北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (1): 152-157. doi: 10.19723/j.issn.1671-167X.2020.01.024
心肺适能对动脉粥样硬化性心血管疾病高危患者的保护作用
任川1,吴晓月1,赵威1,2,△( ),陶立元3,刘萍1,高炜1
),陶立元3,刘萍1,高炜1
- 1. 北京大学第三医院心内科,北京大学第三医院血管医学研究所,国家卫生健康委员会心血管分子生物学与调节肽重点实验室,分子心血管学教育部重点实验室,心血管受体研究北京市重点实验室,北京 100191
2. 北京大学第三医院体检中心,北京 100191
3. 北京大学第三医院临床流行病学研究中心,北京 100191
Protective effect of cardiopulmonary fitness on patients with high risk of atherosclerotic cardiovascular disease
Chuan REN1,Xiao-yue WU1,Wei ZHAO1,2,△( ),Li-yuan TAO3,Ping LIU1,Wei GAO1
),Li-yuan TAO3,Ping LIU1,Wei GAO1
- 1. Department of Cardiology, Peking University Third Hospital; Institute of Vascular Medicine of Peking University Third Hospital; Key Laboratory of Cardiovascular Molecular Biology and Regulatory Peptides of National Health Commission; Key Laboratory of Molecular Cardiovascular Science of Ministry of Education; Beijing Key Laboratory of Cardiovascular Receptors Research, Beijing 100191, China
2. Physical Examination Center, Peking University Third Hospital, Beijing 100191, China
3. Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing 100191, China
摘要:
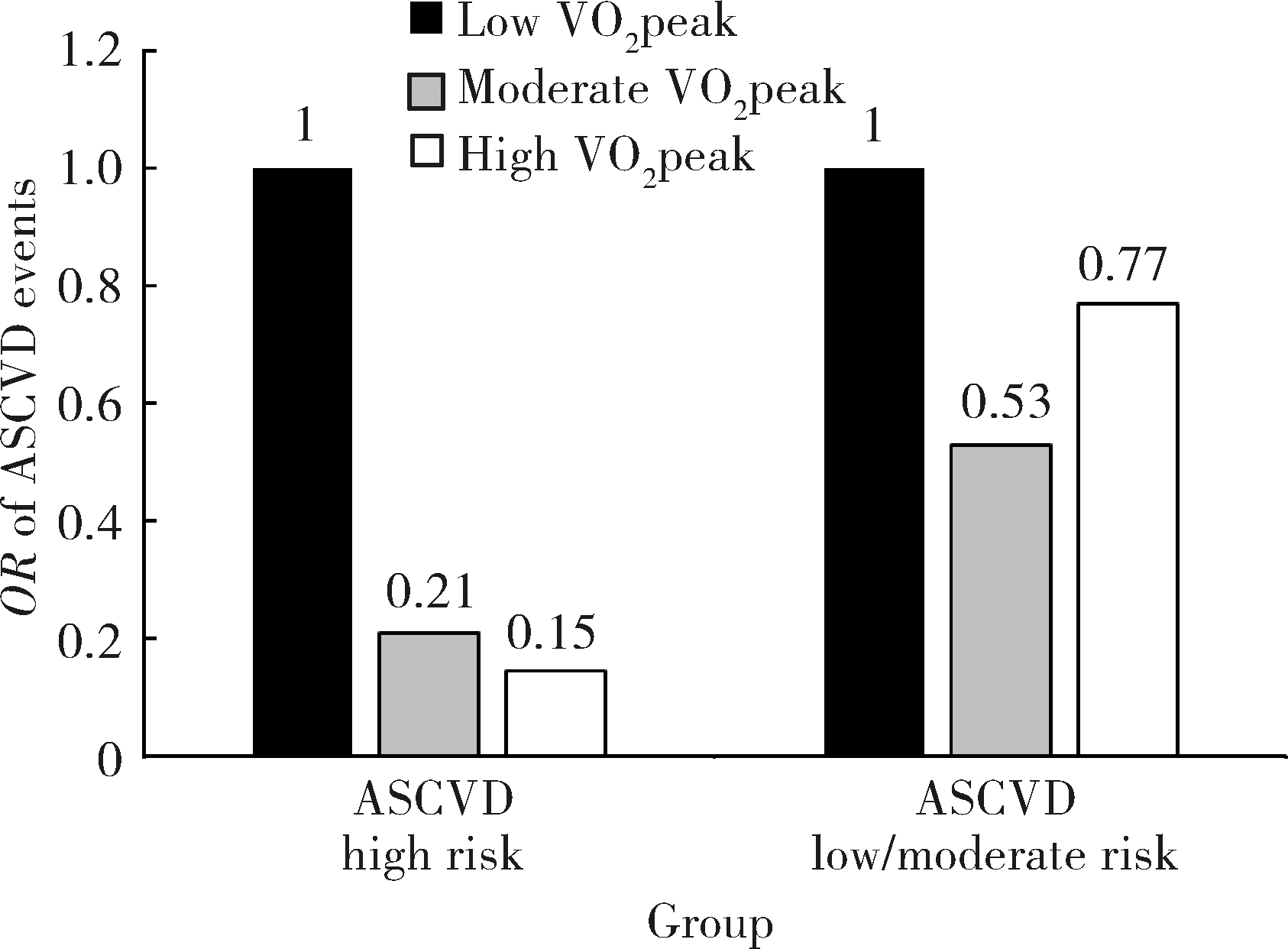
目的:在动脉粥样硬化性心血管疾病(arteriosclerotic cardiovascular disease,ASCVD)不同危险程度患者中评估心肺适能对ASCVD事件发生的影响。方法:入选2016年9月至2018年4月期间于北京大学第三医院行心肺运动试验的非ASCVD患者544例,根据《2016年中国成人血脂异常防治指南》对其进行ASCVD总体危险评估,通过心肺运动试验准确测定心肺适能指标——峰值摄氧量(peak oxygen uptake,VO2peak),并对患者进行临床随访。结果:506例患者完成了随访(低危组250例,中危组93例,高危组163例),中位随访时间为19个月(9~28个月)。在随访期内共51例患者出现ASCVD事件,其中心肌梗死/不稳定心绞痛/冠脉血运重建治疗者 33例,缺血性脑卒中/短暂脑缺血发作/颈动脉血运重建者18例。出现ASCVD事件的患者作为ASCVD组(n=51),其余患者作为非ASCVD组(n=455)。ASCVD组VO2peak[16.3(3.6)mL/(kg·min) vs. 19.1(3.2)mL/(kg·min), P<0.001]显著低于非ASCVD组。以是否发生ASCVD事件为因变量,进行Logistic回归分析,结果提示VO2peak[OR 0.893(95% CI:0.831~0.959),P=0.002]及ASCVD危险分层[OR 1.428(95% CI:1.028~1.878),P=0.031]与ASCVD事件的发生独立相关,VO2peak每升高1 mL/(kg·min),ASCVD事件发生风险降低11%。依据患者VO2peak的三分位数[14.4 mL/(kg·min), 23.0 mL/(kg·min)]将患者分为低、中、高VO2peak,分别在ASCVD 危险分层高危和中、低危的患者中,以是否发生ASCVD事件为因变量进行Logistic回归分析。结果显示在ASCVD危险分层高危患者中,中水平VO2peak[OR 0.210(95% CI:0.054~0.814),P=0.024]及高水平VO2peak[OR 0.146(95% CI:0.025~0.870), P=0.035]患者ASCVD事件的发生均显著下降,但在ASCVD中低危患者中未发现VO2peak升高对ASCVD事件发生的显著影响。结论:高心肺适能可显著降低ASCVD高危患者ASCVD事件的发生。
中图分类号:
- R541.4
| [1] | Ross R, Blair SN, Arena R , et al. Importance of assessing cardiorespiratory fitness in clinical practice: A case for fitness as a clinical vital sign: A scientific statement from the American Heart Association[J]. Circulation, 2016,134(24):e653-e699. |
| [2] | Hannan AL, Hing W, Simas V , et al. High-intensity interval training versus moderate-intensity continuous training within cardiac rehabilitation: A systematic review and meta-analysis[J]. Open Access J Sports Med, 2018,9:1-17. |
| [3] | Letnes JM, Dalen H, Vesterbekkmo EK , et al. Peak oxygen uptake and incident coronary heart disease in a healthy population: the HUNT fitness study[J]. Eur Heart J, 2019,40(20):1633-1639. |
| [4] | 中国成人血脂异常防治指南修订联合委员会. 中国成人血脂异常防治指南(2016年修订版)[J]. 中国循环杂志, 2016,31(10):937-951. |
| [5] | Skalski J, Allison TG, Miller TD , et al. The safety of cardiopulmonary exercise testing in a population with high-risk cardiovascular diseases[J]. Circulation, 2012,126(21):2465-2472. |
| [6] | Stamatakis E, Hamer M, O'Donovan G , et al. A non-exercise testing method for estimating cardiorespiratory fitness: Associations with all-cause and cardiovascular mortality in a pooled analysis of eight population-based cohorts[J]. Eur Heart J, 2013,34(10):750-758. |
| [7] | Gander J, Lee DC, Sui X , et al. Self-rated health status and cardiorespiratory fitness as predictors of mortality in men[J]. Br J Sports Med, 2011,45(14):1095-1100. |
| [8] | Kim D, Park W . The inverse relationship between cardiorespiratory fitness and intima- media thickness with prehypertensive middle-aged woman[J]. Tohoku J Exp Med, 2017,243(4):283-288. |
| [9] | Brawner CA, Al-Mallah MH, Ehrman JK , et al. Change in maximal exercise capacity is associated with survival in men and women[J]. Mayo Clin Proc, 2017,92(3):383-390. |
| [10] | Ehrman JK, Brawner CA, Al-Mallah MH , et al. Cardiorespiratory fitness change and mortality risk among black and white patients: Henry Ford Exercise Testing (FIT) project[J]. Am J Med, 2017,130(10):1177-1183. |
| [11] | Kelley E, Imboden MT, Harber MP , et al. Cardiorespiratory fitness is inversely associated with clustering of metabolic syndrome risk factors: The ball state adult fitness program longitudinal life-style study[J]. Mayo Clin Proc Innov Qual Outcomes, 2018,2(2):155-164. |
| [12] | Mora S, Redberg RF, Cui Y , et al. Ability of exercise testing to predict cardiovascular and all-cause death in asymptomatic women: A 20-year follow-up of the lipid research clinics prevalence study[J]. JAMA, 2003,290(12):1600-1607. |
| [13] | Barker AR, Gracia-Marco L, Ruiz JR , et al. Physical activity, sedentary time, TV viewing, physical fitness and cardiovascular disease risk in adolescents: The HELENA study[J]. Int J Car-diol, 2018,254:303-309. |
| [14] | Williams PT . Physical fitness and activity as separate heart disease risk factors: A meta-analysis[J]. Med Sci Sports Exerc, 2001,33(5):754-761. |
| [15] | Ekblom-Bak E, Hellénius ML, Ekblom O , et al. Independent associations of physical activity and cardiovascular fitness with cardiovascular risk in adults[J]. Eur J Cardiovasc Prev Rehabil, 2010,17(2):175-180. |
| [16] | Pinkstaff S, Peberdy MA, Kontos MC , et al. Overestimation of aerobic capacity with the bruce treadmill protocol in patients being assessed for suspected myocardial ischemia[J]. J Cardiopulm Rehabil Prev, 2011,31(4):254-260. |
| [1] | 刘欢,何映东,刘金波,黄薇,赵娜,赵红薇,周晓华,王宏宇. 血管健康指标对新发心脑血管事件的预测价值:北京血管健康分级标准的初步验证[J]. 北京大学学报(医学版), 2020, 52(3): 514-520. |
| [2] | 孙文强,赵舟,高卿,韩增强,杨威,廉波,刘刚,陈生龙,陈彧. 非体外循环冠状动脉旁路移植术中桥血管血流对术后近中期预后的影响[J]. 北京大学学报(医学版), 2019, 51(5): 851-855. |
| [3] | 张静,李素芳,陈红,宋俊贤. miR-106b-5p在调节内皮细胞基因表达谱中的作用[J]. 北京大学学报(医学版), 2019, 51(2): 221-227. |
| [4] | 刘滕飞,张婧薇,陈夏欢,冯雪茹,柏中胜,刘梅林. CMTM5基因rs723840单核苷酸多态性与阿司匹林治疗下血小板高反应性的相关性研究[J]. 北京大学学报(医学版), 2015, 47(6): 905-909. |
| [5] | 刘滕飞,张婧薇,陈夏欢,冯雪茹,柏中胜,刘梅林. 尿11-脱氢血栓素B2水平与2型糖尿病合并冠心病患者阿司匹林临床疗效的相关性研究[J]. 北京大学学报(医学版), 2015, 47(6): 920-924. |
|
||