北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (1): 188-194. doi: 10.19723/j.issn.1671-167X.2021.01.028
肺叶切除术中少尿与术后急性肾损伤的关系
- 北京大学第一医院麻醉科,北京 100034
Impact of oliguria during lung surgery on postoperative acute kidney injury
MENG Zhao-ting,MU Dong-liang( )
)
- Department of Anesthesiology, Peking University First Hospital, Beijing 100034, China
摘要:
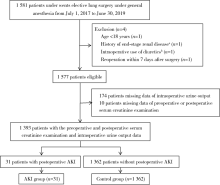
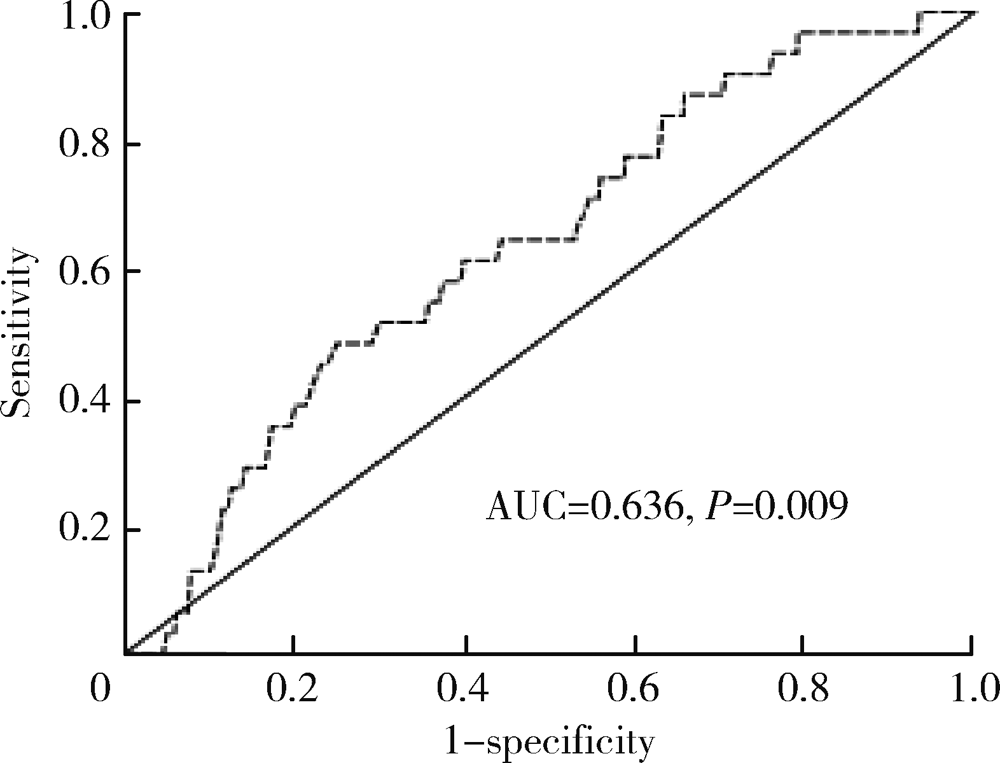
目的: 探索术中尿量对术后急性肾损伤(acute kidney injury, AKI)的影响,以及术后AKI发生的独立危险因素。方法: 选择2017年7月至2019年6月于北京大学第一医院在全身麻醉下接受择期肺叶切除术的患者作为研究对象进行回顾性队列研究。将入组患者按照是否发生术后AKI分为AKI组和对照组。首先对围术期各变量进行单因素分析,探讨其与术后AKI的关系;其次,采用受试者工作特征曲线(receiver operating characteristic curve,ROC curve)分析术中尿量对术后AKI的预测价值,并以约登(Youden)指数为最大值时的上下4个界值[以0.1 mL/(kg·h)为间隔]为少尿界值,采用单因素分析探索各界值定义下的少尿与AKI发生风险的关系,并取OR值最大者为少尿界值;最后,将单因素分析中P<0.10的围术期各变量共同代入多因素Logistic回归模型,分析术后AKI的独立危险因素。结果: 共1 393名患者最终纳入研究,术后AKI发生率为2.2%。ROC曲线显示术中单位尿量用于预测术后AKI的曲线下面积为0.636(P=0.009), 约登指数为最大值时(约登指数0.234,敏感度48.4%,特异度75.0%)的少尿界值为0.785 mL/(kg·h)。进一步取0.7、0.8、0.9、1.0 mL/(kg·h)以及传统界值0.5 mL/(kg·h)为少尿界值分析少尿对术后AKI的影响。单因素分析显示,以小于0.8 mL/(kg·h)为少尿界值时,少尿患者发生AKI的风险增加最为显著(OR=2.774, 95%CI 1.357~5.671, P=0.004)。多因素回归分析显示术中尿量<0.8 mL/(kg·h)(OR=2.698,95%CI 1.260~5.778, P=0.011)是术后AKI发生的独立危险因素,另两个独立危险因素为术前血红蛋白≤120.0 g/L(OR=3.605, 95%CI 1.545~8.412, P=0.003)以及术前估计肾小球滤过率<30 mL/(min·1.73 m2)(OR=11.009, 95%CI 1.813~66.843, P=0.009)。 结论: 对于肺叶切除术,术中少尿是术后AKI发生的独立危险因素,且尿量<0.8 mL/(kg·h)是可能的筛选标准。
中图分类号:
- R614
| [1] | Nadim MK, Forni LG, Bihorac A, et al. Cardiac and vascular surgery-associated acute kidney injury: the 20th International Consensus Conference of the ADQI (acute disease quality initiative) group[J]. J Am Heart Assoc, 2018,7(11):e8834. |
| [2] |
Sanaiha Y, Kavianpour B, Dobaria V, et al. Acute kidney injury is independently associated with mortality and resource use after emergency general surgery operations[J]. Surgery, 2020,167(2):328-334.
doi: 10.1016/j.surg.2019.07.035 pmid: 31668777 |
| [3] |
Vaara ST, Bellomo R. Postoperative renal dysfunction after noncardiac surgery[J]. Curr Opin Crit Care, 2017,23(5):440-446.
doi: 10.1097/MCC.0000000000000439 pmid: 28820797 |
| [4] |
Grams ME, Sang Y, Coresh J, et al. Acute kidney injury after major surgery: a retrospective analysis of veterans health administration data[J]. Am J Kidney Dis, 2016,67(6):872-880.
doi: 10.1053/j.ajkd.2015.07.022 pmid: 26337133 |
| [5] | Cardinale D, Cosentino N, Moltrasio M, et al. Acute kidney injury after lung cancer surgery: Incidence and clinical relevance, predictors, and role of N-terminal pro B-type natriuretic peptide[J]. Lung Cancer, 2018,123(9):155-159. |
| [6] |
Ostermann M, Joannidis M. Acute kidney injury 2016: diagnosis and diagnostic workup[J]. Crit Care, 2016,20(1):299-311.
doi: 10.1186/s13054-016-1478-z pmid: 27670788 |
| [7] |
Weiss R, Meersch M, Pavenstädt HJ, et al. Acute kidney injury: a frequently underestimated problem in perioperative medicine[J]. Dtsch Arztebl Int, 2019,116(49):833-842.
doi: 10.3238/arztebl.2019.0833 pmid: 31888797 |
| [8] |
Zarbock A, Koyner JL, Hoste EAJ, et al. Update on perioperative acute kidney injury[J]. Anesth Analg, 2018,127(5):1236-1245.
doi: 10.1213/ANE.0000000000003741 pmid: 30138176 |
| [9] |
du Toit L, Biccard BM. The relationship between intraoperative oliguria and acute kidney injury[J]. Br J Anaesth, 2019,122(6):707-710.
doi: 10.1016/j.bja.2019.03.008 pmid: 30961912 |
| [10] |
Hori D, Katz1 NM, Fine DM, et al. Defining oliguria during cardiopulmonary bypass and its relationship with cardiac surgery-associated acute kidney injury[J]. Br J Anaesth, 2016,117(6):733-740.
pmid: 27956671 |
| [11] |
Mizota T, Yamamoto Y, Hamada M, et al. Intraoperative oliguria predicts acute kidney injury after major abdominal surgery[J]. Br J Anaesth, 2017,119(6):1127-1134.
doi: 10.1093/bja/aex255 pmid: 29136086 |
| [12] |
Kim HJ, Cha SI, Kim CH, et al. Risk factors of postoperative acute lung injury following lobectomy for nonsmall cell lung cancer[J]. Medicine, 2019,98(13):e15078.
doi: 10.1097/MD.0000000000015078 pmid: 30921242 |
| [13] |
O’Connor ME, Kirwan CJ, Pearse RM, et al. Incidence and associations of acute kidney injury after major abdominal surgery[J]. Intensive Care Med, 2016,42(4):521-530.
doi: 10.1007/s00134-015-4157-7 pmid: 26602784 |
| [14] |
Levey AS, Coresh J, Greene T, et al. Expressing the modification of diet in renal disease study equation for estimating glomerular filtration rate with standardized serum creatinine values[J]. Clin Chem, 2007,53(4):766-772.
doi: 10.1373/clinchem.2006.077180 pmid: 17332152 |
| [15] |
Quan S, Pannu N, Wilson T, et al. Prognostic implications of adding urine output to serum creatinine measurements for staging of acute kidney injury after majorsurgery: a cohort study[J]. Nephrol Dial Transplant, 2016,31(12):2049-2056.
doi: 10.1093/ndt/gfw374 pmid: 27941063 |
| [16] |
Kellum JA, Sileanu FE, Murugan R, et al. Classifying AKI by urine output versus serum creatinine level[J]. J Am Soc Nephrol, 2015,26(9):2231-2238.
doi: 10.1681/ASN.2014070724 pmid: 25568178 |
| [17] |
Eknoyan G. Rufus of ephesus and his “diseases of the kidneys”[J]. Nephron, 2002,91(3):383-390.
doi: 10.1159/000064277 pmid: 12119467 |
| [18] |
Macedo E, Malhotra R, Bouchard J, et al. Oliguria is an early predictor of higher mortality in critically ill patients[J]. Kidney Int, 2011,80(7):760-770.
doi: 10.1038/ki.2011.150 pmid: 21716258 |
| [19] | Inácio R, Gameiro J, Amaro S, et al. Intraoperative oliguria does not predict postoperative acute kidney injury in major abdominal surgery: a cohort analysis [J/OL]. J Bras Nefrol[2019-12-01]. https://doi.org/10.1590/2175-8239-jbn-2019-0244. |
| [20] |
Rung GW, Marshall WK. Nerve blocks in the critical care environment[J]. Crit Care Clin, 1990,6(2):343-367.
pmid: 2188709 |
| [21] |
Matot I, Dery E, Bulgov Y, et al. Fluid management during video-assisted thoracoscopic surgery for lung resection: a ran-domized, controlled trial of effects on urinary output and postoperative renal function[J]. J Thorac Cardiovasc Surg, 2013,146(2):461-466.
doi: 10.1016/j.jtcvs.2013.02.015 pmid: 23558303 |
| [22] |
Myles PS, Bellomo R, Corcoran T, et al. Restrictive versus liberal fluid therapy for major abdominal surgery[J]. N Engl J Med, 2018,378(24):2263-2274.
doi: 10.1056/NEJMoa1801601 pmid: 29742967 |
| [1] | 李志存, 吴天俣, 梁磊, 范宇, 孟一森, 张骞. 穿刺活检单针阳性前列腺癌术后病理升级的危险因素分析及列线图模型构建[J]. 北京大学学报(医学版), 2024, 56(5): 896-901. |
| [2] | 颜野,李小龙,夏海缀,朱学华,张羽婷,张帆,刘可,刘承,马潞林. 前列腺癌根治术后远期膀胱过度活动症的危险因素[J]. 北京大学学报(医学版), 2024, 56(4): 589-593. |
| [3] | 陈延,李况蒙,洪锴,张树栋,程建星,郑仲杰,唐文豪,赵连明,张海涛,姜辉,林浩成. 阴茎海绵体注射试验对阴茎血管功能影响的回顾性研究[J]. 北京大学学报(医学版), 2024, 56(4): 680-686. |
| [4] | 庞博,郭桐君,陈曦,郭华棋,石嘉章,陈娟,王欣梅,李耀妍,单安琪,余恒意,黄婧,汤乃军,王艳,郭新彪,李国星,吴少伟. 天津与上海35岁以上人群氮氧化物个体暴露水平及其影响因素[J]. 北京大学学报(医学版), 2024, 56(4): 700-707. |
| [5] | 和静,房中则,杨颖,刘静,马文瑶,霍勇,高炜,武阳丰,谢高强. 血浆中脂质代谢分子与颈动脉粥样硬化斑块、传统心血管危险因素及膳食因素的关系[J]. 北京大学学报(医学版), 2024, 56(4): 722-728. |
| [6] | 蔡珊,张依航,陈子玥,刘云飞,党佳佳,师嫡,李佳欣,黄天彧,马军,宋逸. 北京市中小学生身体活动时间现状及影响因素的路径[J]. 北京大学学报(医学版), 2024, 56(3): 403-410. |
| [7] | 张祖洪,陈天娇,马军. 中小学生青春发动时相与心血管代谢危险因素的相关性[J]. 北京大学学报(医学版), 2024, 56(3): 418-423. |
| [8] | 林郁婷,王华丽,田宇,巩俐彤,常春. 北京市老年人认知功能的影响因素[J]. 北京大学学报(医学版), 2024, 56(3): 456-461. |
| [9] | 朱金荣,赵亚娜,黄巍,赵微微,王悦,王松,苏春燕. 感染新型冠状病毒的血液透析患者的临床特征[J]. 北京大学学报(医学版), 2024, 56(2): 267-272. |
| [10] | 赖展鸿,李嘉辰,贠泽霖,张永刚,张昊,邢晓燕,邵苗,金月波,王乃迪,李依敏,李玉慧,栗占国. 特发性炎性肌病完全临床应答相关因素的单中心真实世界研究[J]. 北京大学学报(医学版), 2024, 56(2): 284-292. |
| [11] | 司筱芊,赵秀娟,朱凤雪,王天兵. 创伤出血性休克后急性呼吸窘迫综合征的危险因素[J]. 北京大学学报(医学版), 2024, 56(2): 307-312. |
| [12] | 李洋洋,侯林,马紫君,黄山雅美,刘捷,曾超美,秦炯. 孕期因素与婴儿牛奶蛋白过敏的关系[J]. 北京大学学报(医学版), 2024, 56(1): 144-149. |
| [13] | 刘晓强,周寅. 牙种植同期植骨术围术期高血压的相关危险因素[J]. 北京大学学报(医学版), 2024, 56(1): 93-98. |
| [14] | 罗靓,李云,王红彦,相晓红,赵静,孙峰,张晓盈,贾汝琳,李春. 抗内皮细胞抗体检测在早期流产中的预测价值[J]. 北京大学学报(医学版), 2023, 55(6): 1039-1044. |
| [15] | 游芳凝,罗靓,刘香君,张学武,李春. 未分化结缔组织病患者的妊娠结局、疾病演变及其影响因素[J]. 北京大学学报(医学版), 2023, 55(6): 1045-1052. |
|
||