司匹林用于心血管病一级预防的不同策略比较:一项马尔可夫模型研究[J]. 北京大学学报(医学版), 2023, 55(3): 480-487. |
| [11] | 袁婷婷,李燊,吴燕,吴海涛. 长期自由选择饮酒小鼠模型的建立及其行为学评价[J]. 北京大学学报(医学版), 2023, 55(2): 315-323. |
| [12] | 高梓翔,王勇,温奥楠,朱玉佳,秦庆钊,张昀,王晶,赵一姣. 基于三维下颌骨平均模型的颌骨标志点自动确定方法[J]. 北京大学学报(医学版), 2023, 55(1): 174-180. |
| [13] | 孟令玮,李雪,高胜寒,李悦,曹瑞涛,张毅,潘韶霞. 三种方法建立大鼠种植体周炎模型的比较[J]. 北京大学学报(医学版), 2023, 55(1): 22-29. |
| [14] | 朱琳,张维宇,许克新. 环磷酰胺诱导SD大鼠膀胱疼痛综合征模型的有效性[J]. 北京大学学报(医学版), 2022, 54(4): 735-740. |
| [15] | 巩超,刘秋萍,王佳敏,刘晓非,张明露,杨瀚,沈鹏,林鸿波,唐迅,高培. 社区人群他汀干预策略预防心血管病效果的马尔可夫模型评价[J]. 北京大学学报(医学版), 2022, 54(3): 443-449. |
|
||