北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (4): 686-691. doi: 10.19723/j.issn.1671-167X.2022.04.017
原发性醛固酮增多症术后高血压未治愈的危险因素
- 北京大学人民医院泌尿外科,北京 100044
Risk factors of persistent hypertension in primary aldosteronism patients after surgery
Yu-chao HUANG-FU,Yi-qing DU,Lu-ping YU,Tao XU*( )
)
- Department of Urology, Peking University People' s Hospital, Beijing 100044, China
摘要:
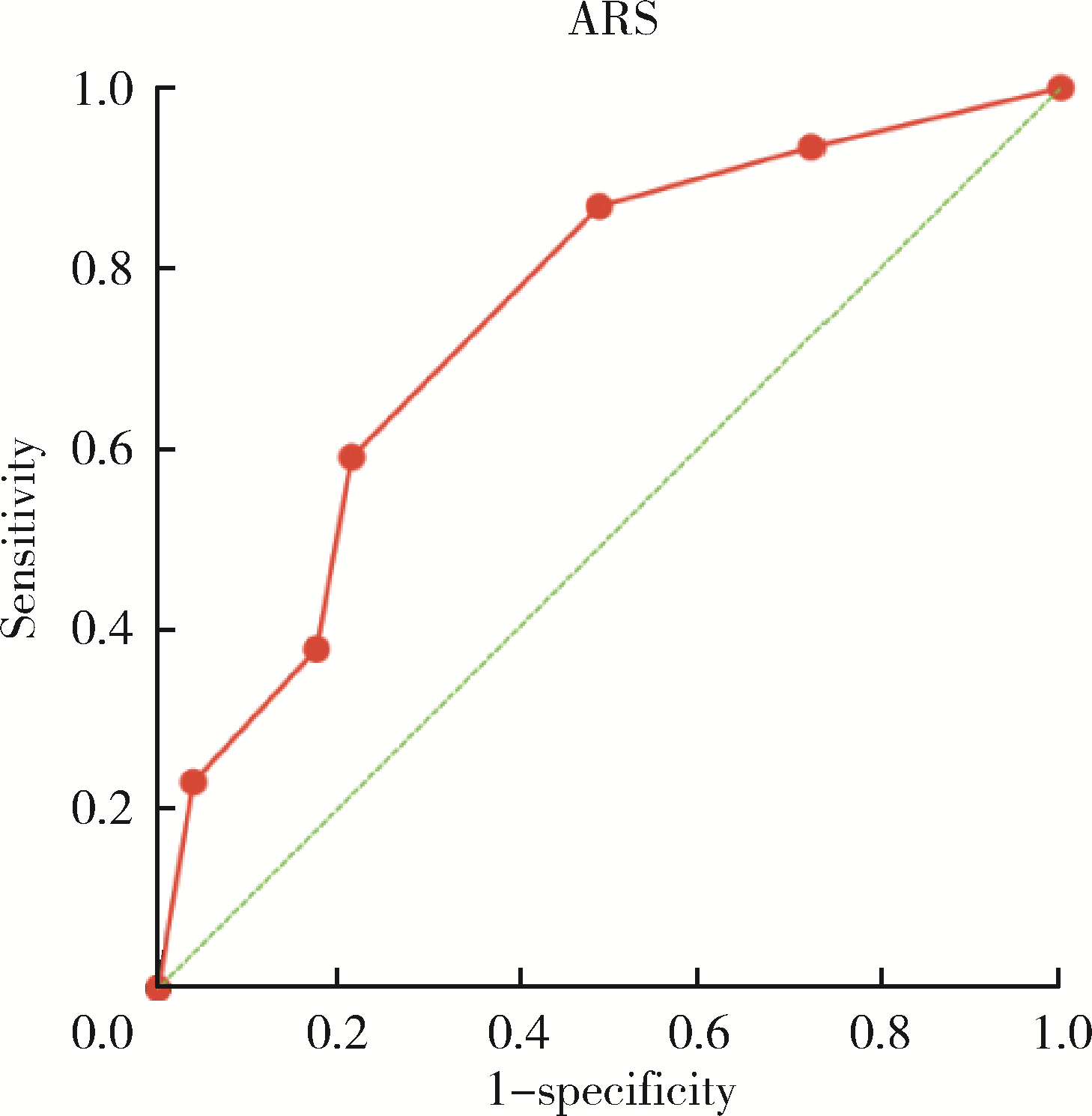
目的: 分析原发性醛固酮增多症患者术后高血压未治愈的危险因素,评价ARS(aldosteronoma resolution score)对于原发性醛固酮增多症术后高血压状态的预测价值。方法: 选择2018年1月—2021年6月于北京大学人民医院行手术治疗的原发性醛固酮增多症患者的病例资料进行回顾性分析,根据术后高血压疾病状态,将患者分为高血压治愈组和高血压未治愈组,比较不同预后组间术前相关因素差异,分析原发性醛固酮增多症患者手术后高血压不缓解的危险因素,并评估ARS对于预测原发性醛固酮增多症术后高血压治愈的价值。结果: 共纳入112例患者,至少6个月术后随访后,大多数患者(94.6%)都达到术后高血压完全缓解或部分缓解。根据患者术后高血压状态,将患者分为高血压治愈组(51例)和高血压未治愈组(61例)。两组间患者年龄、体重指数、腰围、高血压病程、术前降压药物种类、术前收缩压、糖尿病病史、心脑血管疾病病史、血清肌酐、估算肾小球滤过率(estimated glomerular filtration rate,eGFR)、高密度脂蛋白胆固醇和甘油三酯差异有统计学意义。Logistic回归分析发现年龄(OR=1.111,95%CI:1.029~1.199)、腰围(OR=1.073,95%CI:1.013~1.137)、术前收缩压(OR=1.033,95%CI:1.008~1.060)和心脑血管疾病病史(OR=16.061,95%CI:1.312~196.612)是原发性醛固酮增多症患者术后高血压未治愈的危险因素,但性别并不是高血压未治愈的危险因素。高血压治愈组患者中位ARS为4分,而未治愈组为2分,在ARS4~5分患者中,术后高血压治愈率为76.5%,ARS的ROC曲线下面积(AUC)为0.743。结论: 心脑血管疾病病史是术后高血压不治愈的重要危险因素,ARS对于预测原发性醛固酮增多症术后高血压状态有一定价值,但仍需进一步研究设计出更适合中国人群的原发性醛固酮增多症手术结果的预测模型。
中图分类号:
- R699
| 1 |
Funder JW , Carey RM , Mantero F , et al. The management of primary aldosteronism: Case detection, diagnosis, and treatment: An endocrine society clinical practice guideline[J]. J Clin Endocrinol Metab, 2016, 101 (5): 1889- 1916.
doi: 10.1210/jc.2015-4061 |
| 2 |
Buffolo F , Burrello J , Burrello A , et al. Clinical score and machine learning-based model to predict diagnosis of primary aldosteronism in arterial hypertension[J]. Hypertension, 2021, 78 (5): 1595- 1604.
doi: 10.1161/HYPERTENSIONAHA.121.17444 |
| 3 |
Xu F , Gao Z , Wang G , et al. Prevalence, subtype classification, and outcomes of treatment of primary aldosteronism: A prospective study in china[J]. Endocr Pract, 2021, 27 (5): 478- 483.
doi: 10.1016/j.eprac.2020.10.007 |
| 4 |
Rossi GP , Bernini G , Caliumi C , et al. A prospective study of the prevalence of primary aldosteronism in 1, 125 hypertensive patients[J]. J Am Coll Cardiol, 2006, 48 (11): 2293- 2300.
doi: 10.1016/j.jacc.2006.07.059 |
| 5 |
Douma S , Petidis K , Doumas M , et al. Prevalence of primary hyperaldosteronism in resistant hypertension: A retrospective observational study[J]. Lancet, 2008, 371 (9628): 1921- 1926.
doi: 10.1016/S0140-6736(08)60834-X |
| 6 |
Calhoun DA , Nishizaka MK , Zaman MA , et al. Hyperaldosteronism among black and white subjects with resistant hypertension[J]. Hypertension, 2002, 40 (6): 892- 896.
doi: 10.1161/01.HYP.0000040261.30455.B6 |
| 7 |
Gomez-Sanchez CE , Gomez-Sanchez EP . Aldosterone-producing adenomas: Mining for genes[J]. Hypertension, 2010, 55 (6): 1306- 1307.
doi: 10.1161/HYPERTENSIONAHA.110.151480 |
| 8 | Rossi GP, Bisogni V, Bacca AV, et al. The 2020 italian society of arterial hypertension (SIIA) practical guidelines for the management of primary aldosteronism [J/OL]. Int J Cardiol Hypertens, 2020, 5: 100029[2022-03-15]. https://doi.org/10.1016/j.ijchy.2020.100029. |
| 9 |
Nishikawa T , Omura M , Satoh F , et al. Guidelines for the diagnosis and treatment of primary aldosteronism: The Japan endocrine society 2009[J]. Endocr J, 2011, 58 (9): 711- 721.
doi: 10.1507/endocrj.EJ11-0133 |
| 10 |
Zarnegar R , Young WF Jr. , Lee J , et al. The aldosteronoma resolution score: Predicting complete resolution of hypertension after adrenalectomy for aldosteronoma[J]. Ann Surg, 2008, 247 (3): 511- 518.
doi: 10.1097/SLA.0b013e318165c075 |
| 11 |
Romero-Velez G , Laird AM , Barajas ME , et al. Outcomes of adrenalectomy and the aldosteronoma resolution score in the black and hispanic population[J]. World J Surg, 2021, 45 (5): 1475- 1482.
doi: 10.1007/s00268-021-05967-y |
| 12 |
Utsumi T , Kawamura K , Imamoto T , et al. High predictive accuracy of aldosteronoma resolution score in japanese patients with aldosterone-producing adenoma[J]. Surgery, 2012, 151 (3): 437- 443.
doi: 10.1016/j.surg.2011.08.001 |
| 13 |
Pasquier L , Kirouani M , Fanget F , et al. Assessment of the aldosteronona resolution score as a predictive resolution score of hypertension after adrenalectomy for aldosteronoma in french patients[J]. Langenbecks Arch Surg, 2017, 402 (2): 309- 314.
doi: 10.1007/s00423-017-1557-x |
| 14 |
中华医学会内分泌学分会肾上腺学组. 原发性醛固酮增多症诊断治疗的专家共识[J]. 中华内分泌代谢杂志, 2016, 32 (3): 188- 195.
doi: 10.3760/cma.j.issn.1000-6699.2016.03.003 |
| 15 |
Williams TA , Lenders JWM , Mulatero P , et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: An international consensus on outcome measures and analysis of remission rates in an international cohort[J]. Lancet Diabete Endocrinol, 2017, 5 (9): 689- 699.
doi: 10.1016/S2213-8587(17)30135-3 |
| 16 |
Milliez P , Girerd X , Plouin PF , et al. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism[J]. J Am Coll Cardiol, 2005, 45 (8): 1243- 1248.
doi: 10.1016/j.jacc.2005.01.015 |
| 17 |
Stowasser M , Sharman J , Leano R , et al. Evidence for abnormal left ventricular structure and function in normotensive individuals with familial hyperaldosteronism type Ⅰ[J]. J Clin Endocrinol Metab, 2005, 90 (9): 5070- 5076.
doi: 10.1210/jc.2005-0681 |
| 18 |
Jiang SB , Guo XD , Wang HB , et al. A retrospective study of laparoscopic unilateral adrenalectomy for primary hyperaldosteronism caused by unilateral adrenal hyperplasia[J]. Int Urol Nephrol, 2014, 46 (7): 1283- 1288.
doi: 10.1007/s11255-013-0614-9 |
| 19 | Morisaki M , Kurihara I , Itoh H , et al. Predictors of clinical success after surgery for primary aldosteronism in the japanese nationwide cohort[J]. J Endocr Soc, 2019, 3 (11): 2012- 2022. |
| 20 | Vasan RS , Beiser A , Seshadri S , et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The framingham heart study[J]. Jama, 2002, 287 (8): 1003- 1010. |
| 21 | Seravalle G , Grassi G . Obesity and hypertension[J]. Pharmacol Res, 2017, 122 (1): 1- 7. |
| 22 | Nurdiantami Y , Watanabe K , Tanaka E , et al. Association of general and central obesity with hypertension[J]. Clin Nutr, 2018, 37 (4): 1259- 1263. |
| 23 | Yang Y , Williams TA , Song Y , et al. Nomogram-based preoperative score for predicting clinical outcome in unilateral primary aldosteronism[J]. J Clin Endocrinol Metab, 2020, 105 (12): e4382- e4392. |
| 24 | 何小群, 杨珊, 吴珏莅, 等. 预测原发性醛固酮增多症术后血压的转归: fisher判别模型[J]. 中华医学杂志, 2016, 96 (42): 3379- 3383. |
| [1] | 陈楚云,孙蓬飞,赵静,贾佳,范芳芳,王春燕,李建平,姜一梦,霍勇,张岩. 北京社区人群促红细胞生成素相关因素及其与10年心血管疾病风险的关系[J]. 北京大学学报(医学版), 2023, 55(6): 1068-1073. |
| [2] | 梁喆,范芳芳,张岩,秦献辉,李建平,霍勇. 中国高血压人群中H型高血压的比率和特征及与美国人群的比较[J]. 北京大学学报(医学版), 2022, 54(5): 1028-1037. |
| [3] | 马麟,吴静依,李双成,李鹏飞,张路霞. 抗高血压药物对二氧化氮长期暴露与慢性肾脏病关联的修饰效应[J]. 北京大学学报(医学版), 2022, 54(5): 1047-1055. |
| [4] | 李志胜,钱浩楠,范田园. 熔融沉积成型3D打印卡托普利与氢氯噻嗪复方片剂的制备与体外评价[J]. 北京大学学报(医学版), 2022, 54(3): 572-577. |
| [5] | 王薇,蔡林,高莹,郭晓蕙,张俊清. 原发性醛固酮增多症术后持续性重度高钾血症1例[J]. 北京大学学报(医学版), 2022, 54(2): 376-380. |
| [6] | 安文成,闫慧娴,邓正照,陈芳,欧小虹,金红心,黄薇. 原发性醛固酮增多症肾上腺切除术后慢性肾功能不全1例[J]. 北京大学学报(医学版), 2021, 53(6): 1201-1204. |
| [7] | 康文玉,王璐,邱敏,张帆,郭巍,强亚勇,拓鹏飞,宗有龙,刘磊磊,王帅帅. 肾上腺海绵状血管瘤1例及文献回顾[J]. 北京大学学报(医学版), 2021, 53(4): 808-810. |
| [8] | 杨航,杨林承,张瑞涛,凌云鹏,葛庆岗. 合并高血压、冠心病、糖尿病的新型冠状病毒肺炎患者发生病死的危险因素分析[J]. 北京大学学报(医学版), 2020, 52(3): 420-424. |
| [9] | 郑鸿尘,薛恩慈,王雪珩,陈曦,王斯悦,黄辉,江锦,叶莺,黄春兰,周筠,高文静,余灿清,吕筠,吴小玲,黄小明,曹卫华,严延生,吴涛,李立明. 基于大家系设计的静息心率与常见慢性病双表型遗传度估计[J]. 北京大学学报(医学版), 2020, 52(3): 432-437. |
| [10] | 孟文颖,黄琬桐,张杰,焦明远,金蕾,靳蕾. 孕早期血清维生素E水平与妊娠期高血压疾病发病风险的关系[J]. 北京大学学报(医学版), 2020, 52(3): 470-478. |
| [11] | 刘颖,曾祥柱,王筝,张函,王希林,袁慧书. 三维动脉自旋标记技术评价抑郁合并高血压患者脑血流灌注[J]. 北京大学学报(医学版), 2019, 51(2): 260-264. |
| [12] | 刘雪芹, 闫辉, 邱建星, 张春雨, 齐建光, 张欣, 肖慧捷, 杨艳玲, 陈永红, 杜军保. 甲基丙二酸尿症相关肺高血压临床特点与基因突变[J]. 北京大学学报(医学版), 2017, 49(5): 768-777. |
| [13] | 樊华,李汉忠,徐维锋,纪志刚,张玉石. 异位促肾上腺皮质激素综合征的外科治疗[J]. 北京大学学报(医学版), 2017, 49(4): 652-656. |
| [14] | 单娇,李宏宇,刘国峰,杨玄,董伟,简伟研,邓芙蓉,郭新彪. 大气污染对中老年高血压和心脑血管疾病患者卫生服务需求的影响:基于 CHARLS数据的分析[J]. 北京大学学报(医学版), 2016, 48(3): 460-464. |
| [15] | 章湖洋,简伟研,方海. 新型农村合作医疗的高血压患者门诊费用对住院费用的替代效应[J]. 北京大学学报(医学版), 2016, 48(3): 472-477. |
|
||