北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (2): 321-326. doi: 10.19723/j.issn.1671-167X.2019.02.023
髓腔内压对树脂水门汀与牙本质粘接强度的影响
- 1. 北京大学口腔医学院·口腔医院,牙体牙髓科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室, 北京 100081;
2. 北京大学口腔医学院·口腔医院第五门诊部, 北京 100020;
Effect of intrapulpal pressure on the bonding strength of resin cement to dentin
Yi-xiang PAN1,Xiu-hua LI2,Fu-cong TIAN3,Xiao-yan WANG1,∆( )
)
- 1. Department of Cariology and Endodontology, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China;
2. Fifth Clinical Division, Peking University School and Hospital of Stomatology, Beijing 100020, China
摘要:
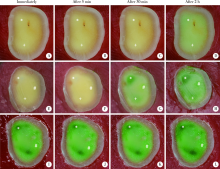
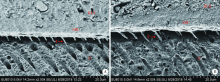
目的: 评价髓腔内压条件对树脂水门汀与牙本质微拉伸粘接强度的影响。方法: 选择新拔除的人无龋第三磨牙30颗分成2组,去除咬合面釉质制备牙本质平面,选取剩余牙本质厚度为0.5~2.5 mm的牙本质试样,在有染料的髓腔内压条件下,观察牙本质表面与牙面处理剂Single Bond Universal(SBU)固化后表面在即刻、5 min、30 min、2 h的染料渗透情况。保持最小剩余牙本质厚度为(1.0±0.1) mm,分别在有或无髓腔内压条件(15或0 cmH2O,1 cmH2O=0.098 kPa)下维持30 min,使用SBU并光照固化,然后使用模具在牙本质表面堆塑RelyX Ultimate(RLX)树脂水门汀(直径10 mm,高4 mm),制备牙本质-树脂水门汀粘接试样。试样在37 ℃蒸馏水中储存24 h后,将牙本质-树脂水门汀试样垂直于粘接界面切割形成横截面积为0.9 mm×0.9 mm条状试样,使用微拉伸测试仪测试计算其粘接强度(两独立样本t检验,双侧检验水平α=0.05),用扫描电镜观察统计试样断裂类型(Fisher精确检验,双侧检验水平α=0.05)。将牙本质-树脂水门汀试样垂直粘接界面做切片,厚度0.8 mm,扫描电镜下观察粘接界面形貌。结果: 在髓腔内压条件下,随时间延长,粘接表面染料渗出增加。有髓腔内压时和无髓腔内压时RLX与牙本质微拉伸粘接强度分别为:(26.26±9.78) MPa和(28.70±9.09) MPa,两者差异无统计学意义(P>0.05)。两组试样断裂类型无明显差异(P>0.05),都以混合断裂为主。两组试样粘接界面可见4~8 μm指状树脂突,分布及长短较均匀,形貌无明显差异。结论: SBU预处理牙本质后,髓腔内压不影响树脂水门汀RLX的即刻牙本质粘接强度。
中图分类号:
- R783.1
| [1] | 林红 . 口腔材料学[M]. 2版. 北京: 北京大学医学出版社, 2013: 193-196. |
| [2] |
Kawano S, Fu J, Saikaew P , et al. Microtensile bond strength of a newly developed resin cement to dentin[J]. Dent Mater J, 2015,34(1):61-69.
doi: 10.4012/dmj.2014-122 |
| [3] |
André CB, Aguiar TR, Ayres AP , et al. Bond strength of self-adhesive resin cements to dry and moist dentin[J]. Braz Oral Res, 2013,27(5):389-395.
doi: 10.1590/S1806-83242013000500002 |
| [4] |
Cardoso MV, Moretto SG, Carvalho RC , et al. Influence of intrapulpal pressure simulation on the bond strength of adhesive systems to dentin[J]. Braz Oral Res, 2008,22(2):170-175.
doi: 10.1590/S1806-83242008000200013 |
| [5] |
Feitosa VP, Gotti VB, Grohmann CV , et al. Two methods to si-mulate intrapulpal pressure: effects upon bonding performance of self-etch adhesives[J]. Int Endod J, 2014,47(9):819-826.
doi: 10.1111/iej.2014.47.issue-9 |
| [6] | Flury S, Peutzfeldt A, Schmidlin PR , et al. Exposed dentin: Influence of cleaning procedures and simulated pulpal pressure on bond strength of a universal adhesive system[J]. PLoS One, 2017,12(1):e169680. |
| [7] |
Hiraishi N, Yiu CK, King NM , et al. Effect of pulpal pressure on the microtensile bond strength of luting resin cements to human dentin[J]. Dent Mater, 2009,25(1):58-66.
doi: 10.1016/j.dental.2008.05.005 |
| [8] |
Mazzitilli C, Monticelli F, Toledano M , et al. Dentin treatment effects on the bonding performance of self-adhesive resin cements[J]. Eur J Oral Sci, 2010,118(1):80-86.
doi: 10.1111/eos.2010.118.issue-1 |
| [9] |
Mohamed MF, El Deeb HA, Gomaa IE , et al. Bond durability of different resin cements to caries-affected dentin under simulated intrapulpal pressure[J]. Oper Dent, 2015,40(3):293-303.
doi: 10.2341/14-035-L |
| [10] |
Moosavi H, Hariri I, Sadr A , et al. Effects of curing mode and moisture on nanoindentation mechanical properties and bonding of a self-adhesive resin cement to pulp chamber floor[J]. Dent Mater, 2013,29(6):708-717.
doi: 10.1016/j.dental.2013.03.020 |
| [11] |
Souza GD, Braga RR, Cesar PF , et al. Correlation between clinical performance and degree of conversion of resin cements: a lite-rature review[J]. J Appl Oral Sci, 2015,23(4):358-368.
doi: 10.1590/1678-775720140524 |
| [12] | 傅昭然, 田福聪, 张路 , 等. 通用型粘接剂对双固化树脂水门汀牙本质粘接强度的影响[J]. 北京大学学报(医学版), 2017,49(1):101-104. |
| [13] | Bakry AS, Nakajima M, Otsuki M , et al. Effect of Er:YAG laser on dentin bonding durability under simulated pulpal pressure[J]. J Adhes Dent, 2009,11(5):361-368. |
| [14] |
Krejci I, Häusler T, Sägesser , et al. New adhesives in class V restorations under combined load and simulated dentinal fluid[J]. Dent Mater, 1994,10(5):331-335.
doi: 10.1016/0109-5641(94)90042-6 |
| [15] | 高学军, 岳林 . 牙体牙髓病学[M]. 2版. 北京: 北京大学医学出版社, 2013: 31-32. |
| [16] | Shaymma M . Durability of solvent-free one-step self-etch adhesive under simulated intrapulpal pressure[J]. J Clin Exp Dent, 2015,7(4):e466-e470. |
| [17] |
Acar O, Erkut S, Lakshmipathy M . Surface detail reproduction under simulated pulpal pressure: a 3-dimensional optical profilometer and scanning electron microscopy evaluation[J]. J Prosthet Dent, 2012,108(2):102-113.
doi: 10.1016/S0022-3913(12)60116-4 |
| [18] | 关天燕, 张彦博, 陈国常 , 等. 模拟髓室压力对两种自酸蚀粘接剂牙本质粘接强度的影响[J]. 口腔疾病防治, 2011,19(10):516-519. |
| [19] |
Tay FR, Gwinnett JA, Wei SH . The overwet phenomenon in two-component acetone-based primers containing aryl amine and carboxylic acid monomers[J]. Dent Mater, 1997,13(2):118-127.
doi: 10.1016/S0109-5641(97)80021-8 |
| [20] |
Wagner A, Wendler M, Petschelt A , et al. Bonding performance of universal adhesives in different etching modes[J]. J Dent, 2014,42(7):800-807.
doi: 10.1016/j.jdent.2014.04.012 |
| [21] |
Kim HJ, Bagheri R, Kim YK , et al. Influence of curing mode on the surface energy and sorption/solubility of dental self-adhesive resin cements[J]. Materials (Basel), 2017,10(2):129-130.
doi: 10.3390/ma10020129 |
| [22] | Mobarak EH, El-Deeb HA, Yousry MM . Influence of different intrapulpal pressure simulation liquids on the microtensile bond strength of adhesive systems to dentin[J]. J Adhes Dent, 2013,15(6):519-526. |
| [1] | 仲若情,朱梦倩,李应龙,潘洁. 低温等离子体对牙本质小管内粪肠球菌的抗菌效果[J]. 北京大学学报(医学版), 2023, 55(1): 38-43. |
| [2] | 郭若兰,黄桂彬,龙赟子,董艳梅. 新型生物活性玻璃促进人工牙本质龋再矿化的作用[J]. 北京大学学报(医学版), 2023, 55(1): 82-87. |
| [3] | 马欣蓉,朱晓鸣,李静,李德利,李和平,谭建国. 新型大气压冷等离子体射流处理对牙本质胶原纤维交联化的影响[J]. 北京大学学报(医学版), 2022, 54(1): 83-88. |
| [4] | 骆池怡,彭楚芳,杨媛,秦满,王媛媛. 3种自酸蚀粘接系统和轻度唾液污染对乳牙釉质及牙本质粘接耐久性的影响[J]. 北京大学学报(医学版), 2021, 53(1): 46-53. |
| [5] | 陈文新,包旭东,岳林. 固化方式对树脂水门汀氧阻聚层形成的影响[J]. 北京大学学报(医学版), 2020, 52(6): 1117-1123. |
| [6] | 李秋菊,宫玮玉,董艳梅. 生物活性玻璃预处理对牙本质粘接界面耐久性的影响[J]. 北京大学学报(医学版), 2020, 52(5): 931-937. |
| [7] | 李芳,刘洋,刘浩辰,冯海兰. 乳光牙本质患者的基因变异分析及患牙的组织学观察[J]. 北京大学学报(医学版), 2018, 50(4): 666-671. |
| [8] | 廖宇,刘晓强,陈立,周建锋,谭建国. 不同表面处理方法对氧化锆与树脂水门汀粘接强度的影响[J]. 北京大学学报(医学版), 2018, 50(1): 53-57. |
| [9] | 臧海玲,王月,梁宇红. 有机溶剂对牙本质表面残留根管封闭剂的清除效果[J]. 北京大学学报(医学版), 2018, 50(1): 63-68. |
| [10] | 贾维茜,赵玉鸣,葛立宏. 人重组转化生长因子β1促进牙髓干细胞的增殖和矿化[J]. 北京大学学报(医学版), 2017, 49(4): 680-681. |
| [11] | 李皓,刘玉华,罗志强. 生物活性玻璃用于缓解活髓牙全冠预备后敏感的效果评价[J]. 北京大学学报(医学版), 2017, 49(4): 709-713. |
| [12] | 信义,王赛楠,崔彩云,董艳梅. 生物活性玻璃和牙本质浸提蛋白对人牙髓细胞的作用[J]. 北京大学学报(医学版), 2017, 49(2): 331-336. |
| [13] | 郭惠杰,高承志, 林斐,刘伟,岳林. 唾液污染对复合树脂间粘接强度的影响[J]. 北京大学学报(医学版), 2017, 49(1): 96-100. |
| [14] | 傅昭然,田福聪,张路,韩冰,王晓燕. 通用型粘接剂对双固化树脂水门汀牙本质粘接强度的影响[J]. 北京大学学报(医学版), 2017, 49(1): 101-104. |
| [15] | 王月,梁宇红. 次氯酸钠溶液表面处理对牙本质粘接强度的影响[J]. 北京大学学报(医学版), 2017, 49(1): 105-109. |
|
||