北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (6): 1106-1111. doi: 10.19723/j.issn.1671-167X.2022.06.008
系统性红斑狼疮合并视网膜病变的临床及免疫学特点
- 1. 北京大学人民医院风湿免疫科,北京 100044
2. 临汾市第三人民医院风湿免疫科,山西临汾 041000
Clinical and immunological characteristics of systemic lupus erythematosus with retinopathy
Min LI1,Lin-qing HOU1,2,Yue-bo JIN1,Jing HE1,*( )
)
- 1. Department of Rheumatology and Immunology, Peking University People's Hospital, Bejing 100044, China
2. Department of Rheumatology and Immunology, The Third People's Hospital of Linfen, Linfen 041000, Shanxi, China
摘要:
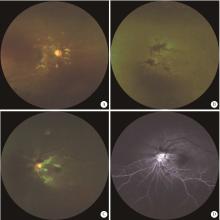
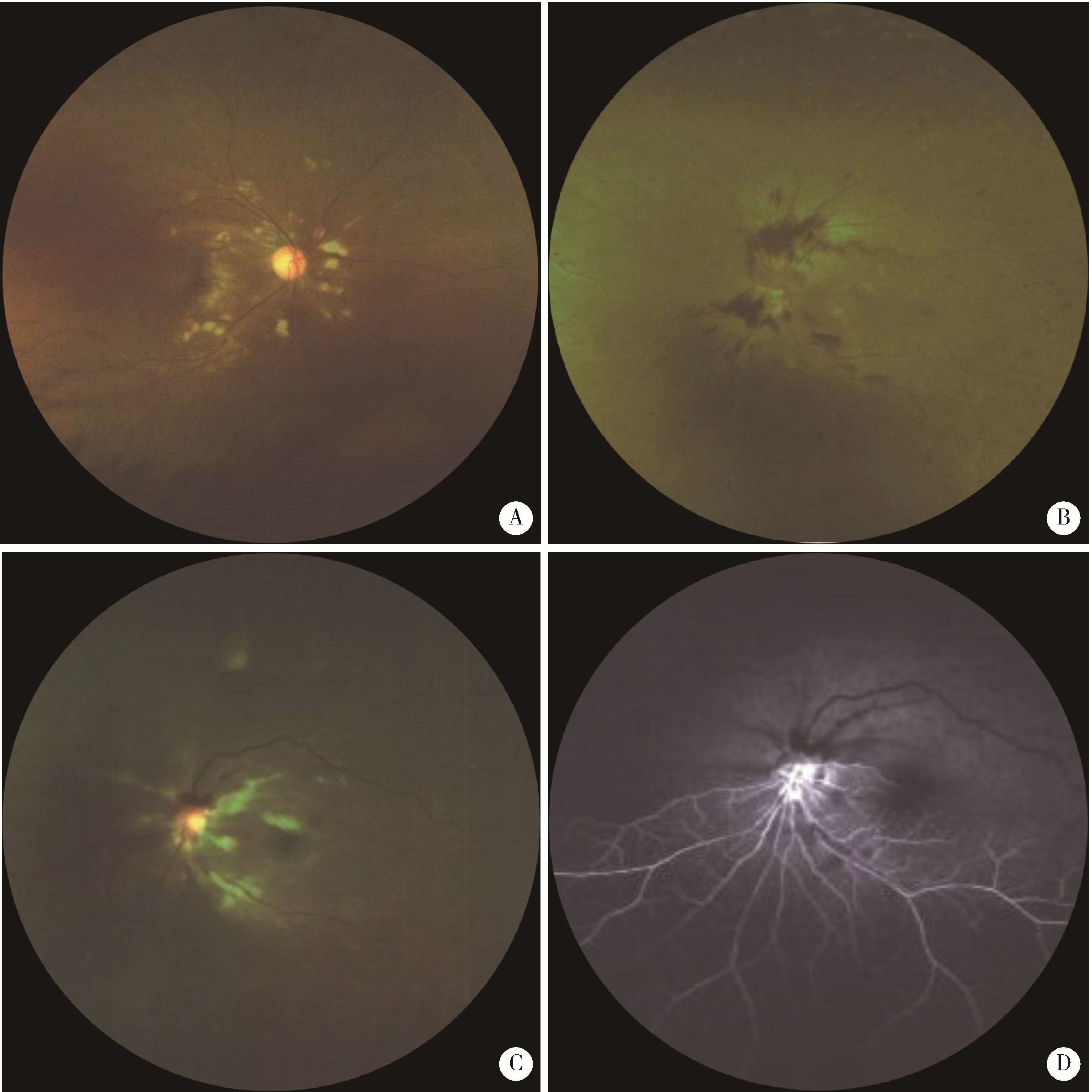
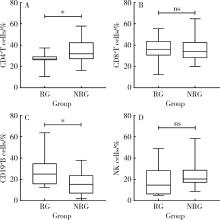
目的: 探讨系统性红斑狼疮(systemic lupus erythematosus, SLE)合并视网膜病变的临床及免疫学特点。方法: 选择2009年1月至2022年7月于北京大学人民医院住院的无高血压无糖尿病的SLE合并视网膜病变患者50例(眼病组),按性别、年龄匹配病程中无视物模糊症状及眼底检查没有视网膜病变的SLE患者50例(非眼病组),对两组患者的临床表现、实验室检查及淋巴细胞亚群进行分析。结果: 眼病组患者最常见的眼底表现为棉絮斑(33/50,66.0%),其次是视网膜出血(31/50,62.0%)。视网膜病变可发生在SLE病程的任何阶段,中位时间为1年(病程范围为20 d至30年)。眼病组出现狼疮性肾炎比例(72.0% vs. 46.0%, P=0.008)和浆膜炎比例(58.0% vs. 28.0%, P=0.002)显著高于非眼病组。眼病组同时出现神经精神性狼疮(neuropsychiatric systemic lupus erythematosus, NPSLE)比例较非眼病组升高,但差异无统计学意义。与非眼病组相比,眼病组中抗心磷脂抗体阳性比例(30.0% vs. 12.0%, P=0.027)、系统性红斑狼疮疾病活动指数评分(中位数22.0 vs. 10.5, P < 0.001)、红细胞沉降率(P < 0.001),C反应蛋白水平(P=0.019)和24 h尿蛋白定量(P=0.026)均显著升高,血红蛋白水平明显减低[(91.64±25.18) g/L vs. (113.96±18.57) g/L, P < 0.001]。与非眼病组相比,SLE视网膜病变患者外周血CD19+B细胞比例显著升高(P=0.010),CD4+T细胞比例明显减低(P=0.025),自然杀伤(natural killer,NK)细胞比例减低(P=0.051)。结论: SLE视网膜病变提示更高的SLE疾病活动性,更易合并肾脏系统、血液系统等损害,建议对所有SLE患者尽早进行眼底筛查。SLE视网膜病变患者可能存在更显著的B细胞异常增殖,应给予积极治疗以防止其他重要脏器受累。
中图分类号:
- R593.24
| 1 |
Au A , O'Day J . Review of severe vaso-occlusive retinopathy in systemic lupus erythematosus and the antiphospholipid syndrome: Associations, visual outcomes, complications and treatment[J]. Clin Exp Ophthalmol, 2004, 32 (1): 87- 100.
doi: 10.1046/j.1442-9071.2004.00766.x |
| 2 |
Moulton VR , Suarez-Fueyo A , Meidan E , et al. Pathogenesis of human systemic lupus erythematosus: A cellular perspective[J]. Trends Mol Med, 2017, 23 (7): 615- 635.
doi: 10.1016/j.molmed.2017.05.006 |
| 3 |
Dammacco R , Procaccio P , Racanelli V , et al. Ocular involvement in systemic lupus erythematosus: The experience of two tertiary referral centers[J]. Ocul Immunol Inflamm, 2018, 26 (8): 1154- 1165.
doi: 10.1080/09273948.2018.1501495 |
| 4 |
Yen YC , Weng SF , Chen HA , et al. Risk of retinal vein occlusion in patients with systemic lupus erythematosus: A population-based cohort study[J]. Br J Ophthalmol, 2013, 97 (9): 1192- 1196.
doi: 10.1136/bjophthalmol-2013-303265 |
| 5 |
Lanham JG , Barrie T , Kohner EM , et al. SLE retinopathy: Evaluation by fluorescein angiography[J]. Ann Rheum Dis, 1982, 41 (5): 473- 478.
doi: 10.1136/ard.41.5.473 |
| 6 | Hochberg MC . Updating the American college of rheumatology revised criteria for the classification of systemic lupus erythematosus[J]. Arthritis Rheum, 1997, 40 (9): 1725. |
| 7 | Gladman DD , Ibanez D , Urowitz MB . Systemic lupus erythematosus disease activity index 2000[J]. J Rheumatol, 2002, 29 (2): 288- 291. |
| 8 |
Md Noh UK , Zahidin AZA , Yong TK . Retinal vasculitis in systemic lupus erythematosus: An indication of active disease[J]. Clinics and Practice, 2012, 2 (2): 54.
doi: 10.4081/cp.2012.e54 |
| 9 |
Stafford-Brady FJ , Urowitz MB , Gladman DD , et al. Lupus retinopathy. Patterns, associations, and prognosis[J]. Arthritis Rheum, 1988, 31 (9): 1105- 1110.
doi: 10.1002/art.1780310904 |
| 10 |
Giorgi D , Pace F , Giorgi A , et al. Retinopathy in systemic lupus erythematosus: Pathogenesis and approach to therapy[J]. Hum Immunol, 1999, 60 (8): 688- 696.
doi: 10.1016/S0198-8859(99)00035-X |
| 11 |
D'Cruz D . Vasculitis in systemic lupus erythematosus[J]. Lupus, 1998, 7 (4): 270- 274.
doi: 10.1191/096120398678920082 |
| 12 |
Kharel R , Shah DN , Singh D . Role of lupus retinopathy in systemic lupus erythematosus[J]. Ophthalmic Inflamm Infect, 2016, 6 (1): 1- 4.
doi: 10.1186/s12348-015-0068-6 |
| 13 |
Seth G , Chengappa KG , Misra DP , et al. Lupus retinopathy: A marker of active systemic lupus erythematosus[J]. Rheum Int, 2018, 38 (8): 1495- 1501.
doi: 10.1007/s00296-018-4083-4 |
| 14 |
曹绪胜, 纪海霞, 张永鹏, 等. 全身使用糖皮质激素继发中心性浆液性脉络膜视网膜病变的临床特征[J]. 眼科, 2020, 29 (3): 193- 197.
doi: 10.3969/j.issn.1006-8422.2020.03.001 |
| 15 |
Million M , Raoult D . The pathogenesis of the antiphospholipid syndrome[J]. N Engl J Med, 2013, 368 (24): 2335.
doi: 10.1056/NEJMc1300484 |
| 16 |
Jeon S , Lee WK . Aggravated capillary non-perfusion after intravitreal bevacizumab for macular edema secondary to systemic lupus erythematosus and anti-phospholipid syndrome[J]. Lupus, 2012, 21 (3): 335- 337.
doi: 10.1177/0961203311422095 |
| 17 | Zhu W , Wu Y , Xu M , et al. Correction: Antiphospholipid antibody and risk of retinal vein occlusion: A systematic review and meta-analysis[J]. PLoS One, 2016, 11 (6): e157536. |
| 18 |
Lipsky PE . Systemic lupus erythematosus: An autoimmune disease of B cell hyperactivity[J]. Nat Immunol, 2001, 2 (9): 764- 766.
doi: 10.1038/ni0901-764 |
| 19 |
Wei C , Anolik J , Cappione A , et al. A new population of cells lacking expression of CD27 represents a notable component of the B cell memory compartment in systemic lupus erythematosus[J]. J Immunol, 2007, 178 (10): 6624- 6633.
doi: 10.4049/jimmunol.178.10.6624 |
| 20 |
Hickman RA , Denniston AK , Yee CS , et al. Bilateral retinal vasculitis in a patient with systemic lupus erythematosus and its remission with rituximab therapy[J]. Lupus, 2010, 19 (3): 327- 329.
doi: 10.1177/0961203309347332 |
| 21 |
Damato E , Chilov M , Lee R , et al. Plasma exchange and rituximab in the management of acute occlusive retinal vasculopathy secondary to systemic lupus erythematosus[J]. Ocul Immunol Inflamm, 2011, 19 (5): 379- 381.
doi: 10.3109/09273948.2011.603069 |
| 22 |
Tselios K , Lam WC , Urowitz MB , et al. Rituximab for sight-threatening lupus-related retinal vasculitis[J]. J Clin Rheumatol, 2018, 24 (2): 93- 94.
doi: 10.1097/RHU.0000000000000600 |
| 23 |
Liu M , Liu J , Zhang X , et al. Activation status of CD56(dim) natural killer cells is associated with disease activity of patients with systemic lupus erythematosus[J]. Clin Rheumatol, 2021, 40 (3): 1103- 1112.
doi: 10.1007/s10067-020-05306-x |
| [1] | 武志慧, 胡明智, 赵巧英, 吕凤凤, 张晶莹, 张伟, 王永福, 孙晓林, 王慧. miR-125b-5p修饰脐带间充质干细胞对系统性红斑狼疮的免疫调控机制[J]. 北京大学学报(医学版), 2024, 56(5): 860-867. |
| [2] | 乔佳佳,田聪,黄晓波,刘军. 肾结石合并系统性红斑狼疮行经皮肾镜碎石取石术的安全性和有效性评估[J]. 北京大学学报(医学版), 2024, 56(4): 745-749. |
| [3] | 任立敏,赵楚楚,赵义,周惠琼,张莉芸,王友莲,沈凌汛,范文强,李洋,厉小梅,王吉波,程永静,彭嘉婧,赵晓珍,邵苗,李茹. 系统性红斑狼疮低疾病活动度及缓解状况的真实世界研究[J]. 北京大学学报(医学版), 2024, 56(2): 273-278. |
| [4] | 冯璐,翟佳羽,赵金霞. IgG4相关性疾病患者就诊情况及其临床特征[J]. 北京大学学报(医学版), 2023, 55(6): 1028-1032. |
| [5] | 罗芷筠,吴佳佳,宋优,梅春丽,杜戎. 伴神经精神系统病变的系统性红斑狼疮相关巨噬细胞活化综合征2例[J]. 北京大学学报(医学版), 2023, 55(6): 1111-1117. |
| [6] | 姚海红,杨帆,唐素玫,张霞,何菁,贾园. 系统性红斑狼疮及成人Still病合并巨噬细胞活化综合征的临床特点及诊断指标[J]. 北京大学学报(医学版), 2023, 55(6): 966-974. |
| [7] | 赵祥格,刘佳庆,黄会娜,陆智敏,白自然,李霞,祁荆荆. 干扰素-α介导系统性红斑狼疮外周血CD56dimCD57+自然杀伤细胞功能的损伤[J]. 北京大学学报(医学版), 2023, 55(6): 975-981. |
| [8] | 刘蕊,赵金霞,闫良. 类风湿关节炎合并下肢静脉血栓患者的临床特点[J]. 北京大学学报(医学版), 2022, 54(6): 1079-1085. |
| [9] | 张琳崎,赵静,王红彦,王宗沂,李英妮,汤稷旸,李思莹,曲进锋,赵明威. 抗ENO1抗体与狼疮性视网膜病变的相关性[J]. 北京大学学报(医学版), 2022, 54(6): 1099-1105. |
| [10] | 邵苗,郭惠芳,雷玲彦,赵清,丁艳杰,林进,吴锐,于峰,李玉翠,苗华丽,张莉芸,杜燕,焦瑞英,庞丽霞,龙丽,栗占国,李茹. 短间期小剂量环磷酰胺治疗系统性红斑狼疮耐受性的多中心对照研究[J]. 北京大学学报(医学版), 2022, 54(6): 1112-1116. |
| [11] | 邹健梅,武丽君,罗采南,石亚妹,吴雪. 血清25-羟维生素D与系统性红斑狼疮活动的关系[J]. 北京大学学报(医学版), 2021, 53(5): 938-941. |
| [12] | 夏芳芳,鲁芙爱,吕慧敏,杨国安,刘媛. 系统性红斑狼疮伴间质性肺炎的临床特点及相关因素分析[J]. 北京大学学报(医学版), 2021, 53(2): 266-272. |
| [13] | 张庆芬,赵红,冯艺. 不同全身麻醉管理方式与早产儿眼底手术临床结局[J]. 北京大学学报(医学版), 2021, 53(1): 195-199. |
| [14] | 包芳,史尉利,胡静,张娣,高东晗,夏云霞,景红梅,克晓燕,葛庆岗,沈宁. 新型冠状病毒肺炎淋巴细胞亚群与严重程度的相关分析[J]. 北京大学学报(医学版), 2020, 52(6): 1075-1081. |
| [15] | 魏士雄,黎苏佳,刘毅. 幼年特发性关节炎成人后的临床特点及生物制剂治疗[J]. 北京大学学报(医学版), 2020, 52(6): 1014-1022. |
|
||