北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (6): 1045-1052. doi: 10.19723/j.issn.1671-167X.2023.06.014
未分化结缔组织病患者的妊娠结局、疾病演变及其影响因素
- 1. 北京大学人民医院风湿免疫科, 北京 100044
2. 重庆市中医院肾病风湿免疫科, 重庆 400011
3. 重庆市渝北区人民医院中医科, 重庆 401120
Analysis of pregnancy outcomes, disease progression, and risk factors in patients with undifferentiated connective tissue disease
Fang-ning YOU1,2,Liang LUO3,Xiang-jun LIU1,Xue-wu ZHANG1,Chun LI1,*( )
)
- 1. Department of Rheumatology and Immunology, Peking University People's Hospital, Beijing 100044, China
2. Department of Nephropathy and Rheumatology, Chongqing Hospital of Traditional Chinese Medicine, Chongqing 400011, China
3. Department of Chinese Medicine, the People's Hospital of Yubei District of Chongqing City, Chongqing 401120, China
摘要:
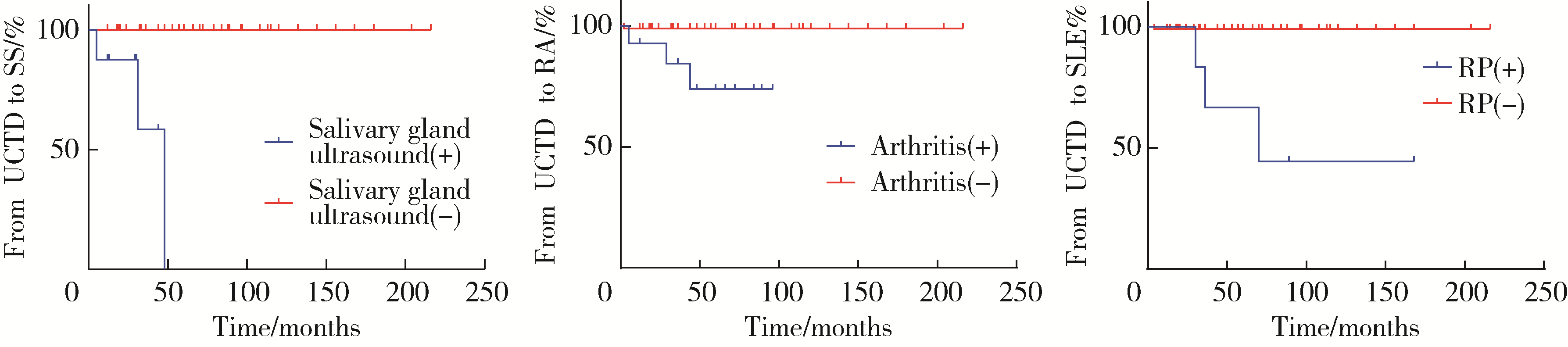
目的: 研究未分化结缔组织病(undifferentiated connective tissue disease, UCTD)患者的妊娠结局、疾病演变及其影响因素。方法: 选择2009年1月至2022年8月在北京大学人民医院就诊并且符合UCTD分类标准孕妇的病例资料进行回顾性分析; 106例UCTD孕妇根据妊娠结局分为不良妊娠结局组(adverse pregnancy outcomes, APOs)(53例)和无APOs组(53例), 比较两组患者临床表现、实验室指标及妊娠结局的差异。不良妊娠结局包括流产、早产、子痫前期、胎膜早破(premature rupture of membranes, PROM)、宫内生长受限(intrauterine growth restriction, IUGR)、产后出血(postpartum hemorrhage, PPH)、死胎、小于胎龄儿(small for gestational age infant, SGA)、低出生体质量(low birth weight infant, LBW)、出生缺陷。采用Logistic回归分析不良妊娠结局的危险因素, 使用Kaplan-Meier法进行生存分析, 通过Cox回归分析筛选出UCTD演变为明确CTD的危险因素。结果: 在106例UCTD患者中, 99例(93.39%)为活产, 4例(3.77%)死胎, 3例(2.83%)流产, 20例(18.86%)早产, 6例(5.66%)SGA, 17例(16.03%)LBW, 11例(10.37%)子痫前期, 7例(6.60%)IUGR, 19例(17.92%)PROM, 10例(9.43%)PPH。APOs组抗SSA抗体阳性率较无APOs组更高(73.58% vs. 54.71%, P=0.036), 白细胞减少比例更高(15.09% vs. 3.77%, P=0.046), 血红蛋白水平较无APOs组明显降低[109.00 (99.50, 118.00) g/L vs. 124.00 (111.50, 132.00) g/L, P < 0.001]。多因素Logistic回归分析显示白细胞减少(OR=0.827, 95%CI: 0.688~0.994)是UCTD患者发生APOs的独立危险因素(P=0.042)。15例(14.15%)UCTD在平均随访5.00(3.00, 7.00)年内演变为明确的结缔组织病, 其中干燥综合征8例(7.54%), 系统性红斑狼疮(systemic lupus erythematosus, SLE)4例(3.77%), 类风湿关节炎4例(3.77%), 混合性结缔组织病1例(0.94%)。雷诺现象(Raynaud phenomenon, RP) (HR=40.157, 95%CI: 3.172~508.326)是UCTD患者妊娠期及产后演变为SLE的独立危险因素(P=0.003)。结论: 白细胞减少是UCTD患者发生APOs的独立危险因素, 雷诺现象是UCTD患者演变为SLE的独立危险因素, 严格的疾病监测、定期随访是预防UCTD合并妊娠患者发生不良妊娠结局和预测疾病演变的关键措施。
中图分类号:
- R593.2
| 1 |
Mosca M , Tani C , Neri C , et al. Undifferentiated connective tissue diseases (UCTD)[J]. Autoimm Rev, 2006, 6 (1): 1- 4.
doi: 10.1016/j.autrev.2006.03.004 |
| 2 | García-González M , Rodríguez-Lozano B , Bustabad S , et al. Undifferentiated connective tissue disease: Predictors of evolution into definite disease[J]. Clin Exp Rheumatol, 2017, 35 (5): 739- 745. |
| 3 |
Mecacci F , Pieralli A , Bianchi B , et al. The impact of autoimmune disorders and adverse pregnancy outcome[J]. Semin Perinatol, 2007, 31 (4): 223- 226.
doi: 10.1053/j.semperi.2007.05.005 |
| 4 | Mosca M , Neri R , Bombardieri S . Undifferentiated connective tissue diseases (UCTD): A review of the literature and a proposal for preliminary classification criteria[J]. Clin Exp Rheumatol, 1999, 17 (5): 615- 620. |
| 5 |
Practice Committee of the American Society for Reproductive Medicine . Evaluation and treatment of recurrent pregnancy loss: A committee opinion[J]. Fertil Steril, 2012, 98 (5): 1103- 1111.
doi: 10.1016/j.fertnstert.2012.06.048 |
| 6 |
Vogel JP , Chawanpaiboon S , Moller AB , et al. The global epidemiology of preterm birth[J]. Best Pract Res Clin Obstet Gynaecol, 2018, 52, 3- 12.
doi: 10.1016/j.bpobgyn.2018.04.003 |
| 7 | Tyas BD , Lestari P , Akbar MIA . Maternal perinatal outcomes related to advanced maternal age in preeclampsia pregnant women[J]. J Family Reprod Health, 2019, 13 (4): 191- 200. |
| 8 |
Sharma D , Shastri S , Farahbakhsh N , et al. Intrauterine growth restriction: Part 1[J]. J Matern Fetal Neonatal Med, 2016, 29 (24): 3977- 3987.
doi: 10.3109/14767058.2016.1152249 |
| 9 |
American College of Obstetricians and Gynecologists' Committee on Practice Bulletins-Obstetrics . Practice bulletin No.172: Premature rupture of membranes[J]. Obstet Gynecol, 2016, 128 (4): 165- 177.
doi: 10.1097/AOG.0000000000001712 |
| 10 | Sheldon WR , Blum J , Vogel JP , et al. Postpartum haemorrhage management, risks, and maternal outcomes: Findings from the World Health Organization Multicountry Survey on Maternal and Newborn Health[J]. BJOG, 2014, 121 (Suppl 1): 5- 13. |
| 11 |
Robinson GE . Pregnancy loss[J]. Best Pract Res Clin Obstet Gynaecol, 2014, 28 (1): 169- 178.
doi: 10.1016/j.bpobgyn.2013.08.012 |
| 12 |
Bertino E , Spada E , Occhi L , et al. Neonatal anthropometric charts: The Italian neonatal study compared with other European studies[J]. J Pediatr Gastroenterol Nutr, 2010, 51 (3): 353- 361.
doi: 10.1097/MPG.0b013e3181da213e |
| 13 |
Krasevec J , Blencowe H , Coffey C , et al. Study protocol for UNICEF and WHO estimates of global, regional, and national low birthweight prevalence for 2000 to 2020[J]. Gates Open Res, 2022, 6, 80- 93.
doi: 10.12688/gatesopenres.13666.1 |
| 14 | World Health Organization (WHO). Sixty-third world health assembly. Birth defects[R]. Geneva: WHO, 2010. |
| 15 |
Ostensen M , Andreoli L , Brucato A , et al. State of the art: Reproduction and pregnancy in rheumatic diseases[J]. Autoimmun Rev, 2015, 14 (5): 376- 386.
doi: 10.1016/j.autrev.2014.12.011 |
| 16 |
Goldenberg RL , Culhane JF , Iams JD , et al. Epidemiology and causes of preterm birth[J]. Lancet, 2008, 371 (9606): 75- 84.
doi: 10.1016/S0140-6736(08)60074-4 |
| 17 |
Radin M , Schreiber K , Cecchi I , et al. A Multicentre study of 244 pregnancies in undifferentiated connective tissue disease: Maternal/fetal outcomes and disease evolution[J]. Rheumatology (Oxford), 2020, 59 (9): 2412- 2418.
doi: 10.1093/rheumatology/kez620 |
| 18 |
Muñoz Muñoz1 C , Ahmed K , Thomas M , et al. Comparing pregnancy outcomes in patients with criteria and non-criteria autoimmune disease: A systematic review[J]. Lupus, 2022, 31 (1): 5- 18.
doi: 10.1177/09612033211061850 |
| 19 |
Haase I , Fischer-Betz R . State of the art: Fertility and pregnancy in rheumatic diseases[J]. Z Rheumatol, 2021, 80 (8): 699- 706.
doi: 10.1007/s00393-021-01073-5 |
| 20 |
Luo L , Li XR , Li C , et al. Risk factors for adverse pregnancy outcomes in women with rheumatoid arthritis and follow-up of their offspring[J]. Clin Rheumatol, 2022, 41 (10): 3135- 3141.
doi: 10.1007/s10067-022-06233-9 |
| 21 |
Erden A , Apaydın H , Fanouriakis A , et al. Performance of the systemic lupus erythematosus risk probability index in a cohort of undifferentiated connective tissue disease[J]. Rheumatology (Oxford), 2022, 61 (9): 3606- 3613.
doi: 10.1093/rheumatology/keac005 |
| 22 |
张晓英, 温鸿雁, 陈俊伟, 等. 未分化结缔组织病合并骨髓增生异常综合征1例[J]. 北京大学学报(医学版), 2012, 44 (2): 316- 319.
doi: 10.3969/j.issn.1671-167X.2012.02.033 |
| 23 |
Lin L , Wei Y , Zhu W , et al. Prevalence, risk factors and associated adverse pregnancy outcomes of anaemia in Chinese pregnant women: A multicentre retrospective study[J]. BMC Pregnancy Childbirth, 2018, 18 (1): 111- 118.
doi: 10.1186/s12884-018-1739-8 |
| 24 |
Li M , Huang SJ . Innate immunity, coagulation and placenta related adverse pregnancy outcomes[J]. Thromb Res, 2009, 124 (6): 656- 662.
doi: 10.1016/j.thromres.2009.07.012 |
| 25 | 孔德璇, 张志坤, 李慧东. 系统性红斑狼疮与孕产妇不良妊娠结局的相关性[J]. 中国妇幼保健, 2022, 37 (10): 1865- 1868. |
| 26 |
Klein A , Molad Y . Hematological manifestations among patients with rheumatic diseases[J]. Acta Haematol, 2021, 144 (4): 403- 412.
doi: 10.1159/000511759 |
| 27 |
Wang F , Jia W , Fan M , et al. Single cell immune landscape of human recurrent miscarriage[J]. Genomics Proteomics Bioinformatics, 2021, 19 (2): 208- 222.
doi: 10.1016/j.gpb.2020.11.002 |
| 28 | Cavazzana I , Franceschini F , Belfiore N , et al. Undifferentiated connective tissue disease with antibodies to Ro/SSa: Clinical features and follow-up of 148 patients[J]. Clin Exp Rheumatol, 2001, 19 (4): 403- 409. |
| 29 |
Tektonidou MG , Andreoli L , Limper M , et al. EULAR recommendations for the management of antiphospholipid syndrome in adults[J]. Ann Rheum Dis, 2019, 78 (10): 1296- 1304.
doi: 10.1136/annrheumdis-2019-215213 |
| 30 |
Duan JN , Ma D , Wen XT , et al. Hydroxychloroquine prophylaxis for preeclampsia, hypertension and prematurity in pregnant patients with systemic lupus erythematosus: A meta-analysis[J]. Lupus, 2021, 30 (7): 1163- 1174.
doi: 10.1177/09612033211007199 |
| [1] | 李志存, 吴天俣, 梁磊, 范宇, 孟一森, 张骞. 穿刺活检单针阳性前列腺癌术后病理升级的危险因素分析及列线图模型构建[J]. 北京大学学报(医学版), 2024, 56(5): 896-901. |
| [2] | 颜野,李小龙,夏海缀,朱学华,张羽婷,张帆,刘可,刘承,马潞林. 前列腺癌根治术后远期膀胱过度活动症的危险因素[J]. 北京大学学报(医学版), 2024, 56(4): 589-593. |
| [3] | 陈延,李况蒙,洪锴,张树栋,程建星,郑仲杰,唐文豪,赵连明,张海涛,姜辉,林浩成. 阴茎海绵体注射试验对阴茎血管功能影响的回顾性研究[J]. 北京大学学报(医学版), 2024, 56(4): 680-686. |
| [4] | 庞博,郭桐君,陈曦,郭华棋,石嘉章,陈娟,王欣梅,李耀妍,单安琪,余恒意,黄婧,汤乃军,王艳,郭新彪,李国星,吴少伟. 天津与上海35岁以上人群氮氧化物个体暴露水平及其影响因素[J]. 北京大学学报(医学版), 2024, 56(4): 700-707. |
| [5] | 和静,房中则,杨颖,刘静,马文瑶,霍勇,高炜,武阳丰,谢高强. 血浆中脂质代谢分子与颈动脉粥样硬化斑块、传统心血管危险因素及膳食因素的关系[J]. 北京大学学报(医学版), 2024, 56(4): 722-728. |
| [6] | 蔡珊,张依航,陈子玥,刘云飞,党佳佳,师嫡,李佳欣,黄天彧,马军,宋逸. 北京市中小学生身体活动时间现状及影响因素的路径[J]. 北京大学学报(医学版), 2024, 56(3): 403-410. |
| [7] | 张祖洪,陈天娇,马军. 中小学生青春发动时相与心血管代谢危险因素的相关性[J]. 北京大学学报(医学版), 2024, 56(3): 418-423. |
| [8] | 林郁婷,王华丽,田宇,巩俐彤,常春. 北京市老年人认知功能的影响因素[J]. 北京大学学报(医学版), 2024, 56(3): 456-461. |
| [9] | 朱金荣,赵亚娜,黄巍,赵微微,王悦,王松,苏春燕. 感染新型冠状病毒的血液透析患者的临床特征[J]. 北京大学学报(医学版), 2024, 56(2): 267-272. |
| [10] | 赖展鸿,李嘉辰,贠泽霖,张永刚,张昊,邢晓燕,邵苗,金月波,王乃迪,李依敏,李玉慧,栗占国. 特发性炎性肌病完全临床应答相关因素的单中心真实世界研究[J]. 北京大学学报(医学版), 2024, 56(2): 284-292. |
| [11] | 司筱芊,赵秀娟,朱凤雪,王天兵. 创伤出血性休克后急性呼吸窘迫综合征的危险因素[J]. 北京大学学报(医学版), 2024, 56(2): 307-312. |
| [12] | 李洋洋,侯林,马紫君,黄山雅美,刘捷,曾超美,秦炯. 孕期因素与婴儿牛奶蛋白过敏的关系[J]. 北京大学学报(医学版), 2024, 56(1): 144-149. |
| [13] | 刘晓强,周寅. 牙种植同期植骨术围术期高血压的相关危险因素[J]. 北京大学学报(医学版), 2024, 56(1): 93-98. |
| [14] | 罗靓,李云,王红彦,相晓红,赵静,孙峰,张晓盈,贾汝琳,李春. 抗内皮细胞抗体检测在早期流产中的预测价值[J]. 北京大学学报(医学版), 2023, 55(6): 1039-1044. |
| [15] | 李宇菲,闫亚妮,靳家扬,李春,裴秋艳. 合并胎儿心脏病变的抗SSA抗体阳性孕妇的临床及实验室特征[J]. 北京大学学报(医学版), 2023, 55(6): 1053-1057. |
|
||