北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (4): 704-710. doi: 10.19723/j.issn.1671-167X.2025.04.012
病理T3a期肾细胞癌肾部分切除与根治性肾切除的回顾性匹配研究
周泽臻, 葛力源, 张帆, 邓绍晖, 颜野, 张洪宪, 王国良, 刘磊, 黄毅, 张树栋*( )
)
- 北京大学第三医院泌尿外科,北京 100191
A retrospective matching study of partial nephrectomy and radical nephrectomy for pathological T3a stage renal cell carcinoma
Zezhen ZHOU, Liyuan GE, Fan ZHANG, Shaohui DENG, Ye YAN, Hongxian ZHANG, Guoliang WANG, Lei LIU, Yi HUANG, Shudong ZHANG*( )
)
- Department of Urology, Peking University Third Hospital, Beijing 100191, China
摘要:
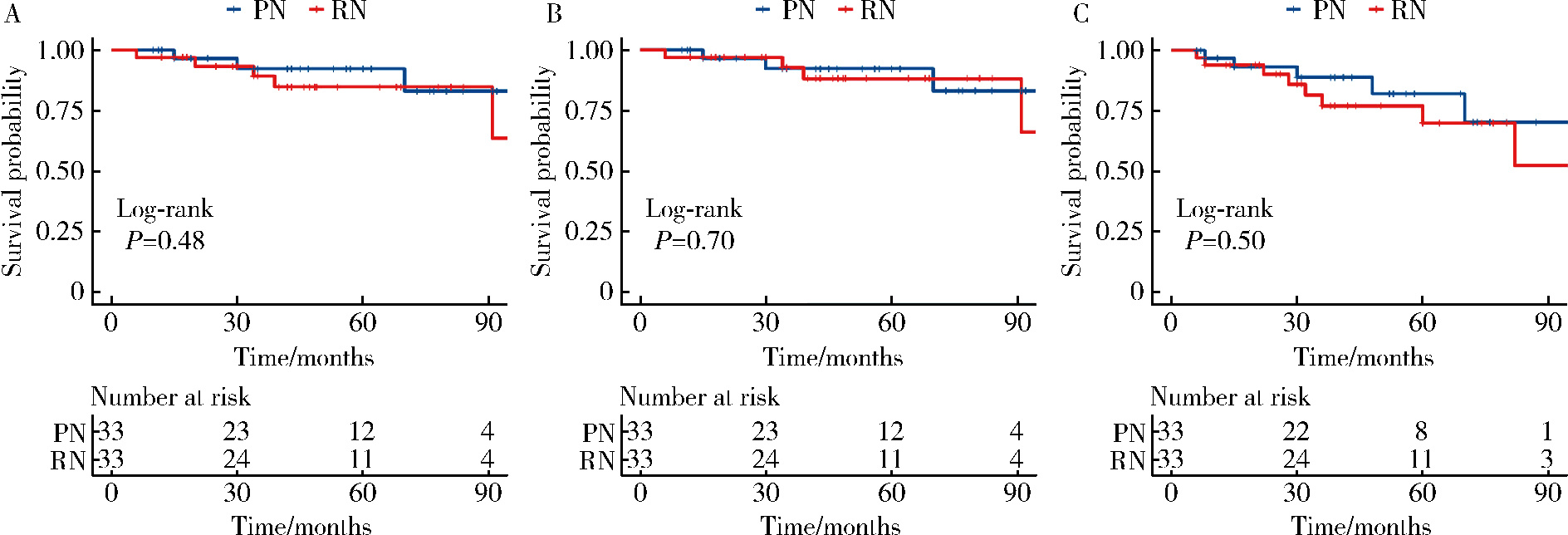
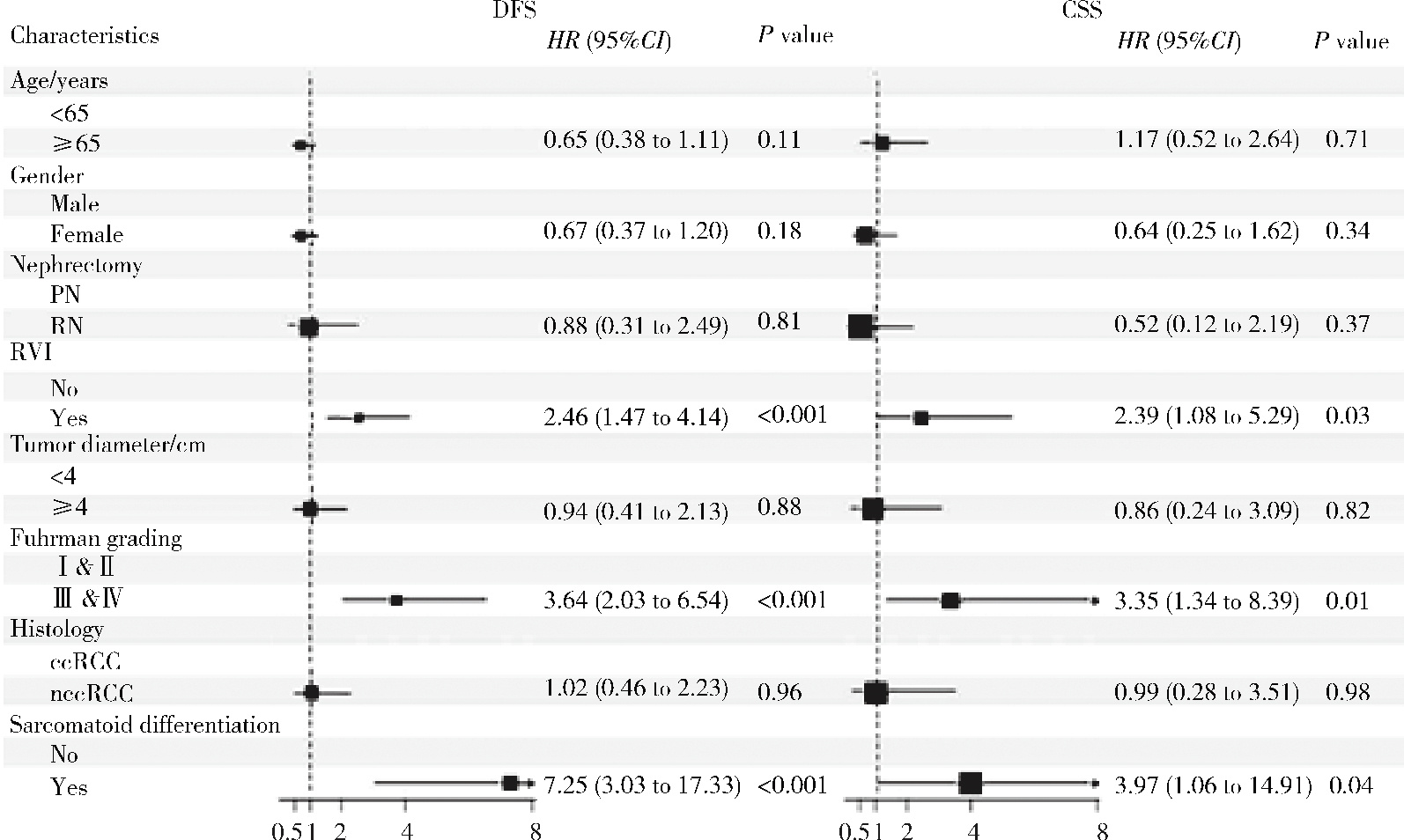
目的: 评估临床T1(clinical T1,cT1)期术后升级为病理T3a(pathological T3a,pT3a)期肾细胞癌(renal cell carcinoma,RCC) 患者应用肾部分切除术(partial nephrectomy,PN)的远期肿瘤学结局。方法: 回顾研究北京大学第三医院2013年2月至2022年12月427例术后评估为pT3aN0M0期的RCC患者,其中33例cT1术后升级为pT3a的RCC患者均接受了PN(PN组),而394例术后未升级的pT3a RCC患者均接受了根治性肾切除术(radical nephrectomy,RN,RN组),根据基线特征以1 ∶ 1的比例进行倾向性评分匹配,使用Kalan-Meier曲线评估总生存期(overall survival, OS)、癌症特异性生存期(cancer-specific survival, CSS)和无病生存期(disease-free survival, DFS),并使用对数秩检验和Cox回归模型进行多因素分析。结果: 匹配前,PN组(n = 33)与RN组(n = 394)相比,肾周脂肪浸润(perirenal fat invasion,PFI; 45.5% vs. 15.2%)和肾段静脉受累(42.4% vs. 20.8%)的比例更高,而肾盂肾窦侵犯(renal sinus invasion,RSI; 21.2% vs. 73.6%)及合并肾静脉癌栓(0% vs. 15.2%)的比例较低,差异有统计学意义(P < 0.05)。匹配后,PN组(n = 33)和RN组(n = 33)的基线特征具有可比性。PN和RN组在手术时间、出血量、平均住院日、并发症发生率、阳性切缘率、中转开放手术的比例方面差异无统计学意义(P >0.05),但PN组术后估算的肾小球滤过率(estimated glomerular filtration rate,eGFR)更高[76.9 (55.4,87.3) mL/(min·1.73 m2) vs. 61.7 (56.8,73.5) mL/(min·1.73 m2),P < 0.05],表明其对肾功能的保留效果更好。两组在OS、CSS和DFS方面差异无统计学意义(P >0.05)。多因素分析显示,肾静脉侵犯(renal vein invasion,RVI)、较高的肿瘤Fuhrman分级(Ⅲ~Ⅳ)以及伴有肉瘤样分化特征是pT3a RCC患者的DFS和CSS的独立危险因素(P < 0.05)。结论: 对于cT1升级为pT3a的RCC患者,PN在更大程度上保留了肾功能,并且肿瘤学结局可能与RN的效果相当。RVI、较高的肿瘤Fuhrmann分级以及伴有肉瘤样分化特征是pT3N0M0期RCC患者的独立危险因素。
中图分类号:
- R737.11
| 1 |
|
| 2 |
|
| 3 |
|
| 4 |
|
| 5 |
|
| 6 |
|
| 7 |
|
| 8 |
白红松, 王栋, 寿建忠, 等. cT1期肾癌行肾部分切除术后升期为pT3a期的临床分析[J]. 临床泌尿外科杂志, 2020, 35 (9): 716- 720.
|
| 9 |
|
| 10 |
|
| 11 |
|
| 12 |
|
| 13 |
|
| 14 |
|
| 15 |
Yang Z, Li J, Liu Z, et al. The effectiveness of partial versus radical nephrectomy for pT3aN0M0 renal cell carcinoma: A propensity score analysis[J]. 2020, 46(10): 1234-1256.
|
| 16 |
|
| 17 |
|
| 18 |
|
| 19 |
|
| 20 |
|
| 21 |
|
| 22 |
周泽臻, 邓绍晖, 颜野, 等. 非转移性T3a肾细胞癌患者3年肿瘤特异性生存期预测[J]. 北京大学学报(医学版), 2024, 56 (4): 673- 679.
doi: 10.19723/j.issn.1671-167X.2024.04.021 |
| 23 |
|
| 24 |
|
| 25 |
|
| 26 |
|
| 27 |
|
| 28 |
|
| [1] | 郭博达, 陆敏, 王国良, 张洪宪, 刘磊, 侯小飞, 赵磊, 田晓军, 张树栋. 肾透明细胞癌与非透明细胞癌伴静脉癌栓患者的临床病理特征及预后比较[J]. 北京大学学报(医学版), 2025, 57(4): 644-649. |
| [2] | 张展奕, 陆敏, 孙悦皓, 董靖晗, 侯小飞, 肖春雷, 王国良, 田晓军, 马潞林, 张洪宪, 张树栋. TFE3重排肾细胞癌合并静脉癌栓患者的临床病理特征及生存分析[J]. 北京大学学报(医学版), 2025, 57(4): 650-661. |
| [3] | 陈克伟,刘茁,邓绍晖,张帆,叶剑飞,王国良,张树栋. 肾血管平滑肌脂肪瘤伴下腔静脉瘤栓的临床诊治[J]. 北京大学学报(医学版), 2024, 56(4): 617-623. |
| [4] | 舒帆,郝一昌,张展奕,邓绍晖,张洪宪,刘磊,王国良,田晓军,赵磊,马潞林,张树栋. 肾部分切除术治疗囊性肾癌的功能学和肿瘤学结果:单中心回顾性研究[J]. 北京大学学报(医学版), 2024, 56(4): 667-672. |
| [5] | 周泽臻,邓绍晖,颜野,张帆,郝一昌,葛力源,张洪宪,王国良,张树栋. 非转移性T3a肾细胞癌患者3年肿瘤特异性生存期预测[J]. 北京大学学报(医学版), 2024, 56(4): 673-679. |
| [6] | 邱敏,宗有龙,王滨帅,杨斌,徐楚潇,孙争辉,陆敏,赵磊,卢剑,刘承,田晓军,马潞林. 腹腔镜肾部分切除术治疗中高复杂程度肾肿瘤的效果[J]. 北京大学学报(医学版), 2023, 55(5): 833-837. |
| [7] | 沈棋,刘亿骁,何群. 肾黏液样小管状和梭形细胞癌的临床病理特点及预后[J]. 北京大学学报(医学版), 2023, 55(2): 276-282. |
| [8] | 许云屹,苏征征,郑林茂,张孟尼,谭珺娅,杨亚蓝,张梦鑫,徐苗,陈铌,陈雪芹,周桥. 转录通读环状RNA rt-circ-HS促进低氧诱导因子1α表达和肾癌细胞增殖与侵袭[J]. 北京大学学报(医学版), 2023, 55(2): 217-227. |
| [9] | 张铨,宋海峰,马冰磊,张喆楠,周朝晖,李傲林,刘军,梁磊,朱时雨,张骞. 术前预后营养指数可作为预测非转移性肾细胞癌预后的指标[J]. 北京大学学报(医学版), 2023, 55(1): 149-155. |
| [10] | 博尔术,洪鹏,张宇,邓绍晖,葛力源,陆敏,李楠,马潞林,张树栋. 乳头状肾细胞癌的临床病理特征和预后分析[J]. 北京大学学报(医学版), 2022, 54(4): 615-620. |
| [11] | 周鑫,李文智. 肾细胞癌极致保肾时代的冷思考[J]. 北京大学学报(医学版), 2022, 54(4): 595-598. |
| [12] | 田雨,程晓悦,贺慧颖,王国良,马潞林. 肾细胞癌合并尿路瘤栓的临床病理特征: 6例报道及文献回顾[J]. 北京大学学报(医学版), 2021, 53(5): 928-932. |
| [13] | 韩松辰,黄子雄,刘慧鑫,徐涛. 单侧肾细胞癌根治性切除术后的肾功能代偿[J]. 北京大学学报(医学版), 2021, 53(4): 680-685. |
| [14] | 赵勋,颜野,黄晓娟,董靖晗,刘茁,张洪宪,刘承,马潞林. 癌栓粘连血管壁对非转移性肾细胞癌合并下腔静脉癌栓患者手术及预后的影响[J]. 北京大学学报(医学版), 2021, 53(4): 665-670. |
| [15] | 孙争辉,黄晓娟,董靖晗,刘茁,颜野,刘承,马潞林. 临床T1期肾细胞癌肾窦侵犯的危险因素[J]. 北京大学学报(医学版), 2021, 53(4): 659-664. |
|
||