北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (4): 764-769. doi: 10.19723/j.issn.1671-167X.2021.04.024
垫底材料弹性模量对髓腔固位冠修复后上颌前磨牙应力分布的影响
- 北京大学口腔医学院·口腔医院,牙体牙髓科 国家口腔医学中心 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室,北京 100081
Influence of base materials on stress distribution in endodontically treated maxillary premolars restored with endocrowns
JIANG You-sheng,FENG Lin( ),GAO Xue-jun
),GAO Xue-jun
- Department of Cariology and Endodontology, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology,Beijing 100081, China
摘要:
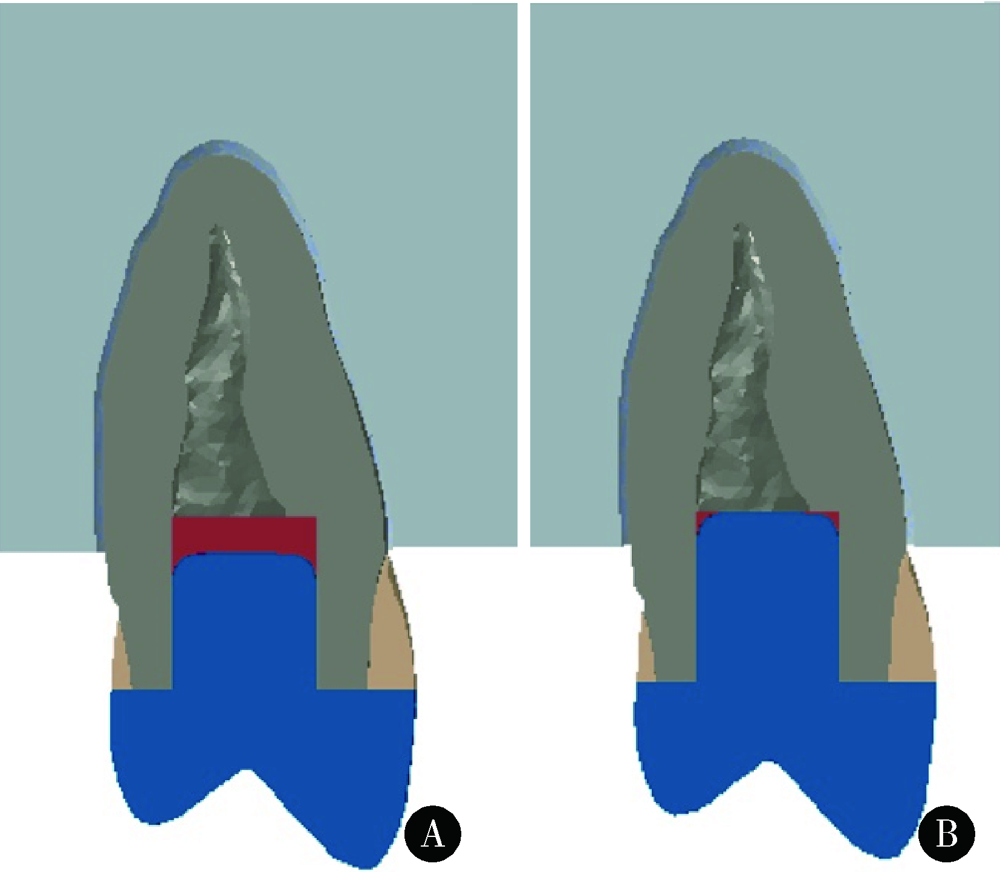
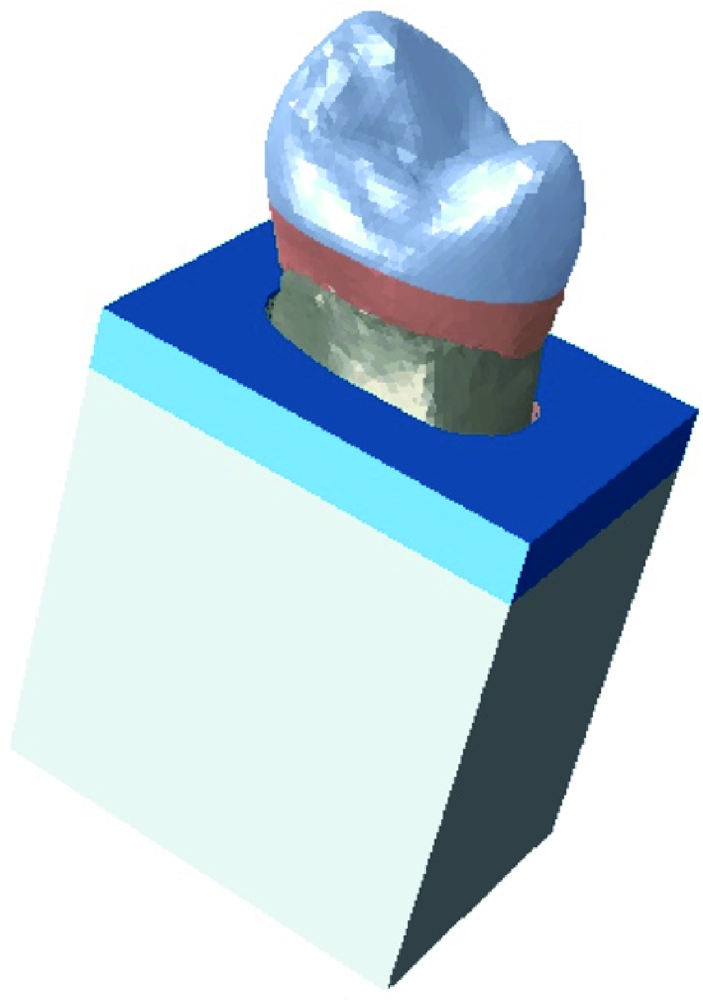
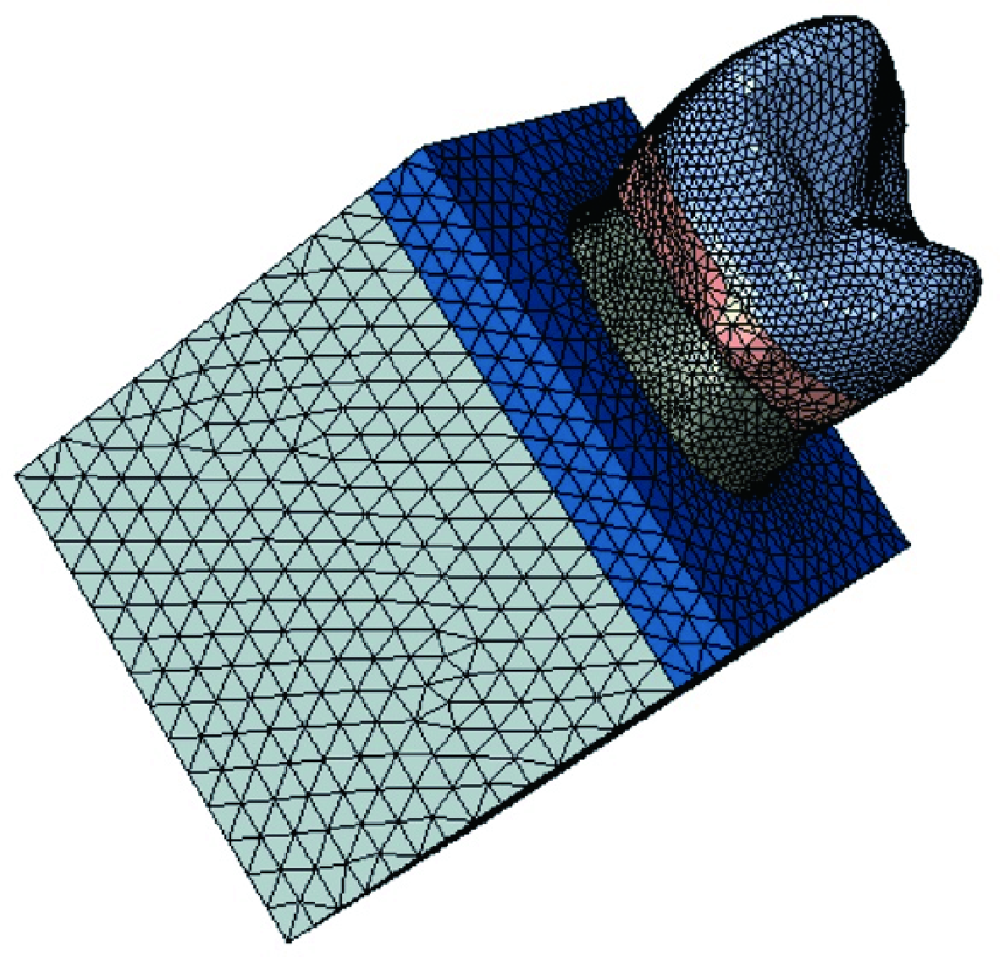
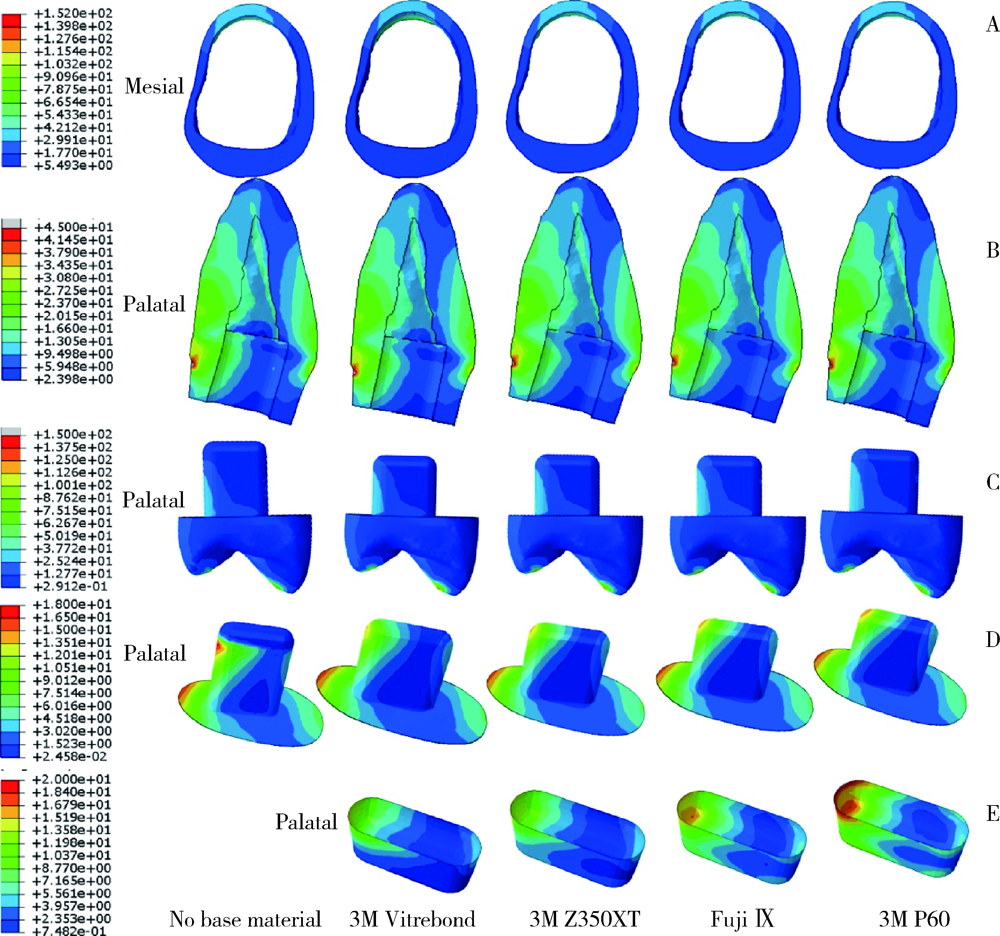
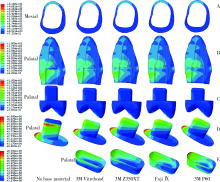
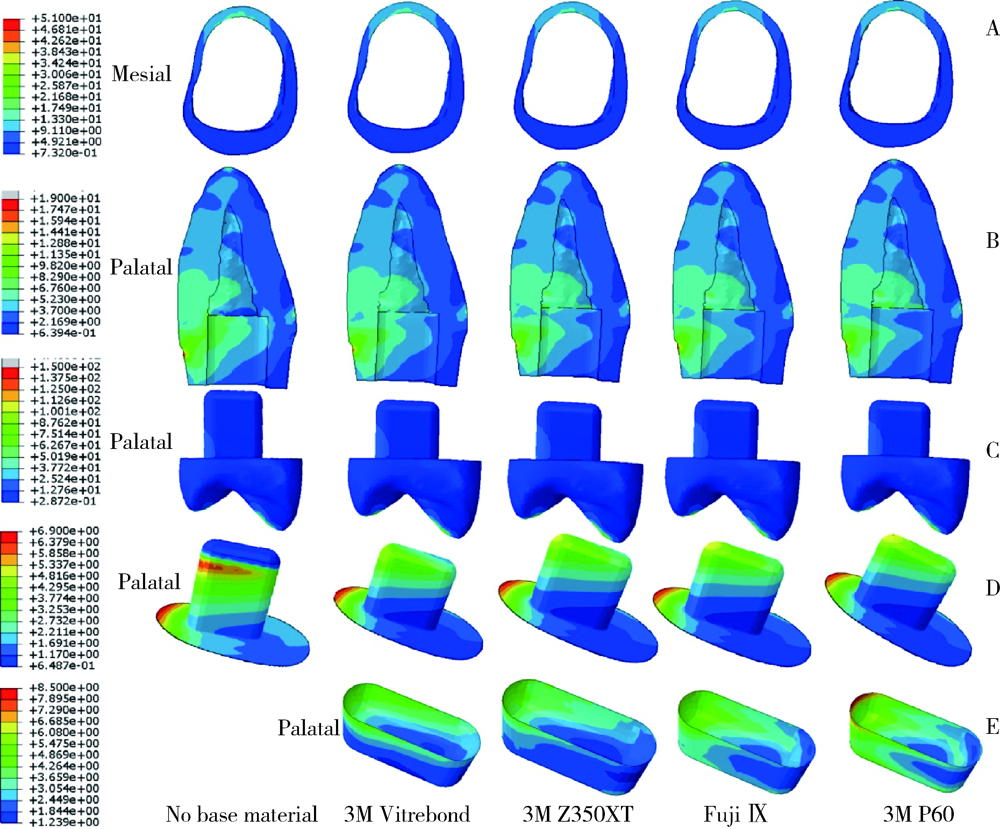
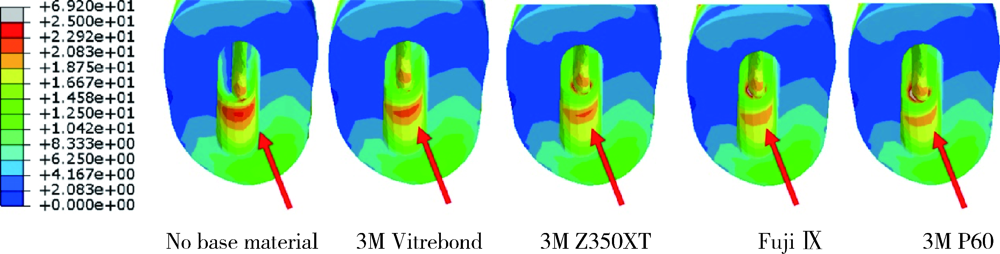
目的: 构建根管治疗后上颌前磨牙经髓腔固位冠修复后的三维有限元模型,分析髓室底垫底材料弹性模量对应力分布的影响。方法: 利用显微CT扫描逆向建立上颌第二前磨牙缺损的三维有限元模型,模拟髓腔固位冠进行修复。实验组采用4 种不同弹性模量的材料:光固化玻璃离子(3M Vitrebond)、流动树脂(3M Filtek Z350XT Flowable Restorative)、高强度玻璃离子(GC Fuji Ⅸ)和后牙复合树脂(3M Filtek P60)进行垫底,4 种不同类型材料的弹性模量依次是3 657、7 300、13 130、19 700 MPa。垫底厚度选择为1 mm,设无垫底材料修复为对照。采用轴向和侧向载荷(30°)分别加载200 N的力,观察应力分布情况,比较应力集中部位及应力峰值的差异。结果: 各模型牙本质和粘接层上的von Mises应力峰值(轴向/侧向加载时)如下:(1)无垫底材料时牙本质19.39/70.49 MPa,粘接层6.97/17.97 MPa;(2)光固化玻璃离子垫底时牙本质19.00/69.75 MPa,粘接层6.87/16.30 MPa;(3)流动树脂垫底时牙本质18.78/69.33 MPa,粘接层6.79/16.17 MPa;(4)高强度玻璃离子垫底时牙本质18.71/69.20 MPa,粘接层6.74/16.07 MPa;(5)后牙复合树脂垫底时牙本质18.61/69.03 MPa,粘接层6.70/16.01 MPa。具有不同弹性模量的垫底材料在相同加载条件下,在牙体组织上应力集中的部位相似,主要集中于牙颈部。侧向力加载时,应力集中的位置与轴向力时相比无明显变化,但应力值增加。有垫底层存在时,牙颈部的应力集中与无垫底层时相比缓解。随着垫底材料的弹性模量不断增加,逐渐接近牙本质的弹性模量,测得的剩余牙体组织及粘接层上的von Mises应力峰值下降。结论: 使用与牙本质弹性模量相近的后牙复合树脂类材料进行适宜厚度的粘接垫底,有利于缓解髓腔固位冠修复后上颌前磨牙牙颈部和粘接层的应力集中。
中图分类号:
- R782.1
| [1] |
Zelic K, Vukicevic A, Jovicic G, et al. Mechanical weakening of devitalized teeth: three-dimensional finite element analysis and prediction of tooth fracture [J]. Int Endod J, 2015, 48(9):850-863.
doi: 10.1111/iej.12381 pmid: 25243348 |
| [2] | 包旭东. 椅旁计算机辅助设计与辅助制作嵌体冠粘接修复大面积缺损根管治疗牙的利与弊 [J]. 中华口腔医学杂志, 2018, 53(4):221-225. |
| [3] |
Bindl A, Mörmann WH. Clinical evaluation of adhesively placed Cerec endo-crowns after 2 years-preliminary results [J]. J Adhes Dent, 1999, 1(3):255-265.
pmid: 11725673 |
| [4] | 李智, 高承志, 许永伟, 等. 铸造陶瓷高嵌体修复根管治疗后前磨牙的3年临床效果观察 [J]. 华西口腔医学杂志, 2015, 33(3):263-266. |
| [5] |
Belleflamme MM, Geerts SO, Louwette MM, et al. No post-nocore approach to restore severely damaged posterior teeth: An up to 10-year retrospective study of documented endocrown cases [J]. J Dent, 2017, 63:1-7.
doi: S0300-5712(17)30093-3 pmid: 28456557 |
| [6] | 冯娟, 郭慧慧, 申晋斌, 等. 磨牙髓室底垫底厚度对全瓷嵌体冠应力分布的影响 [J]. 牙体牙髓牙周病学杂志, 2017, 27(1):16-21. |
| [7] | 王惠芸. 我国人牙的测量和统计 [J]. 中华口腔科杂志, 1959, 7(3):149-155. |
| [8] | 张丹, 白保晶, 张振庭. 垫底厚度对全瓷嵌体修复应力分布影响的三维有限元分析 [J]. 北京口腔医学, 2015, 23(2):105-108. |
| [9] |
Ilie N, Hickel R. Investigations on a methacrylate-based flowable composite based on the TM technology [J]. Dent Mater, 2011, 27(4):348-355.
doi: 10.1016/j.dental.2010.11.014 |
| [10] |
Yap AUJ, Wang X, Wu X, et al. Comparative hardness and modulus of tooth-colored restoratives: A depth-sensing microindentation study [J]. Biomaterials, 2004, 25(11):2179-2185.
doi: 10.1016/j.biomaterials.2003.09.003 |
| [11] |
Papadogiannis DY, Lakes RS, Papadogiannis Y, et al. The effect of temperature on the viscoelastic properties of nano-hybrid composites [J]. Dent Mater, 2008, 24(2):257-266.
pmid: 17640723 |
| [12] |
Zhu J, Rong Q, Wang X, et al. Influence of remaining tooth structure and restorative material type on stress distribution in endodontically treated maxillary premolars: A finite element analysis [J]. J Prosthet Dent, 2017, 117(5):646-655.
doi: 10.1016/j.prosdent.2016.08.023 |
| [13] |
Coldea A, Fischer J, Swain MV, et al. Damage tolerance of indirect restorative materials (including PICN) after simulated bur adjustments [J]. Dent Mater, 2015, 31(6):684-694.
doi: 10.1016/j.dental.2015.03.007 |
| [14] |
Chung SM, Yap AUJ, Koh WK, et al. Measurement of Poisson’s ratio of dental composite restorative materials [J]. Biomaterials, 2004, 25(13):2455-2460.
pmid: 14751729 |
| [15] | 冯瑞明, 薛明. 根管治疗后牙体粘接修复前的髓腔处理 [J]. 中国实用口腔科杂志, 2017, 10(4):193-197. |
| [16] |
Farah JW, Powers JM, Dennison JB, et al. Effects of cement bases on the stresses and deflections in composite restorations [J]. J Dent Res, 1976, 55(1):115-120.
pmid: 1060645 |
| [17] |
Yamamoto T, Takeishi S, Momoi Y. Finite element stress analysis of indirect restorations prepared in cavity bases [J]. Dent Mater J, 2007, 26(2):274-279.
doi: 10.4012/dmj.26.274 |
| [1] | 欧蒙恩,丁云,唐卫峰,周永胜. 基台边缘-牙冠的平台转移结构中粘接剂流动的三维有限元分析[J]. 北京大学学报(医学版), 2023, 55(3): 548-552. |
| [2] | 李智,徐永祥,包旭东,王晓燕. 垫底树脂和固位深度对树脂基纳米陶瓷髓腔固位冠修复磨牙抗折性能的影响[J]. 北京大学学报(医学版), 2022, 54(1): 95-99. |
| [3] | 马珂楠,陈虎,沈妍汝,周永胜,王勇,孙玉春. 选择性激光熔化打印可摘局部义齿圆环形卡环固位力的有限元分析[J]. 北京大学学报(医学版), 2022, 54(1): 105-112. |
| [4] | 周伟,安金刚,荣起国,张益. 下颌骨颏部骨折联合双侧髁突囊内骨折致伤机制的三维有限元分析[J]. 北京大学学报(医学版), 2021, 53(5): 983-989. |
| [5] | 任爽,时会娟,张家豪,刘振龙,邵嘉艺,朱敬先,胡晓青,黄红拾,敖英芳. 前交叉韧带重建术后移植物应力的有限元分析[J]. 北京大学学报(医学版), 2021, 53(5): 865-870. |
| [6] | 林春平,卢松鹤,朱浚鑫,胡洪成,岳兆国,唐志辉. 个性化根形种植体的螺纹形态对周围牙槽骨应力分布影响的三维有限元分析[J]. 北京大学学报(医学版), 2019, 51(6): 1130-1137. |
| [7] | 付宏宇,王芳芳,侯晓玫. 控制记忆合金丝镍钛根管锉弯曲性能有限元分析模型的构建及力学分析[J]. 北京大学学报(医学版), 2019, 51(1): 131-135. |
| [8] | 柳大为,李晶,郭亮,荣起国,周彦恒. 舌侧矫治器关闭间隙上前牙牙周膜应力变化的三维有限元分析[J]. 北京大学学报(医学版), 2018, 50(1): 141-147. |
| [9] | 孙丽颖,郭阳,荣起国,田光磊. 舟骨骨折术后康复治疗的有限元分析[J]. 北京大学学报(医学版), 2016, 48(4): 751-封三. |
| [10] | 赵旭, 张磊, 孙健, 杨振宇,谢秋菲. 后牙种植体支持单冠牙合面高度的三维有限元力学分析[J]. 北京大学学报(医学版), 2016, 48(1): 94-100. |
| [11] | 甄敏,胡文杰,荣起国. 上颌中切牙冠根折行冠延长术并桩核冠修复的三维有限元分析[J]. 北京大学学报(医学版), 2015, 47(6): 1015-1021. |
| [12] | 周团锋, 张相皞, 王新知. 一体化计算机辅助设计与制作氧化锆桩核的三维有限元分析[J]. 北京大学学报(医学版), 2015, 47(1): 78-84. |
| [13] | 杨雪, 荣起国, 杨亚东. 附着体类型对种植支持可摘局部义齿应力分布的影响[J]. 北京大学学报(医学版), 2015, 47(1): 72-77. |
| [14] | 刘海鹰,王捷夫,朱震奇. 融合与Topping-off术对腰椎影响的有限元分析[J]. 北京大学学报(医学版), 2013, 45(5): 723-727. |
| [15] | 刘诗铭, 刘玉华, 徐军. 牙槽骨高度对上颌前磨牙桩核冠修复后应力分布的影响[J]. 北京大学学报(医学版), 2013, 45(1): 44-49. |
|
||