北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (4): 680-685. doi: 10.19723/j.issn.1671-167X.2021.04.010
单侧肾细胞癌根治性切除术后的肾功能代偿
韩松辰,黄子雄,刘慧鑫,徐涛
- 北京大学人民医院泌尿外科,北京 100044
Renal functional compensation after unilateral radical nephrectomy of renal cell carcinoma
HAN Song-chen,HUANG Zi-xiong,LIU Hui-xin,XU Tao
- Department of Urology, Peking University People’s Hospital, Beijing 100044, China
摘要:
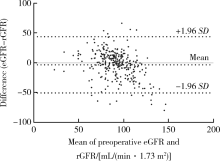
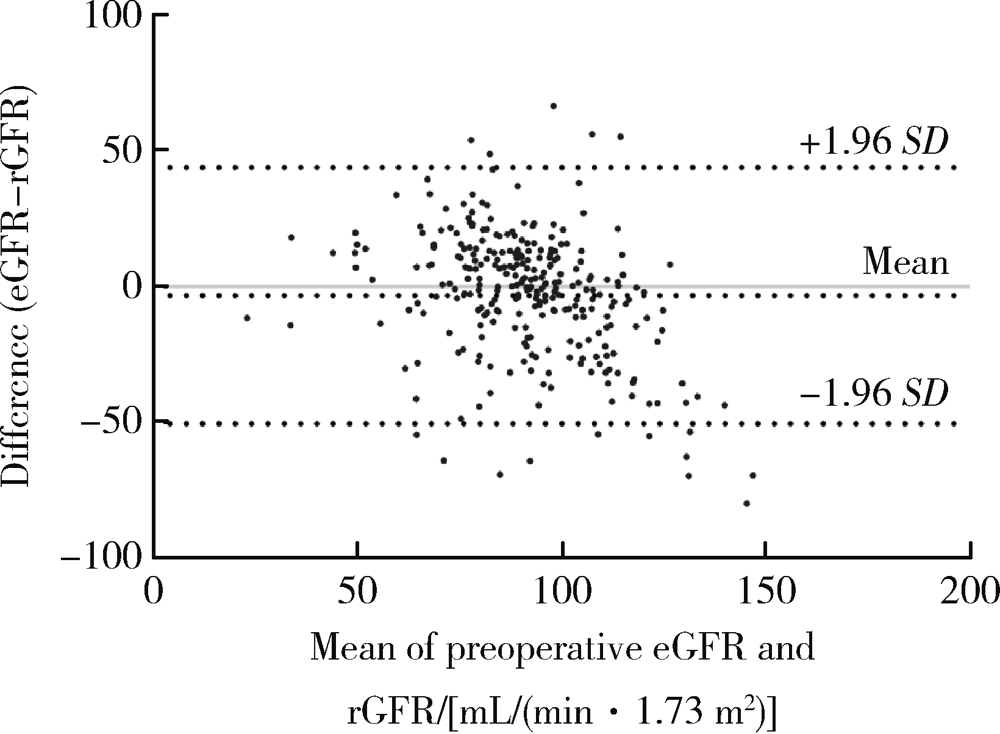
目的: 探讨单侧肾细胞癌根治性肾切除术(radical nephrectomy,RN)后留存肾肾功能代偿(renal functional compensation,RFC)的影响因素。方法: 回顾性分析286例在北京大学人民医院接受RN的肾细胞癌患者的临床资料,记录术前体重指数(body mass index,BMI)、收缩压、吸烟史、慢性疾病史等基础信息和术前血生化、尿常规、影像学等辅助检查结果。所有患者均在术前行99m锝-二乙三胺五乙酸(99mtechnetium-diethylenetriamine pentaacetic acid,99mTc-DTPA)肾动态显像检查。记录手术方式、术后病理结果和术后1~60个月的血肌酐数值。术前、术后估计肾小球滤过率(estimate the glomerular filtration rate,eGFR)由慢性肾脏疾病流行病学合作组(chronic kidney disease epidemiology collaboration,CKD-EPI)公式计算,RFC百分比定义为RN术后留存肾eGFR较术前eGFR变化的百分比。采用单因素和多因素线性回归分析确定影响留存肾RFC的独立预测因素。结果: 患者中位年龄61岁,65.4%为男性,83.6%的病例为早期肾细胞癌(T1期和T2期)。18.5%的患者术前合并糖尿病,39.5%合并高血压,19.2%既往有吸烟史,27.6%在术前影像学检查中发现健侧肾囊肿。226例患者行腹腔镜RN,60例行开腹RN。肾透明细胞癌是最主要的病理类型,占88.5%,中位肿瘤最大径为4.5 cm(0.7~13.5 cm)。术后1个月时中位RFC百分比为27%,在随后5年内保持稳定。单因素变量分析结果显示年龄、性别、术前血尿酸水平、术前是否存在蛋白尿、是否存在健侧肾囊肿以及术前健侧肾的分肾功能百分比与RN术后留存肾RFC百分比具有相关性(P<0.05),其中,术前血尿酸水平和术前健侧肾分肾功能百分比与术后RFC百分比呈极强负相关性。多因素线性回归分析结果显示,年龄(P<0.001)、术前血尿酸水平(P<0.001)、术前是否存在蛋白尿(P=0.002)、术前eGFR(P<0.001)和术前健侧肾分肾功能百分比(P<0.001)是术后RFC的独立预测因素。结论: 术前血生化、尿常规和肾动态显像等基本辅助检查对于预测RN术后留存肾的代偿能力意义很大,临床决策时需综合考虑多方面因素对术后基线eGFR的影响。
中图分类号:
- R737.11
| [1] |
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020 [J]. CA Cancer J Clin, 2020, 70(1):7-30.
doi: 10.3322/caac.v70.1 |
| [2] |
Campbell S, Uzzo RG, Allaf ME, et al. Renal mass and localized renal cancer: AUA guideline [J]. J Urol, 2017, 198(3):520-529.
doi: S0022-5347(17)59870-5 pmid: 28479239 |
| [3] | Patel N, Mason P, Rushton S, et al. Renal function and cardiovascular outcomes after living donor nephrectomy in the UK: Qua-lity and safety revisited [J]. BJU Int, 2013, 112(2):134-142. |
| [4] |
Lee SH, Kim DS, Cho S, et al. Comparison of postoperative estimated glomerular filtration rate between kidney donors and radical nephrectomy patients, and risk factors for postoperative chronic kidney disease [J]. Int J Urol, 2015, 22(7):674-678.
doi: 10.1111/iju.2015.22.issue-7 |
| [5] |
Srivastava T, Hariharan S, Alon US, et al. Hyperfiltration-mediated injury in the remaining kidney of a transplant donor [J]. Transplantation, 2018, 102(10):1624-1635.
doi: 10.1097/TP.0000000000002304 pmid: 29847501 |
| [6] |
Aguilar Palacios D, Caraballo ER, Tanaka H, et al. Compensatory changes in parenchymal mass and function after radical nephrectomy [J]. J Urol, 2020, 204(1):42-49.
doi: 10.1097/JU.0000000000000797 pmid: 32073996 |
| [7] |
Zabor EC, Furberg H, Lee B, et al. Long-term renal function recovery following radical nephrectomy for kidney cancer: Results from a multicenter confirmatory study [J]. J Urol, 2018, 199(4):921-926.
doi: 10.1016/j.juro.2017.10.027 |
| [8] |
Kawamura N, Yokoyama M, Fujii Y, et al. Recovery of renal function after radical nephrectomy and risk factors for postoperative severe renal impairment: A Japanese multicenter longitudinal study [J]. Int J Urol, 2016, 23(3):219-223.
doi: 10.1111/iju.13028 pmid: 26663437 |
| [9] |
Park BH, Sung HH, Jeong BC, et al. Tumor size is associated with compensatory hypertrophy in the contralateral kidney after radical nephrectomy in patients with renal cell carcinoma [J]. Int Urol Nephrol, 2016, 48(6):977-983.
doi: 10.1007/s11255-016-1250-y |
| [10] |
Anderson RG, Bueschen AJ, Lloyd LK, et al. Short-term and long-term changes in renal function after donor nephrectomy [J]. J Urol, 1991, 145(1):11-13.
doi: 10.1016/S0022-5347(17)38232-0 |
| [11] |
Okada T, Omoto-Kitao M, Mukamoto M, et al. Compensatory renal growth in uninephrectomized immature rats: Proliferative acti-vity and epidermal growth factor [J]. J Vet Med Sci, 2010, 72(8):975-980.
doi: 10.1292/jvms.09-0496 |
| [12] |
Shehab AB, Shaheen FA, Fallatah A, et al. Early changes in vo-lume and function of the remaining kidney after unilateral donor nephrectomy [J]. Saudi J Kidney Dis Transpl, 1994, 5(4):474-478.
pmid: 18583774 |
| [13] |
Vergho D, Burger M, Schrammel M, et al. Matched-pair analysis of renal function in the immediate postoperative period: A comparison of living kidney donors versus patients nephrectomized for renal cell cancer [J]. World J Urol, 2015, 33(5):725-731.
doi: 10.1007/s00345-014-1423-1 |
| [14] |
Scosyrev E, Messing EM, Sylvester R, et al. Renal function after nephron-sparing surgery versus radical nephrectomy: Results from EORTC randomized trial 30904 [J]. Eur Urol, 2014, 65(2):372-377.
doi: 10.1016/j.eururo.2013.06.044 pmid: 23850254 |
| [15] | Sarkar D, Agrawal A, Agrawal DK. Clinical assessment of stabilisation of renal function after nephrectomy [J/OL]. Urologia, 2021. . |
| [16] |
Takagi T, Mir MC, Sharma N, et al. Compensatory hypertrophy after partial and radical nephrectomy in adults [J]. J Urol, 2014, 192(6):1612-1618.
doi: 10.1016/j.juro.2014.06.018 |
| [17] |
Jeon HG, Choo SH, Jeong BC, et al. Uric acid levels correlate with baseline renal function and high levels are a potent risk factor for postoperative chronic kidney disease in patients with renal cell carcinoma [J]. J Urol, 2013, 189(4):1249-1254.
doi: 10.1016/j.juro.2012.11.043 |
| [18] |
Cho A, Lee JE, Jang HR, et al. Association between pre-donation serum uric acid concentration and change in renal function after living kidney donation in women [J]. Intern Med J, 2014, 44(12a):1217-1222.
doi: 10.1111/imj.12591 pmid: 25266773 |
| [19] |
Yim K, Bindayi A, Mckay R, et al. Rising serum uric acid level is negatively associated with survival in renal cell carcinoma [J]. Cancers (Basel), 2019, 11(4):536.
doi: 10.3390/cancers11040536 |
| [20] |
Khosla UM, Zharikov S, Finch JL, et al. Hyperuricemia induces endothelial dysfunction [J]. Kidney Int, 2005, 67(5):1739-1742.
pmid: 15840020 |
| [21] | Guo B, Guo Y, Liu C. Predictive factors of progression in renal function after unilateral nephrectomy in renal malignancy [J]. J buon, 2020, 25(3):1650-1657. |
| [22] | Zhang Z, Zhao J, Zabell J, et al. Proteinuria in patients undergoing renal cancer surgery: Impact on overall survival and stability of renal function [J]. Eur Urol Focus, 2016, 2(6):616-622. |
| [23] | 杜晓英, 李林法, 何强, 等. 99mTc-DTPA肾动态显像检测肾小球滤过率的临床应用评价 [J]. 中华肾脏病杂志, 2006, 22(5):266-270. |
| [1] | 周泽臻,邓绍晖,颜野,张帆,郝一昌,葛力源,张洪宪,王国良,张树栋. 非转移性T3a肾细胞癌患者3年肿瘤特异性生存期预测[J]. 北京大学学报(医学版), 2024, 56(4): 673-679. |
| [2] | 沈棋,刘亿骁,何群. 肾黏液样小管状和梭形细胞癌的临床病理特点及预后[J]. 北京大学学报(医学版), 2023, 55(2): 276-282. |
| [3] | 许云屹,苏征征,郑林茂,张孟尼,谭珺娅,杨亚蓝,张梦鑫,徐苗,陈铌,陈雪芹,周桥. 转录通读环状RNA rt-circ-HS促进低氧诱导因子1α表达和肾癌细胞增殖与侵袭[J]. 北京大学学报(医学版), 2023, 55(2): 217-227. |
| [4] | 张铨,宋海峰,马冰磊,张喆楠,周朝晖,李傲林,刘军,梁磊,朱时雨,张骞. 术前预后营养指数可作为预测非转移性肾细胞癌预后的指标[J]. 北京大学学报(医学版), 2023, 55(1): 149-155. |
| [5] | 博尔术,洪鹏,张宇,邓绍晖,葛力源,陆敏,李楠,马潞林,张树栋. 乳头状肾细胞癌的临床病理特征和预后分析[J]. 北京大学学报(医学版), 2022, 54(4): 615-620. |
| [6] | 周鑫,李文智. 肾细胞癌极致保肾时代的冷思考[J]. 北京大学学报(医学版), 2022, 54(4): 595-598. |
| [7] | 田雨,程晓悦,贺慧颖,王国良,马潞林. 肾细胞癌合并尿路瘤栓的临床病理特征: 6例报道及文献回顾[J]. 北京大学学报(医学版), 2021, 53(5): 928-932. |
| [8] | 赵勋,颜野,黄晓娟,董靖晗,刘茁,张洪宪,刘承,马潞林. 癌栓粘连血管壁对非转移性肾细胞癌合并下腔静脉癌栓患者手术及预后的影响[J]. 北京大学学报(医学版), 2021, 53(4): 665-670. |
| [9] | 孙争辉,黄晓娟,董靖晗,刘茁,颜野,刘承,马潞林. 临床T1期肾细胞癌肾窦侵犯的危险因素[J]. 北京大学学报(医学版), 2021, 53(4): 659-664. |
| [10] | 于妍斐,何世明,吴宇财,熊盛炜,沈棋,李妍妍,杨风,何群,李学松. 延胡索酸水合酶缺陷型肾细胞癌的临床病理特征及预后[J]. 北京大学学报(医学版), 2021, 53(4): 640-646. |
| [11] | 张晓鹏,黄子雄,于路平,张晓威,李清,刘士军,徐涛. 小肾细胞癌的临床与病理特征分析[J]. 北京大学学报(医学版), 2019, 51(4): 623-627. |
| [12] | 黄子雄,杜依青,张晓鹏,刘士军,徐涛. 肾细胞癌骨转移的临床与病理分析[J]. 北京大学学报(医学版), 2018, 50(5): 811-815. |
| [13] | 丁振山,邱敏,徐梓程,肖若陶,葛力源,马潞林. 乳头状肾细胞癌合并癌栓患者的临床病理分析[J]. 北京大学学报(医学版), 2018, 50(5): 805-810. |
| [14] | 孙静,宋卫东,闫思源,席志军. 氯喹抑制肾癌细胞活性促进舒尼替尼诱导的细胞凋亡[J]. 北京大学学报(医学版), 2018, 50(5): 778-784. |
|
||