北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (1): 159-164. doi: 10.19723/j.issn.1671-167X.2019.01.027
脐动脉血气pH值对剖宫产新生儿住院期间并发症的预测价值
- 1. 北京大学第一医院 麻醉科,北京 100034
2. 北京大学第一医院 手术室, 北京 100034
Predictive value of umbilical arterial cord pH on complications during hospitalization in neonates after cesarean section
Ju BAO1,Jia LIU2,Yuan QU1,Dong-liang MU1,△( )
)
- 1. Department of Anesthesiology,Peking University First Hospital,Beijing 100034, China
2. Department of Operation Room,Peking University First Hospital,Beijing 100034, China
摘要:
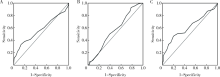
目的:分析脐动脉血气pH值对剖宫产新生儿住院期间并发症的预测价值。方法:本研究为回顾性队列研究,选择2017年1月1日至6月30日在北京大学第一医院剖宫产娩出并完成脐动脉血气分析的新生儿为研究对象,主要观察终点是新生儿住院期间并发症发生率。按照新生儿是否发生住院期间并发症将研究对象分为两组,比较两组间脐动脉血气pH值。收集母婴围产期的资料和新生儿住院期间并发症的资料,采用ROC曲线分析脐动脉血气pH对新生儿住院期间并发症的预测价值。结果:共纳入872例新生儿(择期541例、急诊331例),新生儿住院期间并发症的总体发生率为14.1%,其中发生率最高的3项分别为感染、吸入性肺炎及心肌损伤。无并发症组pH值平均为7.31,有并发症组pH值平均为7.29,组间比较差异有统计学意义(P<0.001)。本研究中pH≤7.20的总体比例为3.1%(27/872),其中无并发症组pH值≤7.20的比例为1.6%(12/749),有并发症组pH值≤7.20的比例为12.2%(15/123),组间比较差异有统计学意义(P<0.001)。多因素Logistic回归分析显示,早产(OR=8.224, 95%CI: 4.910~13.777, P<0.001)、妊娠期高血压(OR=1.886, 95%CI: 1.004~3.546, P=0.049)、宫内生长受限(OR=4.429, 95%CI: 1.280~15.330, P=0.019)、急诊剖宫产(OR=2.711, 95%CI: 1.682~4.369, P<0.001)、脐动脉血气pH值≤7.20(OR=7.420, 95%CI: 2.951~18.655, P<0.001)及5分钟Apgar评分小于10分(OR=11.849, 95%CI: 3.977~35.128, P<0.001)是新生儿发生住院期间并发症的危险因素。脐动脉血气pH值预测全部新生儿、择期新生儿及急诊新生儿住院并发症的ROC曲线下面积分别为0.570(95%CI: 0.508~0.633, P=0.012)、0.559(95%CI: 0.465~0.652, P=0.189)及0.617(95%CI: 0.538~0.697, P=0.002)。结论:脐动脉血气pH值≤7.2与剖宫产新生儿住院并发症发生率增加有相关性,但是ROC分析显示其预测价值较低。
中图分类号:
- R722.1
| [1] |
Yildiz EP, Tatli B, Ekici B , et al. Evaluation of etiologic and prognostic factors in neonatal convulsions[J]. Pediatr Neurol, 2012,47(3):186-192.
doi: 10.1016/j.pediatrneurol.2012.05.015 pmid: 22883283 |
| [2] |
Elmahdy H, El-Mashad AR, EI-Bathrawy H , et al. Human recombinant erythropoietin in asphyxia neonatorum: pilot trial[J]. Pediatrics, 2010,125(5):e1135-e1142.
doi: 10.1542/peds.2009-2268 pmid: 20385632 |
| [3] |
张燕妮, 牟红梅 . 新生儿窒息126例临床分析[J]. 中国妇幼健康研究, 2016,27(11):1370-1372.
doi: 10.3969/j.issn.1673-5293.2016.11.025 |
| [4] |
ACOG Committee on Obstetric Practice. ACOG Committee Opi-nion No. 348, November 2006: Umbilical cord blood gas and acid-base analysis[J]. Obstet Gynecol, 2006,108(5):1319-1322.
doi: 10.1097/00006250-200611000-00058 |
| [5] |
Whitelaw A, Thoresen M . Clinical trials of treatments after perinatal asphyxia[J]. Curr Opin Pediatr, 2002,14(6):664-668.
doi: 10.1097/00008480-200212000-00002 pmid: 12436031 |
| [6] |
Neilson JP . Umbilical cord blood gas analysis[J]. BMJ, 2010(340):c1720.
doi: 10.1016/S0889-8545(05)70107-8 pmid: 20466790 |
| [7] |
Ahmadpour-Kacho M, Asnafi N, Javadian M , et al. Correlation between umbilical cord pH and Apgar score in high-risk pregnancy[J]. Iran J Pediatr, 2010,20(4):401-406.
doi: 10.1007/s13312-010-0170-7 pmid: 23056738 |
| [8] |
White CR, Doherty DA, Henderson JJ , et al. Benefits of introducing universal umbilical cord blood gas and lactate analysis into an obstetric unit[J]. Aust N Z J Obstet Gynaecol, 2010,50(4):318-328.
doi: 10.1111/j.1479-828X.2010.01192.x pmid: 20716258 |
| [9] |
White CR, Doherty DA, Cannon JW , et al. Cost effectiveness of universal umbilical cord blood gas and lactate analysis in a tertiary level maternity unit[J]. J Perinat Med, 2016,44(5):573-584.
doi: 10.1515/jpm-2015-0398 pmid: 26966927 |
| [10] |
Wiklund I, Ahlberg M, Dahlström A , et al. Routine testing of umbilical cord blood after normal delivery should be discontinued[J]. Sex Reprod Healthc, 2014,5(4):165-166.
doi: 10.1016/j.srhc.2014.10.002 pmid: 25433824 |
| [11] |
Kutuk MS, Yikilmaz A, Ozgun MT , et al. Prenatal diagnosis and postnatal outcome of fetal intracranial hemorrhage[J]. Childs Nerv Syst, 2014,30(3):411-418.
doi: 10.1007/s00381-013-2243-0 pmid: 23907139 |
| [12] |
Caffrey Osvald E, Prentice P . NICE clinical guideline:antibiotics for the prevention and treatment of early-onset neonatal infection[J]. Arch Dis Child Educ Pract Ed, 2014,99(3):98-100.
doi: 10.1136/archdischild-2013-304629 pmid: 24334339 |
| [13] |
Mortier I, Blanc J, Tosello B , et al. Is gestational diabetes an independent risk factor of neonatal severe respiratory distress syndrome after 34 weeks of gestation? A prospective study[J]. Arch Gynecol Obstet, 2017,296(6):1071-1077.
doi: 10.1007/s00404-017-4505-7 pmid: 28948345 |
| [14] |
Eaton S . Necrotizing enterocolitis symposium:Epidemiology and early diagnosis[J]. J Pediatr Surg, 2017,52(2):223-225.
doi: 10.1016/j.jpedsurg.2016.11.013 pmid: 27914586 |
| [15] |
Sabol BA, Caughey AB . Acidemia in neonates with a 5-minute Apgar score of 7 or greater. What are the outcomes? [J]. Am J Obstet Gynecol, 2016, 215(4): 486. e1-e6.
doi: 10.1016/S0002-9378(16)30277-0 |
| [16] |
Malin GL, Morris RK, Khan KS . Strength of association between umbilical cord pH and perinatal and long-term outcomes:systema-tic review and meta-analysis[J]. BMJ, 2010(340):c1471.
doi: 10.1097/01.aoa.0000397115.97213.02 pmid: 20466789 |
| [17] |
Zanardo V, Dal Cengio V, Parotto M , et al. Elective caesarean delivery adversely affects preductal oxygen saturation during birth transition[J]. Arch Dis Child Fetal Neonatal Ed, 2016,101(4):F339-F343.
doi: 10.1136/archdischild-2015-308304 pmid: 26644392 |
| [18] |
Yeh P, Emary K, Impey L . The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: analysis of 51 519 consecutive validated samples[J]. BJOG, 2012,119(7):824-831.
doi: 10.1111/j.1471-0528.2012.03335.x pmid: 22571747 |
| [19] |
Cahill AG, Mathur AM, Smyser CD , et al. Neurologic injury in acidemic term infants[J]. Am J Perinatol, 2017,34(7):668-675.
doi: 10.1055/s-0036-1597135 pmid: 27926973 |
| [20] |
Low JA, Lindsay BG, Derrick EJ . Threshold of metabolic acidosis associated with newborn complications[J]. Am J Obstet Gynecol, 1997,177(6):1391-1394.
doi: 10.1016/S0002-9378(97)70080-2 pmid: 9423740 |
| [21] |
中华医学会妇产科学分会妊娠期高血压疾病学组. 妊娠期高血压疾病诊治指南(2015)[J]. 中华产科急救电子杂志, 2015,4(4):206-213.
doi: 10.3760/cma.j.issn.0529-567x.2015.10.001 |
| [22] |
Allen MC, Cristofalo EA, Kim C . Outcomes of preterm infants:morbidity replaces mortality[J]. Clin Perinatol, 2011,38(3):441-454.
doi: 10.1016/j.clp.2011.06.011 pmid: 21890018 |
| [23] |
张春雨, 李蕊, 张大程 , 等. 脐血血气分析在早产儿窒息诊断中的价值及影响因素分析[J]. 中国妇幼保健, 2017,32(5):968-971.
doi: 10.7620/zgfybj.j.issn.1001-4411.2017.05.33 |
| [24] |
Low JA, Killen H, Derrick EJ . Antepartum fetal asphyxia in the preterm pregnancy[J]. Am J Obstet Gynecol, 2003,188(2):461-465.
doi: 10.1067/mob.2003.37 pmid: 12592256 |
| [25] |
Pallotto EK, Kilbride HW . Perinatal outcome and later implications of intrauterine growth restriction[J]. Clin Obstet Gynecol, 2006,46(2):257-269.
doi: 10.1097/00003081-200606000-00008 pmid: 16721105 |
| [26] |
Unterscheider J, O’Donoghue K, Daly S, , et al. Fetal growth restriction and the risk of perinatal mortality-case studies from the multicenter PORTO study[J]. BMC Pregnancy Childbirth, 2014(14):63.
doi: 10.1186/1471-2393-14-63 pmid: 3923738 |
| [27] |
Razaz N, Boyce WT, Brownell M , et al. Five-minute Apgar score as a marker for developmental vulnerability at 5 years of age[J]. Arch Dis Child Fetal Neonatal Ed, 2016,101(2):F114-F120.
doi: 10.1136/archdischild-2015-308458 |
| [28] |
Persson M, Razaz N, Tedroff K , et al. Five and 10 minute Apgar scores and risks of cerebral palsy and epilepsy:population based cohort study in Sweden[J]. BMJ, 2018(360):k207.
doi: 10.1136/bmj.k207 pmid: 29437691 |
| [29] |
徐娜, 马挺, 田肇隆 , 等. 剖宫产术中仰卧位低血压综合征对新生儿脐血血气分析的影响[J]. 首都医科大学学报, 2009,30(3):393-395.
doi: 10.3969/j.issn.1006-7795.2009.03.030 |
| [1] | 金江, 陈雪, 赵琰, 贾军, 张建中. 卵清蛋白诱导的特应性皮炎小鼠模型中白细胞介素-25的作用及其调控意义[J]. 北京大学学报(医学版), 2024, 56(5): 756-762. |
| [2] | 焦莶如, 龚潘, 牛悦, 徐兆, 周宗朴, 杨志仙. 以婴儿癫痫性痉挛综合征为表型的吡哆醇依赖性癫痫[J]. 北京大学学报(医学版), 2024, 56(5): 781-787. |
| [3] | 钟华, 李原, 徐丽玲, 白明欣, 苏茵. 18F-FDG PET/CT在风湿免疫病中的应用[J]. 北京大学学报(医学版), 2024, 56(5): 853-859. |
| [4] | 周庆欣,杨晴晴,石舒原,李沛,孙凤. 健康体检人群血尿酸与气流阻塞的相关性[J]. 北京大学学报(医学版), 2024, 56(4): 693-699. |
| [5] | 马会超,李军,王永清. 妊娠合并炎症性肠病的临床特点[J]. 北京大学学报(医学版), 2024, 56(2): 260-266. |
| [6] | 任立敏,赵楚楚,赵义,周惠琼,张莉芸,王友莲,沈凌汛,范文强,李洋,厉小梅,王吉波,程永静,彭嘉婧,赵晓珍,邵苗,李茹. 系统性红斑狼疮低疾病活动度及缓解状况的真实世界研究[J]. 北京大学学报(医学版), 2024, 56(2): 273-278. |
| [7] | 苏俊琪,王晓颖,孙志强. 舌鳞状细胞癌根治性切除术后患者预后预测列线图的构建与验证[J]. 北京大学学报(医学版), 2024, 56(1): 120-130. |
| [8] | 李洋洋,侯林,马紫君,黄山雅美,刘捷,曾超美,秦炯. 孕期因素与婴儿牛奶蛋白过敏的关系[J]. 北京大学学报(医学版), 2024, 56(1): 144-149. |
| [9] | 殳畅,韩烨,孙雨哲,杨再目,侯建霞. Ⅲ期牙周炎患者牙周基础治疗前后炎症性贫血相关指标的变化[J]. 北京大学学报(医学版), 2024, 56(1): 45-50. |
| [10] | 李文根,古晓东,翁锐强,刘苏东,陈超. 血浆外泌体miR-34-5p和miR-142-3p在系统性硬化症中的表达及临床意义[J]. 北京大学学报(医学版), 2023, 55(6): 1022-1027. |
| [11] | 冯璐,翟佳羽,赵金霞. IgG4相关性疾病患者就诊情况及其临床特征[J]. 北京大学学报(医学版), 2023, 55(6): 1028-1032. |
| [12] | 陈楚云,孙蓬飞,赵静,贾佳,范芳芳,王春燕,李建平,姜一梦,霍勇,张岩. 北京社区人群促红细胞生成素相关因素及其与10年心血管疾病风险的关系[J]. 北京大学学报(医学版), 2023, 55(6): 1068-1073. |
| [13] | 王子恺,莫佳丽,张蒙,廖纪萍. 2013—2020年北京市慢性阻塞性肺疾病急性加重女性住院患者的流行病学和住院费用分析[J]. 北京大学学报(医学版), 2023, 55(6): 1074-1081. |
| [14] | 冯敏,陈哲,程永静. 以十二指肠溃疡为突出表现的IgG4相关性疾病1例[J]. 北京大学学报(医学版), 2023, 55(6): 1125-1129. |
| [15] | 扶琼,叶霜. 嵌合抗原受体T细胞治疗在自身免疫疾病中的应用和思考[J]. 北京大学学报(医学版), 2023, 55(6): 953-957. |
|
||