北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (2): 283-287. doi: 10.19723/j.issn.1671-167X.2019.02.016
解剖型髓内钉和股骨近端防旋髓内钉治疗老年股骨转子间骨折的疗效比较
- 1. 宣城市人民医院骨科,安徽宣城 242000
2. 北京大学人民医院创伤骨科, 北京 100044
Comparison of the effects of two cephalomedullary nails (zimmer natural nail and proximal femoral nail antirotation) in treatment of elderly intertrochan teric fractures
Jian CHEN1,Cai-hong ZUO1,Cai-yi ZHANG1,Ming YANG2,Pei-xun ZHANG2,∆( )
)
- 1. Department of Orthopaedics, People’s Hospital of Xuancheng City, Xuancheng 242000, Anhui, China;
2. Department of Traumatology and Orthopaedics, Peking University People’s Hospital, Beijing 100044, China;
摘要:
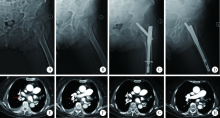
目的: 比较股骨近端防旋髓内钉(proximal femoral nail antirotation,PFNA)与解剖型髓内钉(zimmer natural nail,ZNN)治疗老年股骨转子间骨折的临床疗效,为临床选择围手术期的处理方式提供数据支撑。方法: 回顾性分析北京大学人民医院创伤骨科2016 年5 月 至2017 年5 月收治且获得完整随访的59例老年股骨转子间骨折患者资料,其中PFNA组28 例,ZNN组31 例。分析比较两组手术时间、术中出血量、骨折愈合时间、术后内固定并发症、术后尖顶距和末次随访髋关节评分。结果: 平均随访(10.8±4.0)个月(6~19 个月), PFNA组患者的手术时间为(62.7±14.2) min,术中出血量为(56.8±20.6) mL,骨折愈合时间为(4.6±0.8)个月,术后内固定并发症发生率为3.6%,术后尖顶距为(17.7±5.5) mm,末次随访髋关节评分为91.8±3.6。ZNN组手术时间为(73.6±18.3) min,术中出血量为(68.7±31.6) mL,骨折愈合时间为(4.5±0.7)个月,术后内固定并发症发生率为3.2%,术后尖顶距为(16.5±4.7) mm,末次随访髋关节评分为92.2±3.8。两组相比,PFNA组在手术时间方面较ZNN组短(P<0.05),而在其他评价指标,两组之间差异均无统计学意义(P>0.05)。结论: PFNA和ZNN内固定术都是治疗老年股骨转子间骨折的有效术式,PFNA的操作更简捷;ZNN的前弓设计可能更适合部分股骨前弓弧度较大的患者。
中图分类号:
- R683
| [1] | Haidukewych GJ . Intertrochanteric fractures: ten tips to improve results[J]. J Bone Joint Surg Am, 2009,91(3):712-719. |
| [2] |
Roberts KC, Brox WT, Jevsevar DS , et al. Management of hip fractures in the elderly[J]. J Am Acad Orthop Surg, 2015,23(2):131-137.
doi: 10.5435/JAAOS-D-14-00432 |
| [3] |
Jensen JS . Classification of trochanteric fractures[J]. Acta Orthop Scand, 1980,51(5):803-810.
doi: 10.3109/17453678008990877 |
| [4] |
杨明, 张晓萌, 张培训 , 等. 经皮导入导针结合纯侧位透视简化股骨近端防旋髓内钉操作[J]. 北京大学学报(医学版), 2015,47(2):258-262.
doi: 10.3969/j.issn.1671-167X.2015.02.013 |
| [5] |
Stern R, Lübbeke A, Suva D , et al. Prospective randomised study comparing screw versus helical blade in the treatment of low-energy trochanteric fractures[J]. Int Orthop, 2011,35(12):1855-1861.
doi: 10.1007/s00264-011-1232-8 |
| [6] |
Harris WH . Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplast. An end-result study using a new method of result evaluation[J]. J Bone Joint Surg Am, 1969,51(4):737-755.
doi: 10.2106/00004623-196951040-00012 |
| [7] | Tucker A, Donnelly KJ, McDonald S , et al. The changing face of fractures of the hip in Northern Ireland: a 15-year review[J]. Bone Joint J, 2017,99B(9):1223-1231. |
| [8] | 张树, 张继源, 杨杜明 , 等. 矢状位不稳定转子间骨折的形态特征和复位技术[J]. 北京大学学报(医学版), 2017,49(2):236-241. |
| [9] | Chatterton BD, Moores TS, Ahmad S , et al. Cause of death and factors associated with early in-hospital mortality after hip fracture[J]. Bone Joint J, 2015,97B(2):246-251. |
| [10] |
Thaler HW, Gosch M, Kammerlander C . Orthogeriatrics: hip fracture and its implications[J]. Wien Med Wochenschr, 2013,163(19/20):433-434.
doi: 10.1007/s10354-013-0229-x |
| [11] |
Pedersen SJ, Borgbjerg FM, Schousboe B , et al. A comprehensive hip fracture program reduces complication rates and mortality[J]. J Am Geriatr Soc, 2008,56(10):1831-1838.
doi: 10.1111/jgs.2008.56.issue-10 |
| [12] |
Evaniew N, Bhandari M . Cochrane in CORR®: intramedullary nails for extracapsular hip fractures in adults (review)[J]. Clin Orthop Relat Res, 2015,473(3):767-774.
doi: 10.1007/s11999-014-4123-7 |
| [13] |
Shin YS, Chae JE, Kang TW , et al. Prospective randomized study comparing two cephalomedullary nails for elderly intertrochanteric fractures: Zimmer Natural nail versus proximal femoral femoral nail antirotation Ⅱ[J]. Injury, 2017,48(7):1550-1557.
doi: 10.1016/j.injury.2017.04.011 |
| [14] | 刘中邸, 徐海林, 陈建海 , 等. 解剖型股骨近端髓内钉治疗老年转子间骨折的初步疗效[J]. 中华老年骨科与康复电子杂志, 2017,3(5):265-269. |
| [15] |
Parmar DS, Porecha MM, Chudasama S . Long proximal femoral nails versus short proximal femoral nails for the management of proximal femoral fractures: a retrospective study of 124 patients[J]. Eur J Orthop Surg Traumatol, 2011,21(3):159-164.
doi: 10.1007/s00590-010-0683-8 |
| [16] |
Chang SM, Song DL, Ma Z , et al. Mismatch of the short straight cephalomedullary nail (PFNA-Ⅱ) with the anterior bow of the femur in an Asian population[J]. J Orthop Trauma, 2014,28(1):17-22.
doi: 10.1097/BOT.0000000000000022 |
| [17] |
戴尅戎, 戴闵, 郭晓山 , 等. 中国骨科大手术静脉血栓栓塞症预防指南[J]. 中华骨科杂志, 2016,36(2):65-71.
doi: 10.3760/cma.j.issn.0253-2352.2016.02.001 |
| [18] |
García-Fuster MJ, Fabia MJ, Furió E , et al. Should we look for silent pulmonary embolism in patients with deep venous thrombosis[J]. BMC Cardiovasc Disord, 2014,14(1):178.
doi: 10.1186/1471-2261-14-178 |
| [19] |
Nosher JL, Patel A, Jagpal S , et al. Endovascular treatment of pulmonary embolism: selective review of available techniques[J]. World J Radiol, 2017,9(12):426-437.
doi: 10.4329/wjr.v9.i12.426 |
| [20] |
Najafzadeh M, Kim SC, Patterson C , et al. Patients’ perception about risks and benefits of venous thromboembolism (VTE) after orthopedic surgery: a qualitative study[J]. BMC Musculoskelet Disord, 2015,16(1):1-8.
doi: 10.1186/s12891-015-0454-0 |
| [21] |
Hou G, Zhou F, Tian Y , et al. Predicting the need for blood transfusions in elderly patients with pertrochanteric femoral fractures[J]. Injury, 2014,45(12):1932-1937.
doi: 10.1016/j.injury.2014.08.033 |
| [22] | 张培训, 薛峰, 安帅 , 等. 股骨近端防旋髓内钉和动力髋螺钉治疗股骨转子间骨折的显性和隐性失血量分析[J]. 北京大学学报(医学版), 2012,44(6):891-894. |
| [1] | 刘园梅, 傅义程, 郝靖欣, 张福春, 刘慧琳. 老年髋部骨折患者住院期间发生术后心力衰竭的列线图预测模型的构建及验证[J]. 北京大学学报(医学版), 2024, 56(5): 874-883. |
| [2] | 张浩宇,石逸雯,潘薇,刘爱萍,孙昕霙,李曼,张旭熙. 基于不同失能水平的老年人照料需求的影响因素[J]. 北京大学学报(医学版), 2024, 56(3): 431-440. |
| [3] | 靖婷,江华,李婷,申倩倩,叶兰,曾银丹,梁文欣,冯罡,司徒文佑,张玉梅. 中国西部5城市中老年人血清25羟基维生素D与握力的相关性[J]. 北京大学学报(医学版), 2024, 56(3): 448-455. |
| [4] | 林郁婷,王华丽,田宇,巩俐彤,常春. 北京市老年人认知功能的影响因素[J]. 北京大学学报(医学版), 2024, 56(3): 456-461. |
| [5] | 汤华萌,袁典琪,王明星,杨晗冰,郭超. 数字融入和健康生活方式对社会经济状况与老年人抑郁关系的序列中介作用[J]. 北京大学学报(医学版), 2024, 56(2): 230-238. |
| [6] | 刘慧丽,吕彦函,王晓晓,李民. 老年患者腹腔镜泌尿系肿瘤根治术后慢性疼痛的影响因素[J]. 北京大学学报(医学版), 2023, 55(5): 851-856. |
| [7] | 祝春素,连至炜,崔一民. 中国中老年人抑郁和慢性病的关联[J]. 北京大学学报(医学版), 2023, 55(4): 606-611. |
| [8] | 刘光奇,庞元捷,吴疆,吕敏,于孟轲,李雨橦,黄旸木. 2013—2019年流感季北京市住院老年人流感疫苗接种趋势分析[J]. 北京大学学报(医学版), 2022, 54(3): 505-510. |
| [9] | 刘杰,郭超. 正/负性情绪对中国老年人死亡风险影响的前瞻性队列研究[J]. 北京大学学报(医学版), 2022, 54(2): 255-260. |
| [10] | 李佳,徐钰,王优雅,高占成. 老年流感肺炎的临床特征及D-二聚体与疾病严重程度的相关性[J]. 北京大学学报(医学版), 2022, 54(1): 153-160. |
| [11] | 敖明昕,李学民,于媛媛,时会娟,黄红拾,敖英芳,王薇. 视觉重建对老年人行走动态足底压力的影响[J]. 北京大学学报(医学版), 2021, 53(5): 907-914. |
| [12] | 彭顺壮, 付茜茜, 冯星淋. 中国中老年居民教育程度与失能发生:社会参与的中介作用[J]. 北京大学学报(医学版), 2021, 53(3): 549-554. |
| [13] | 侯国进,周方,田耘,姬洪全,张志山,郭琰,吕扬,杨钟玮,张雅文. 后路短节段跨伤椎椎弓根螺钉固定治疗胸腰段爆裂骨折术后再发后凸的危险因素[J]. 北京大学学报(医学版), 2021, 53(1): 167-174. |
| [14] | 陈家丽,金月波,王一帆,张晓盈,李静,姚海红,何菁,李春. 老年发病类风湿关节炎的临床特征及其心血管疾病危险因素分析:一项大样本横断面临床研究[J]. 北京大学学报(医学版), 2020, 52(6): 1040-1047. |
| [15] | 刘中砥,许庭珉,党育,张殿英,付中国. 有限切开复位髓内外联合固定技术治疗股骨转子下骨折的临床随访[J]. 北京大学学报(医学版), 2020, 52(6): 1102-1106. |
|
||