北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (1): 57-65. doi: 10.19723/j.issn.1671-167X.2024.01.010
基于下颌运动轨迹的正颌外科术中下颌骨髁突定位方法及初步精度验证
- 北京大学口腔医学院·口腔医院口腔颌面外科,国家口腔医学中心,国家口腔疾病临床医学研究中心,口腔生物材料和数字诊疗装备国家工程研究中心,口腔数字医学北京市重点实验室,北京 100081
Mandibular condyle localization in orthognathic surgery based on mandibular movement trajectory and its preliminary accuracy verification
Xinyu XU,Ling WU,Fengqi SONG,Zili LI,Yi ZHANG,Xiaojing LIU*( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
摘要:
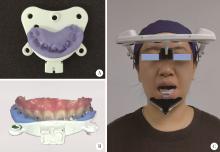
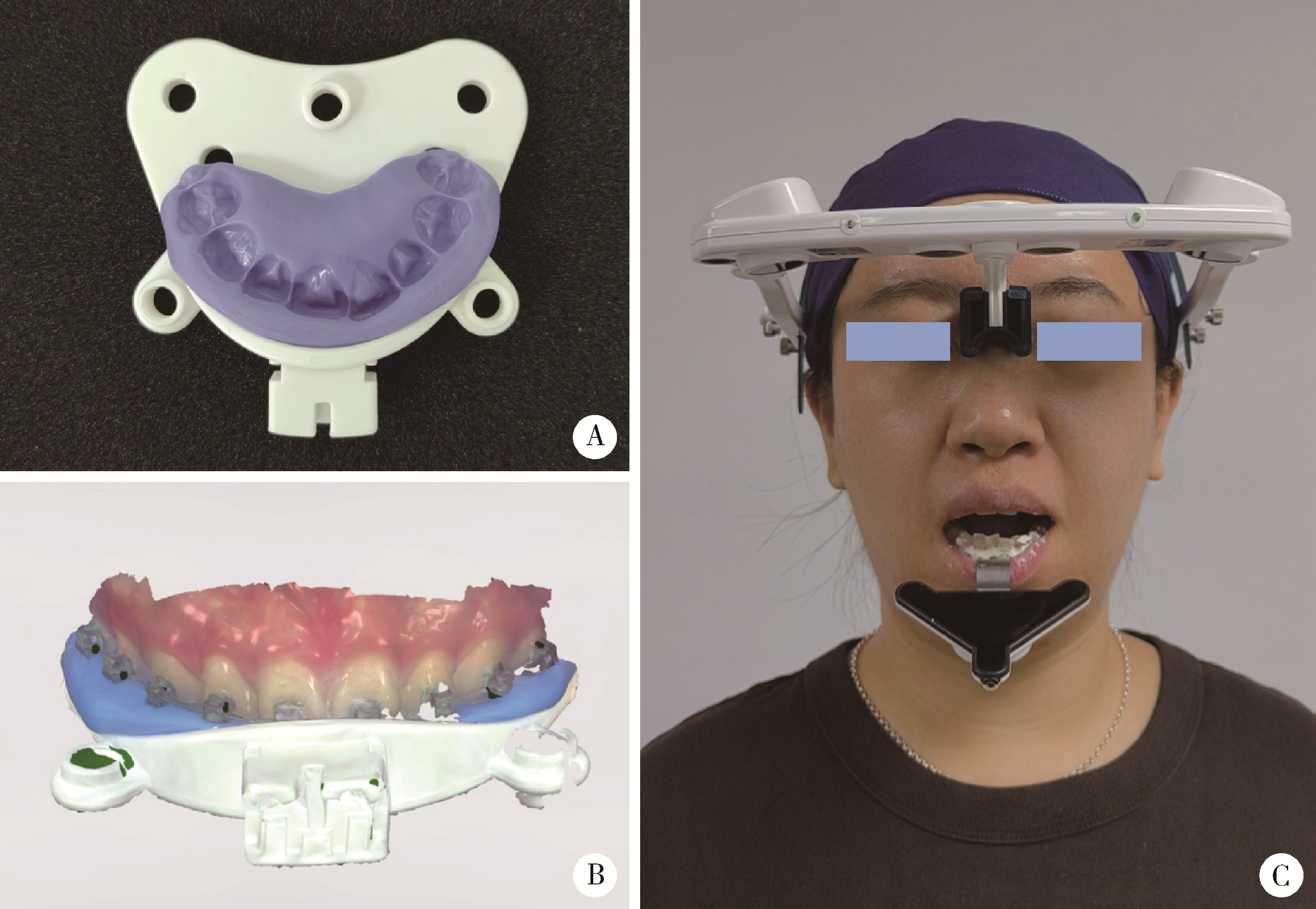
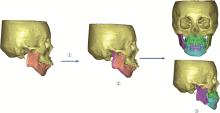
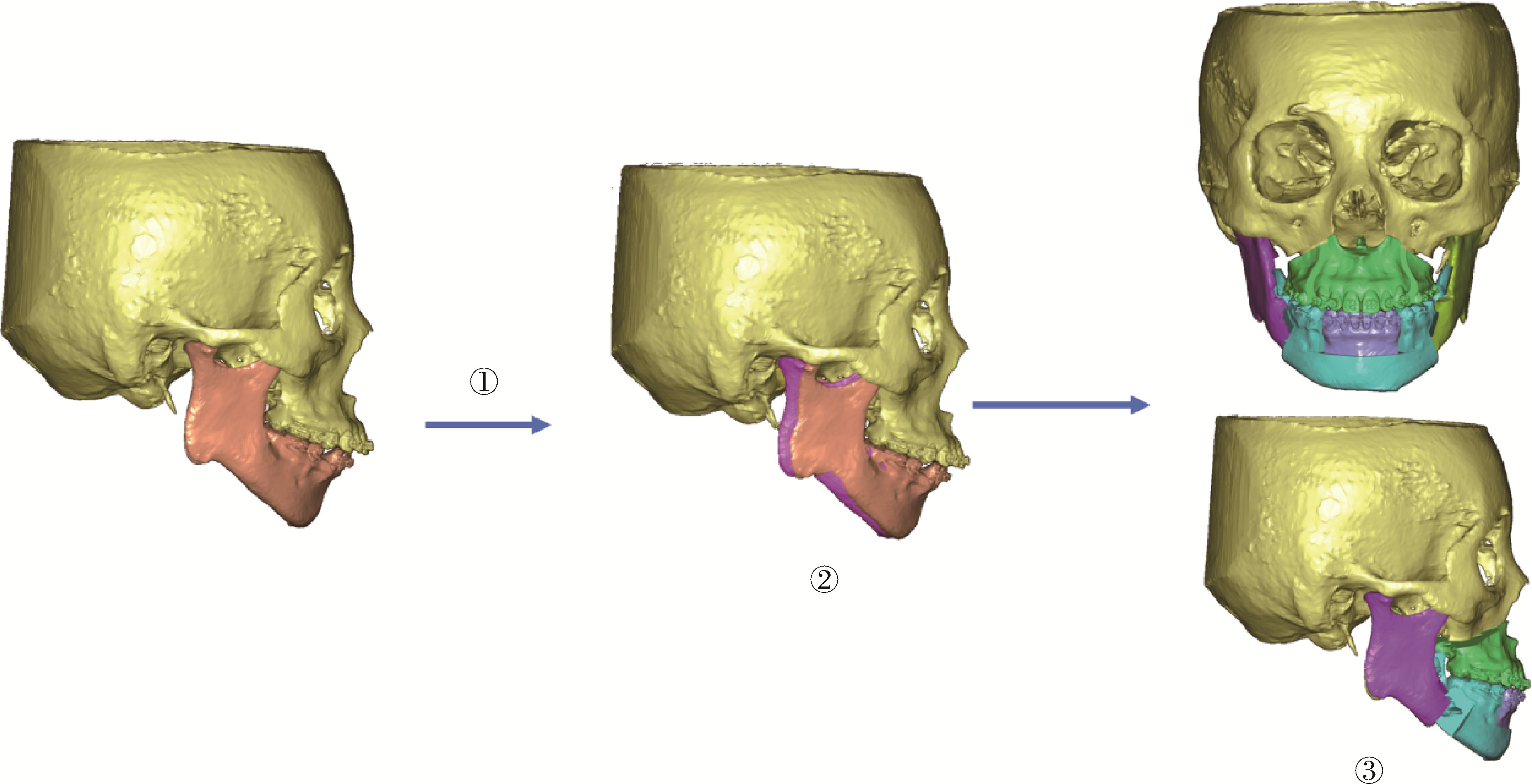
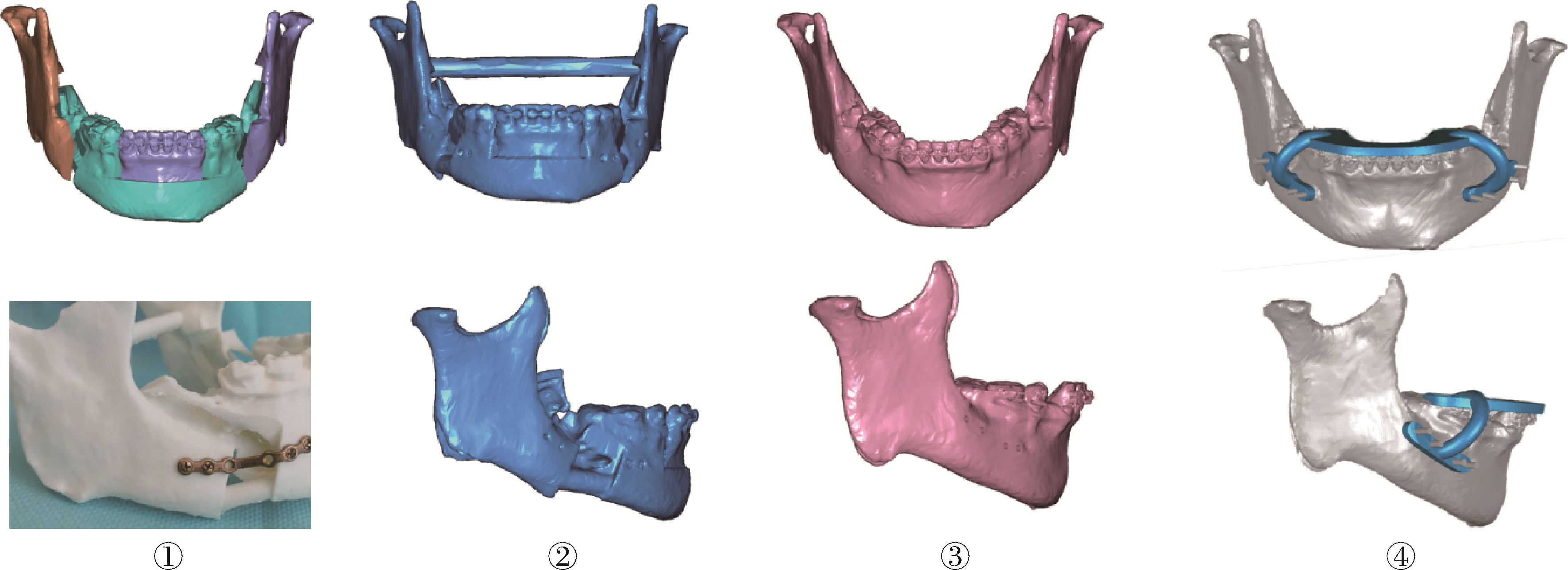
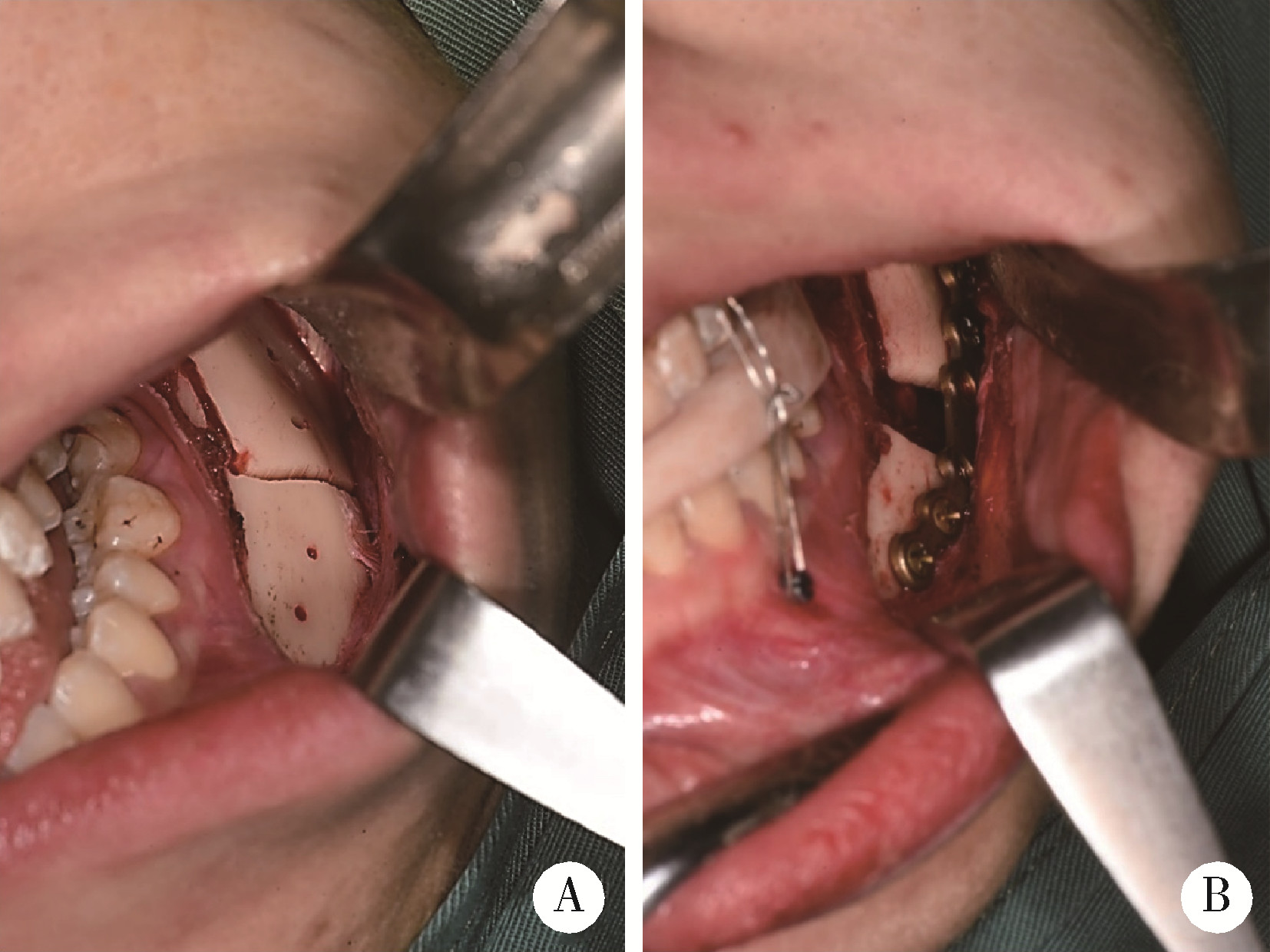
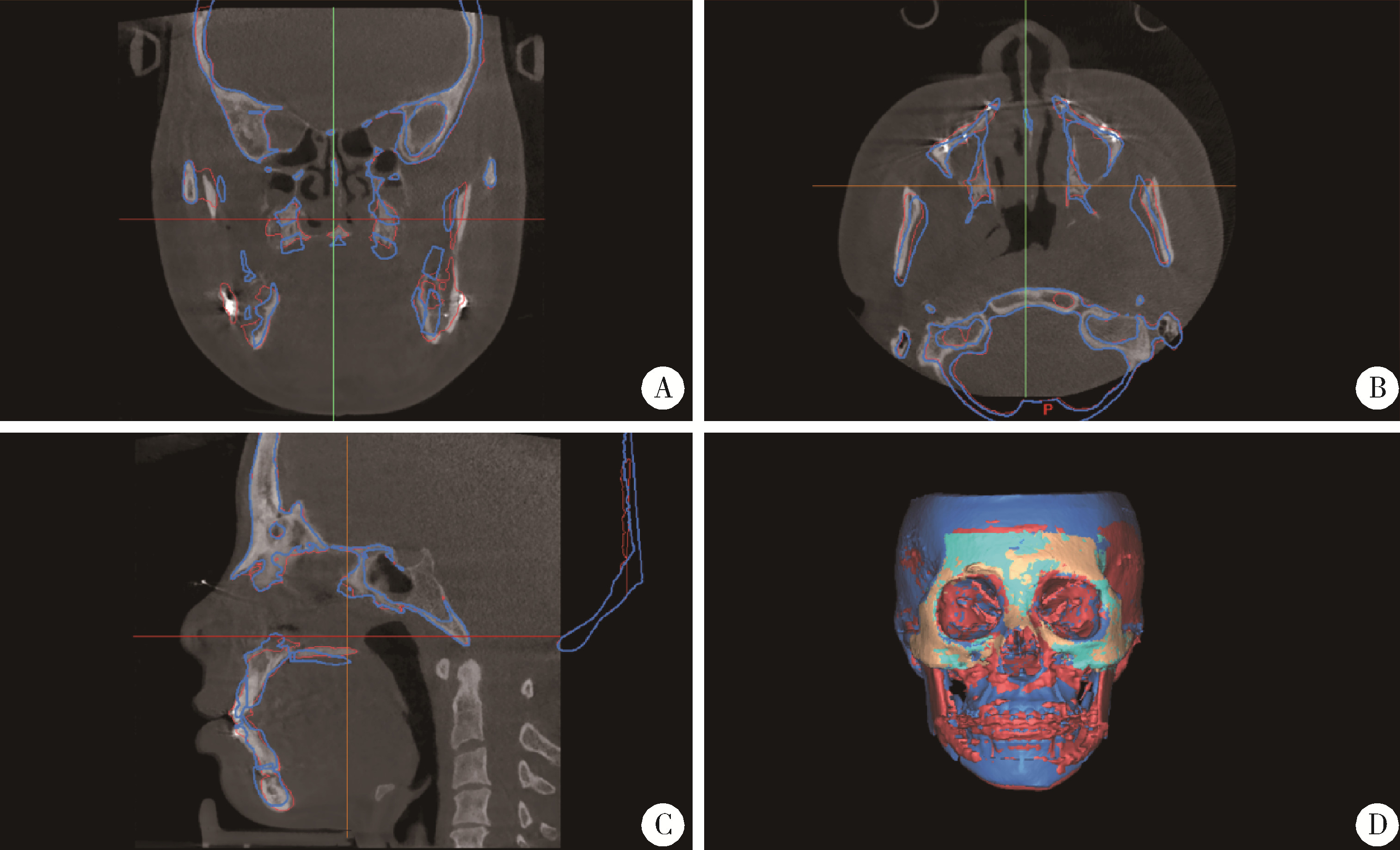
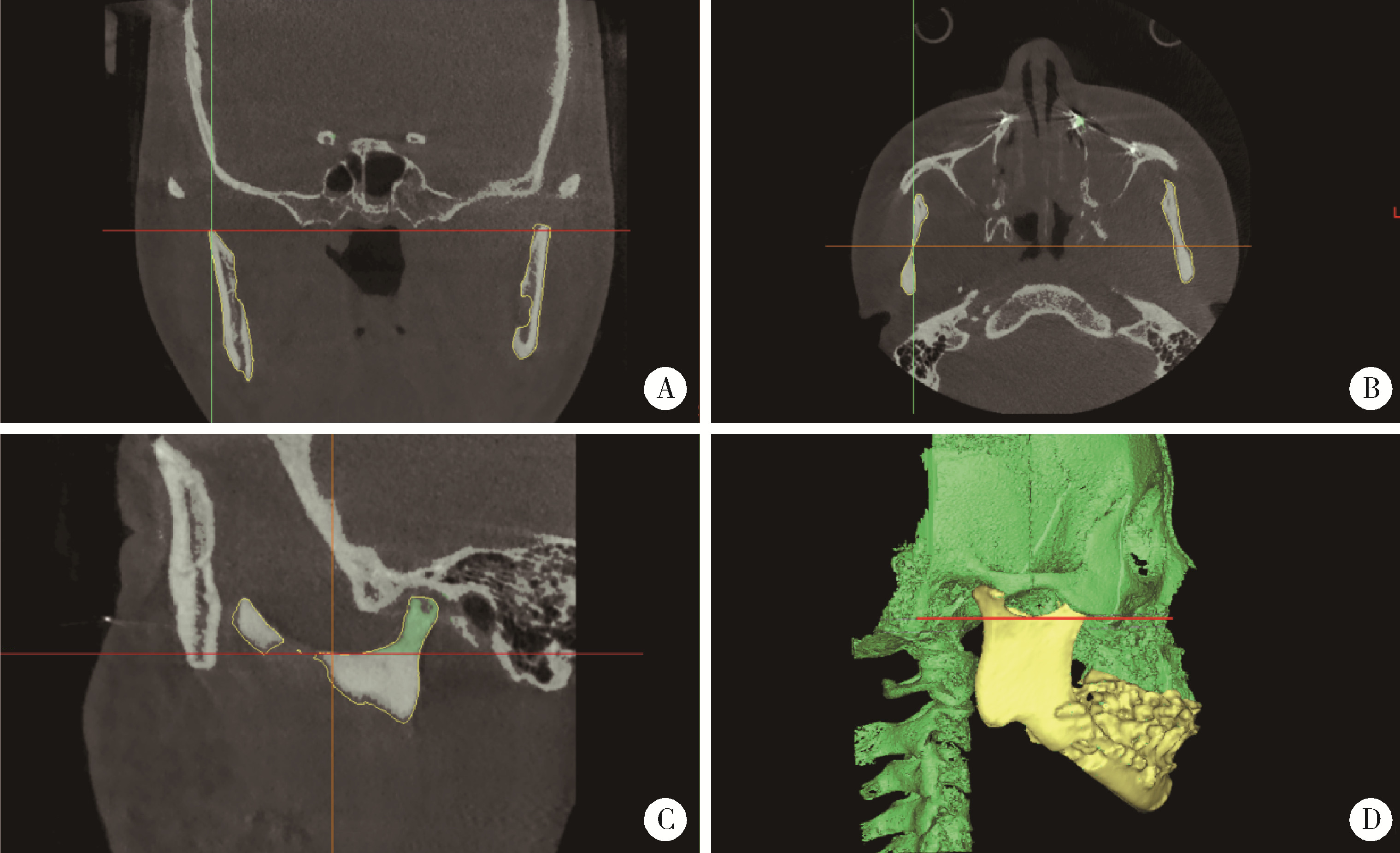
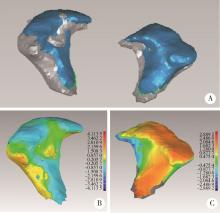
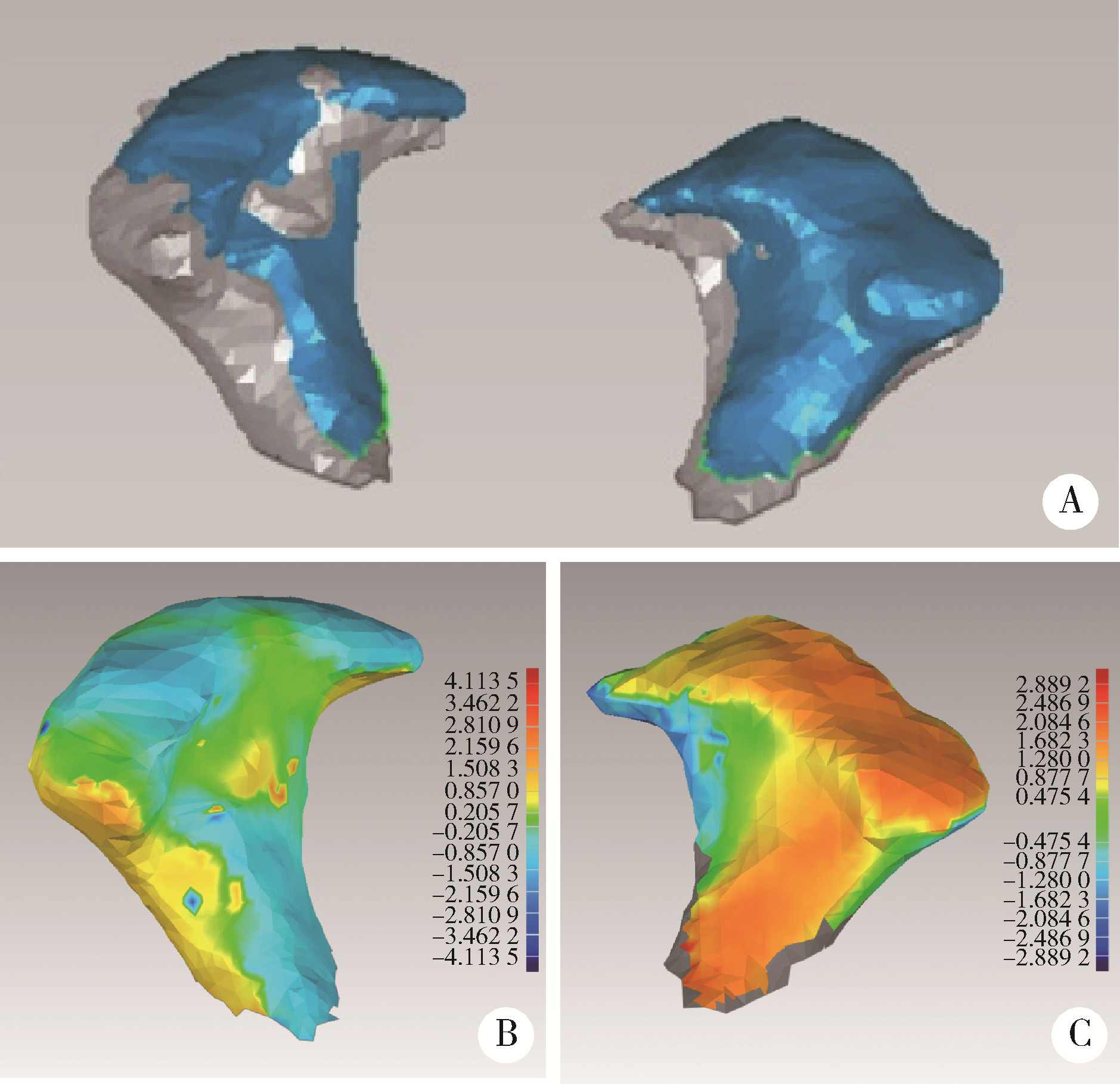
目的: 基于下颌运动轨迹建立正颌手术下颌骨髁突位置的术前规划和术中定位技术流程,并对其定位准确性进行评价。方法: 通过大视野锥形束计算机体层摄影术(cone beam computed tomography, CBCT)和口内扫描分别获得面部骨组织和牙齿的三维数据,采用下颌运动记录仪记录患者下颌生理状态下各方向运动时的下颌运动轨迹。使用IVSPlan l.0.25软件,通过数据分割、三维重建得到上、下颌骨的三维模型,通过标志点配准将牙列数据与颌骨数据融合,将下颌运动记录仪得到的数据转化为下颌骨相对于上颌骨的矩阵变换方程组,通过下颌骨三维数据的矩阵变换得到不同时刻下颌骨髁突的坐标位置,并通过软件可视化呈现其三维运动轨迹。由一名具有颞下颌关节病诊治和正颌外科手术双专业背景的高年资口腔颌面外科医师在可视化界面上筛选合适的下颌骨髁突位置作为近心骨段的术后位置,常规进行正颌外科设计,基于咬合关系和面型设计远心骨段位置,将近、远心骨段数据融合得到术后下颌骨形态,通过3D打印得到实体模型。在实体模型上预成型钛板、打孔,设计下颌骨髁突定位导板。手术中,通过下颌骨髁突定位导板和预成型钛板引导包含下颌骨髁突的近心骨段就位于术前设计位置。通过10例骨性Ⅱ类牙颌面畸形患者验证该流程在双侧下颌升支矢状劈开截骨术(sagittal split ramus osteotomy, SSRO)中定位下颌骨髁突的准确性。误差的计算方法为术前设计与术后2周CBCT实际下颌骨髁突表面距离的均方根(root mean square, RMS)。结果: 术前设计下颌骨髁突位置与术后2周的实际位置相比,下颌骨髁突表面平均距离的RMS为(1.59±0.36) mm,95%CI:1.35~1.70 mm,小于2 mm的专家共识建议值(P < 0.05)。结论: 下颌运动轨迹对正颌外科手术设计中确定包含下颌骨髁突的近心骨段位置可能具有指导作用,使用下颌骨髁突定位装置和预成型钛板术中引导下颌骨髁突就位的精度可以满足临床需求。
中图分类号:
- R782.2
| 1 |
Apostolakis D , Michelinakis G , Kamposiora P , et al. The current state of computer assisted orthognathic surgery: A narrative review[J]. J Dent, 2022, 119, 104052.
doi: 10.1016/j.jdent.2022.104052 |
| 2 |
Ho CT , Lin HH , Liou EJ , et al. Three-dimensional surgical simulation improves the planning for correction of facial prognathism and asymmetry: A qualitative and quantitative study[J]. Sci Rep, 2017, 7, 40423.
doi: 10.1038/srep40423 |
| 3 | 黄俊强, 黄臻, 伍军, 等. 骨性Ⅲ类错牙合伴下颌偏斜患者下颌支矢状劈开截骨术前后髁突位置的锥形束CT分析[J]. 中华口腔医学杂志, 2019, 54 (10): 649- 655. |
| 4 |
Nunes de Lima V , Faverani LP , Santiago JF Jr , et al. Evaluation of condylar resorption rates after orthognathic surgery in class Ⅱ and Ⅲ dentofacial deformities: A systematic review[J]. J Craniomaxillofac Surg, 2018, 46 (4): 668- 673.
doi: 10.1016/j.jcms.2018.02.002 |
| 5 |
Pachnicz D , Ramos A . Mandibular condyle displacements after orthognathic surgery: An overview of quantitative studies[J]. Quant Imag Med Surg, 2021, 11 (4): 1628- 1650.
doi: 10.21037/qims-20-677 |
| 6 |
Mozzo P , Procacci C , Tacconi A , et al. A new volumetric CT machine for dental imaging based on the cone-beam technique: Preliminary results[J]. Eur Radiol, 1998, 8 (9): 1558- 1564.
doi: 10.1007/s003300050586 |
| 7 |
Wu TY , Lin HH , Lo LJ , et al. Postoperative outcomes of two- and three-dimensional planning in orthognathic surgery: A compa-rative study[J]. J Plast Reconstr Aesthet Surg, 2017, 70 (8): 1101- 1111.
doi: 10.1016/j.bjps.2017.04.012 |
| 8 |
Adolphs N , Haberl EJ , Liu W , et al. Virtual planning for craniomaxillofacial surgery: 7 years of experience[J]. J Craniomaxillofac Surg, 2014, 42 (5): e289- e295.
doi: 10.1016/j.jcms.2013.10.008 |
| 9 |
Kim DS , Choi SC , Lee SS , et al. Principal direction of inertia for 3D trajectories from patient-specific TMJ movement[J]. Comput Biol Med, 2013, 43 (3): 169- 175.
doi: 10.1016/j.compbiomed.2012.12.007 |
| 10 |
Zhang L , Shen L , Zhang L , et al. Dynamic 3D images fusion of the temporomandibular joints: A novel technique[J]. J Dent, 2022, 126, 104286.
doi: 10.1016/j.jdent.2022.104286 |
| 11 |
李源, 刘木清, 刘博, 等. 基于锥形束CT影像的颞下颌关节髁突骨改建三维定量评价研究[J]. 中华口腔医学杂志, 2020, 55 (9): 617- 623.
doi: 10.3760/cma.j.cn112144-20200507-00249 |
| 12 |
Tecco S , Saccucci M , Nucera R , et al. Condylar volume and surface in Caucasian young adult subjects[J]. BMC Med Imaging, 2010, 10, 28.
doi: 10.1186/1471-2342-10-28 |
| 13 | 侯磊, 叶国华, 刘筱菁, 等. 下颌后缩伴颞下颌关节重度骨关节病患者正颌术后颌骨稳定性及髁突体积变化的评价[J]. 北京大学学报(医学版), 2020, 52 (1): 113- 118. |
| 14 | Marlière DAA , Demétrio MS , Schmitt ARM , et al. Accuracy between virtual surgical planning and actual outcomes in orthognathic surgery by iterative closest point algorithm and color maps: A retrospective cohort study[J]. Med Oral Patol Oral, 2019, 24 (2): E243- E253. |
| 15 | 陈硕, 刘筱菁, 李自力, 等. 下颌后缩畸形患者正颌外科术后髁突改建的三维影像评价[J]. 北京大学学报(医学版), 2015, 47 (4): 703- 707. |
| 16 |
Epker BN , Wylie GA . Control of the condylar-proximal mandibular segments after sagittal split osteotomies to advance the mandible[J]. Oral Surg Oral Med Oral Pathol, 1986, 62 (6): 613- 617.
doi: 10.1016/0030-4220(86)90251-3 |
| 17 | Barretto MDA , Melhem-Elias F , Deboni MCZ . Methods of mandibular condyle position and rotation center used for orthognathic surgery planning: A systematic review[J]. J Stomatol Oral Maxi, 2022, 123 (3): 345- 352. |
| 18 |
Costa F , Robiony M , Toro C , et al. Condylar positioning devices for orthognathic surgery: A literature review[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2008, 106 (2): 179- 190.
doi: 10.1016/j.tripleo.2007.11.027 |
| 19 |
Jung GS , Kim TK , Lee JW , et al. The effect of a condylar repositioning plate on condylar position and relapse in two-jaw surgery[J]. Arch Plast Surg, 2017, 44 (1): 19- 25.
doi: 10.5999/aps.2017.44.1.19 |
| 20 |
Bethge LS , Ballon A , Mack M , et al. Intraoperative condyle positioning by sonographic monitoring in orthognathic surgery verified by MRI[J]. J Cranio Maxill Surg, 2015, 43 (1): 71- 80.
doi: 10.1016/j.jcms.2014.10.012 |
| 21 |
Marmulla R , Muhling J . Computer-assisted condyle positioning in orthognathic surgery[J]. J Oral Maxil Surg, 2007, 65 (10): 1963- 1968.
doi: 10.1016/j.joms.2006.11.024 |
| 22 |
Quast A , Santander P , Trautmann J , et al. A new approach in three dimensions to define pre- and intraoperative condyle-fossa relationships in orthognathic surgery: Is there an effect of general anaesthesia on condylar position?[J]. Int J Oral Max Surg, 2020, 49 (10): 1303- 1310.
doi: 10.1016/j.ijom.2020.02.011 |
| 23 |
Oh HJ , Moon JH , Ha H , et al. Virtually-planned orthognathic surgery achieves an accurate condylar position[J]. J Oral Maxillofac Surg, 2021, 79 (5): 1146.e1- 1146.e25.
doi: 10.1016/j.joms.2020.12.048 |
| 24 |
Schouman T , Rouch P , Imholz B , et al. Accuracy evaluation of CAD/CAM generated splints in orthognathic surgery: A cadaveric study[J]. Head Face Med, 2015, 11, 24.
doi: 10.1186/s13005-015-0082-9 |
| 25 |
Ritto FG , Schmitt ARM , Pimentel T , et al. Comparison of the accuracy of maxillary position between conventional model surgery and virtual surgical planning[J]. Int J Oral Maxillofac Surg, 2018, 47 (2): 160- 166.
doi: 10.1016/j.ijom.2017.08.012 |
| 26 |
Kaur A , Rattan V , Rai S , et al. Changes in condylar position after orthognathic surgery and its correlation with temporomandibular symptoms (TMD): A prospective study[J]. J Cranio Maxill Surg, 2022, 50 (12): 915- 922.
doi: 10.1016/j.jcms.2022.12.003 |
| 27 |
Lee SJ , Yang HJ , Choi MH , et al. Real-time augmented model guidance for mandibular proximal segment repositioning in orthognathic surgery, using electromagnetic tracking[J]. J Craniomaxillofac Surg, 2019, 47 (1): 127- 137.
doi: 10.1016/j.jcms.2018.10.016 |
| [1] | 蔡安东,王晓霞,周文娟,柳忠豪. 下颌前突畸形患者上颌骨及髁突虚拟位置与术后现实位置的比较[J]. 北京大学学报(医学版), 2024, 56(1): 74-80. |
| [2] | 李穗,马雯洁,王时敏,丁茜,孙瑶,张磊. 上前牙种植单冠修复体切导的数字化设计正确度[J]. 北京大学学报(医学版), 2024, 56(1): 81-87. |
| [3] | 张雯,刘筱菁,李自力,张益. 基于解剖标志的鼻翼基底缩窄缝合术对正颌患者术后鼻唇部形态的影响[J]. 北京大学学报(医学版), 2023, 55(4): 736-742. |
| [4] | 罗昊,田福聪,王晓燕. 不同椅旁可切削修复材料序列抛光时间及表面粗糙度与光泽度的比较[J]. 北京大学学报(医学版), 2022, 54(3): 565-571. |
| [5] | 冯莎蔚,国慧,王勇,赵一姣,刘鹤. 乳牙数字化参考牙冠模型的初步构建[J]. 北京大学学报(医学版), 2022, 54(2): 327-334. |
| [6] | 李怡,王丽瑜,刘晓强,周倜,吕季喆,谭建国. 不同材料及厚度椅旁CAD/CAM瓷贴面的边缘特征[J]. 北京大学学报(医学版), 2022, 54(1): 140-145. |
| [7] | 邱淑婷,朱玉佳,王时敏,王飞龙,叶红强,赵一姣,刘云松,王勇,周永胜. 姿势微笑位口唇对称参考平面的数字化构建及初步应用验证[J]. 北京大学学报(医学版), 2022, 54(1): 193-199. |
| [8] | 徐啸翔,曹烨,赵一姣,贾璐,谢秋菲. 数字化个齿托盘制取下颌全牙列全冠预备体印模的体外评价[J]. 北京大学学报(医学版), 2021, 53(1): 54-61. |
| [9] | 岳兆国,张海东,杨静文,侯建霞. 数字化评估CAD/CAM个性化基台与成品基台影响粘接剂残留的体外研究[J]. 北京大学学报(医学版), 2021, 53(1): 69-75. |
| [10] | 李峥,柳玉树,王时敏,张瑞,贾璐,叶红强,胡文杰,赵文艳,刘云松,周永胜. 数字化方法复制暂时修复体牙合面形态在重度磨耗病例中的应用[J]. 北京大学学报(医学版), 2021, 53(1): 62-68. |
| [11] | 房硕博,杨广聚,康艳凤,孙玉春,谢秋菲. 数字化辅助确定再定位牙合垫颌位方法的探索和精度评价[J]. 北京大学学报(医学版), 2021, 53(1): 76-82. |
| [12] | 罗佳,张宇,崔宏燕,祝宁,沈惠丹,邸萍,林野. 锥度固位结合数字化技术在后牙连续多牙种植即刻修复中的应用[J]. 北京大学学报(医学版), 2020, 52(5): 964-970. |
| [13] | 魏菱,邹东,陈虎,潘韶霞,孙玉春,周永胜. 一种数字化全口义齿的临床疗效评价[J]. 北京大学学报(医学版), 2020, 52(4): 762-770. |
| [14] | 孙玉春,王勇,邓珂慧,陈虎,李伟伟,赵一姣,潘韶霞,叶红强,周永胜. 功能易适数字化全口义齿的自主创新研发[J]. 北京大学学报(医学版), 2020, 52(2): 390-394. |
| [15] | 游浪,邓珂慧,李伟伟,赵一姣,孙玉春,周永胜. 无牙颌患者鼻唇角变化侧面观的视觉敏感阈值[J]. 北京大学学报(医学版), 2020, 52(1): 107-112. |
|
||